Abstract
Background
Recently, in addition to multi-drug resistant tuberculosis (MDR-TB), extensively drug-resistant tuberculosis (XDR-TB) has become rapidly growing public health threat. This study examined the clinical differences between pulmonary TB patients with extensively drug resistance (XDR) and multi-drug resistance (MDR) at the National Medical Center in Korea in order to determine the clinical characteristics associated more with XDR-TB than MDR-TB.
Methods
Patients who received a diagnosis of culture-confirmed pulmonary TB and a drug sensitivity test (DST) for anti-TB drugs at the National Medical Center between January 2000 and August 2007 were enrolled in this study. The patients were identified into the XDR-TB or MDR-TB group according to the DST results. The clinical characteristics were reviewed retrospectively from the medical records. Statistical analysis for the comparisons was performed using a χ2-test, independent samples t-test or binary logistic regression where appropriate.
Results
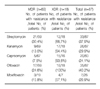
A total 314 patients with culture-confirmed pulmonary TB were included. Among them, 18 patients (5.7%) had XDR-TB and 69 patients (22%) had MDR-TB excluding XDR-TB. A comparison of the clinical characteristics, revealed the XDR-TB group to have a higher frequency of a prior pulmonary resection for the treatment of TB (odds ratio [OR], 3.974; 95% confidence interval [CI], 1.052~15.011; P value 0.032) and longer average previous treatment duration with anti-TB drugs, including a treatment interruption period prior to the diagnosis of XDR, than the MDR-TB group (XDR-TB group, 72.67 months; MDR-TB group, 13.09 months; average treatment duration difference between two groups, 59.582 months; 95% CI, 31.743~87.420; P value, 0.000). In addition, a longer previous treatment duration with anti-TB drugs was significantly associated with XDR-TB (OR, 1.076; 95% CI, 1.038~1.117; P value, 0.000). A comparison of the other clinical characteristics revealed the XDR-TB group to have a higher frequency of male gender, diabetes mellitus (DM), age under 45, treatment interruption history, cavitations on simple chest radiograph and positive result of sputum AFB staining at the time of diagnosis of XDR. However, the association was not statistically significant.
References
1. Centers for Disease Control and Prevention. Notice to readers: revised definition of extensively drug-resistant tuberculosis. MMWR Morb Mortal Wkly Rep. 2006. 55:1176.
2. Dukes Hamilton C, Sterling TR, Blumberg HM, Leonard M, McAuley J, Schlossberg D, et al. Extensively drug-resistant tuberculosis: are we learning from history or repeating it? Clin Infect Dis. 2007. 45:338–342.
3. Centers for disease control and prevention. Emergence of Mycobacterium tuberculosis with extensive resistance to second-line drugs-worldwide, 2000~2004. MMWR Morb Mortal Wkly Rep. 2006. 55:301–305.
4. Raviglione M. XDR-TB: entering the post-antibiotic era? Int J Tuberc Lung Dis. 2006. 10:1185–1187.
5. Gandhi NR, Moll A, Sturm AW, Pawinski R, Govender T, Lalloo U, et al. Extensively drug resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet. 2006. 368:1575–1580.
6. Kim HR, Hwang SS, Kim HJ, Lee SM, Yoo CG, Kim YW, et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007. 45:1290–1295.
7. Kang YA, Choi YJ, Cho YJ, Lee SM, Yoo CG, Kim YW, et al. Cost of treatment for multidrug-resistant tuberculosis in South Korea. Respirology. 2006. 11:793–798.
8. Iseman MD. Treatment of multidrug-resistant tuberculosis. N Engl J Med. 1993. 329:784–791.
9. Colebunders R, Apers L, Shamputa IC. Treatment of multidrug-resistant tuberculosis. Lancet. 2004. 363:1240.
10. Choi JC, Lim SY, Suh GY, Chung MP, Kim HJ, Kwon OJ, et al. Drug resistance rates of Mycobacterium tuberculosis at a private referral center in Korea. J Korean Med Sci. 2007. 22:677–681.
11. Arevalo M, Solera J, Cebrian D, Bartolome J, Robles P. Risk factors associated with drug-resistant Mycobacterium tuberculosis in Castilla-la-Mancha (Spain). Eur Respir J. 1996. 9:274–278.
12. Ruddy M, Balabanova Y, Graham C, Fedorin I, Malomanova N, Elisarova E, et al. Rates of drug resistance and risk factor analysis in civilian and prison patients with tuberculosis in Samara Region, Russia. Thorax. 2005. 60:130–135.
13. Faustini A, Hall AJ, Perucci CA. Risk factors for multi-drug resistant tuberculosis in Europe: a systematic review. Thorax. 2006. 61:158–163.
14. Djuretic T, Herbert J, Drobniewski F, Yates M, Smith EG, Magee JG, et al. Antibiotic resistant tuberculosis in the United Kingdom: 1993~1999. Thorax. 2002. 57:477–482.
15. Kordy FN, Al-Thawadi S, Alrajhi AA. Drug resistance patterns of Mycobacterium tuberculosis in Riyadh, Saudi Arabia. Int J Tuberc Lung Dis. 2004. 8:1007–1011.
16. Harrow EM, Rangel JM, Arriega JM, Cohen I, Regil Ruiz MI, DeRiemer K, et al. Epidemiology and clinical consequences of drug-resistant tuberculosis in a Guatemalan hospital. Chest. 1998. 113:1452–1458.
17. Sharma SK, Turaga KK, Balamurugan A, Saha PK, Pandey RM, Jain NK, et al. Clinical and genetic risk factors for the development of multi-drug resistant tuberculosis in non-HIV infected patients at a tertiary care center in India: a case-control study. Infect Genet Evol. 2003. 3:183–188.
18. Jeon CY, Hwang SH, Min JH, Prevots DR, Goldfeder LC, Lee H, et al. Extensively drug-resistant tuberculosis in South Korea: risk factors and treatment outcomes among patients at a tertiary referral hospital. Clin Infect Dis. 2008. 46:42–49.
19. Kim HJ, Kang CH, Kim YT, Sung SW, Kim JH, Lee SM, et al. Prognostic factors for surgical resection in patients with multidrug-resistant tuberculosis. Eur Respir J. 2006. 28:576–580.
20. Leimane V, Riekstina V, Holtz TH, Zarovska E, Skripconoka V, Thorpe LE, et al. Clinical outcome of individualised treatment of multidrug-resistant tuberculosis in Latvia: a retrospective cohort study. Lancet. 2005. 365:318–326.
21. Yew WW, Chan CK, Chau CH, Tam CM, Leung CC, Wong PC, et al. Outcomes of patients with multidrug-resistant pulmonary tuberculosis treated with ofloxacin/levofloxacin-containing regimens. Chest. 2000. 117:744–751.
22. World Health Organization. Guidelines for the programmatic management of drug-resistant pulmonary tuberculosis. 2006. Geneva: World Health Organization.
23. Caminero JA. Management of multidrug-resistant tuberculosis and patients in retreatment. Eur Respir J. 2005. 25:928–936.
24. Mukherjee JS, Rich ML, Socci AR, Joseph JK, Virú FA, Shin SS, et al. Programmes and principles in treatment of multidrug-resistant tuberculosis. Lancet. 2004. 363:474–481.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download