Abstract
We report the patient presented with a left-sided pleural effusion. Pleural fluid analysis revealed lymphocyte-dominant exudates with lower level of adenosine deaminase and negative cytologic malignancy. Thoracoscopic examination and histologic examination revealed metastatic nodules on pleurae, proven to be from the papillary thyroid cancer. There were no other sites of distant metastases. Though papillary thyroid cancer is characterized with slow progression and relatively good prognosis, metastatic pleural effusion as an initial manifestation of undiagnosed papillary thyroid cancer can be considered.
Papillary thyroid cancer (PTC) is the most common kind of thyroid cancer and the clinical outcomes for patients with PTC are excellent because of an indolent clinical course and a favorable prognosis1,2. It has been diagnosed increasingly in the subclincal phase as a result of frequent use of ultrasound imaging and surveillance2. Since PTC is diagnosed in relatively early stage and usually tends to advance locally to regional lymph nodes, distant metastases are rare. The lungs and bone are common sites of metastases, but most of these metastases occur after initial treatment of thyroid cancer. Only approximately 4% of patients presented initially with distant metastasis in well-differentiated thyroid cancer3. Moreover, metastatic pleural effusion by itself, as the initial manifestation of papillary thyroid cancer, is infrequent4.
We report here a 47-year-old male who presented with shortness of breath and pleuritic chest pain induced by left-sided pleural effusion, and diagnosed as metastatic papillary thyroid cancer to the pleura.
A 47-year-old man presented with 3-week history of worsening shortness of breath and left-sided pleuritic chest pain. His medical history was unremarkable. He was a current smoker of total 15 pack-years. On review of symptoms, he denied fever, night sweating, or weight loss. On physical examination, he was afebrile and complained of shortness of breath. Examination of the neck demonstrated no palpable nodules and chest auscultation revealed diminished breathing sound over the left lower lung field. The others were unremarkable. Simple chest radiography showed a pleural effusion in the left hemithorax (Figure 1A).
Diagnostic thoracentesis revealed clear, amber-colored pleural fluid with protein concentration of 5.4 mg/dl and lactate dehydrogenase concentration of 69 IU/L. The serum total protein and lactate dehydrogenase measured on the same day were 7.8 mg/dl and 510 IU/L, respectively. The total leukocyte count of pleural fluid was 1,760/mm3, and this consisted of 80% lymphocytes and 20% polymorphonuclear leukocytes. The overall nature of the pleural effusion was lymphocyte-dominant exudate. The adenosine deaminase (ADA) level was 16.4 U/L and the polymerase chain reaction (PCR) was negative for Mycobacterium tuberculosis. The staining for acid-fast bacilli was also negative. The glucose concentration was 89 mg/dl and gram staining showed no bacteria. Repeated cytologic analyses of the pleural effusion revealed no evidence of malignancy. To evaluate the underlying cause such as malignancy, computed tomography (CT) of the chest (Figure 1B) and flexible fiberoptic bronchoscopy were performed. Low attenuated, round-shaped small nodule on the right lobe of the thyroid was suspected and a large amount of effusion was noted on chest CT.
Thoracoscopic examination showed multiple small nodular patchy lesions on the diaphragmatic, para-aortic, visceral, and parietal pleura (Figure 2A). The histopathology of these nodular lesions revealed metastatic carcinoma with psammoma bodies (Figure 2B). Immunohistochemical stains were positive for thyroid transcription-factor 1 (TTF-1) and cytokeratin 7, which strongly suggested thyroid cancer as the primary tumor1. Then ultrasonography of the thyroid was performed, revealing a hyperechoic, 12-mm oval cystic nodule with peripheral solid components on the right side of the isthmus. Thyroid function test revealed TSH 1.88 mU/L (0.17~4.05 mU/L), free T4 1.51 ng/dl (0.79~1.86 ng/dl), thyroglobulin 157 ng/ml (0~30 ng/ml). Fine needle aspiration on cystic nodule of thyroid was performed with the result of possible papillary carcinoma. Consequently, he was diagnosed as PTC with metastatic pleural effusion. Total thyroidectomy and cervical lymph node dissection were performed and final pathology confirmed a papillary carcinoma measuring 0.7×0.6×0.8 cm. The tumor involved only the right lobe and did not extend to the surgical margins grossly and microscopically. 9 of 55 perithyroidal lymph nodes were positive for metastatic papillary thyroid cancer. Two months later, 131I radioablation therapy was followed.
Pleural effusion is commonly encountered medical problem and manifestation of a wide range of diseases5. A structured approach to the investigation of the patient with a pleural effusion could allow an accurate diagnosis. Pleural fluid analysis is the most useful test in differentiating possible causes and directing further investigations6.
Tuberculous pleurisy was initially suspected in this patient as the cause of the unilateral pleural effusion showing the nature of lymphocyte-dominant exudates, considering the high incidence of tuberculous pleurisy in Korea7. However, the likelihood of tuberculous pleurisy as the cause of the pleural effusion decreased, because of the negative acid-fast bacilli smear, the lower level of ADA, and the negative PCR for M. tuberculosis of pleural fluid8.
Subsequently, a presumed diagnosis of malignant pleural effusion was made. Malignancy is one of the most common causes of an exudative pleural effusion in elderly patients. The common causes of malignant pleural effusion are metastases from a primary cancer of the lung, breast, or lymphoma6. However, there were no evidences of other pulmonary or systemic disease, even after chest CT and bronchoscopic examination.
Though low attenuated, round-shaped nodule on the right lobe of the thyroid was suspected on chest CT, it was considered as benign nodule. The possibility of thyroid cancer as a cause of malignant effusion was not initially suspected. After histopathology of nodular lesions on pleura verified the metastatic papillary carcinoma, thyroid gland was reexamined carefully by ultrasonography.
Papillary thyroid cancer is the most common type of thyroid cancer. Most papillary thyroid cancers present as an asymptomatic thyroid nodule, and are diagnosed in the early stages, with an excellent prognosis and expected survival. Distant metastases from papillary thyroid cancer are rare and are associated with a poor prognosis1. 19 patients (2.3%) presented with distant metastases in 810 patients presenting with papillary thyroid cancer3. It is difficult to suspect papillary thyroid cancer as the primary tumor in the differential diagnosis of malignant pleural effusion. Malignant pleural effusion as a manifestation of distant metastasis is rare and diagnosis of papillary thyroid cancer often precedes the occurrence of malignant pleural effusion4. In retrospective report from the MD Anderson Cancer Center, 10 patients (0.6%) had malignant pleural effusion that developed during the course of papillary thyroid cancer among 1,772 patients. Moreover, all patients had radiologically apparent lung metastases at the time pleural effusion was found9.
Furthermore, papillary thyroid cancer, initially presenting as a pleural effusion before diagnosis is made is very infrequent. In a reported case of pleural effusion resulting from metastatic thyroid cancer, the patient had already been diagnosed with papillary thyroid cancer a few years earlier4. The pleural effusion developed during the course of the disease and was merely a recurrent complication. By contrast, our patient presented with a pleural effusion before being diagnosed with papillary thyroid cancer.
In conclusion, malignant metastatic pleural effusion from papillary thyroid cancer is very rare. Nevertheless, the possibility of malignant metastatic pleural effusion from papillary thyroid cancer deserves consideration in the differential diagnosis of an exudative, lymphocyte-dominant pleural effusion.
Figures and Tables
Figure 1
Chest radiograph on the day of admission showed a left pleural effusion (A). Contrast-enhanced chest computed tomography showed a left-sided, unilateral pleural effusion, and collapse of the left lung with no pathologic endobronchial mass or lymphadenopathy (B).
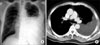
Figure 2
Thoracoscopic examination revealed small multiple patchy lesions on the diaphragmatic pleura (A). Histology of the pleural metastasis showed papillary proliferation of atypical cells and complex and branching papillae with a central fibrovascular core (B, hematoxylin and eosin stain, ×200).

References
1. Schlumberger MJ. Papillary and follicular thyroid carcinoma. N Engl J Med. 1998. 338:297–306.
2. Sosa JA, Udelsman R. Papillary thyroid cancer. Surg Oncol Clin N Am. 2006. 15:585–601.
3. Shaha AR, Shah JP, Loree TR. Differentiated thyroid cancer presenting initially with distant metastasis. Am J Surg. 1997. 174:474–476.
4. Vernon AN, Sheeler LR, Biscotti CV, Stoller JK. Pleural effusion resulting from metastatic papillary carcinoma of the thyroid. Chest. 1992. 101:1448–1450.
5. Medford A, Maskell N. Pleural effusion. Postgrad Med J. 2005. 81:702–710.
6. Rahman NM, Chapman SJ, Davies RJ. Pleural effusion: a structured approach to care. Br Med Bull. 2004. 72:31–47.
7. Kim NJ, Hong SC, Kim JO, Suhr JW, Kim SY, Ro HK. Etiologic considerations of nonspecific pleuritis. Korean J Intern Med. 1991. 6:58–63.
8. Laniado-Laborin R. Adenosine deaminase in the diagnosis of tuberculous pleural effusion: is it really an ideal test? A word of caution. Chest. 2005. 127:417–418.
9. Vassilopoulou-Sellin R, Sneige N. Pleural effusion in patients with differentiated papillary thyroid cancer. South Med J. 1994. 87:1111–1116.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download