Abstract
Pheochromocytoma is derived from the chromaffin tissue. The typical finding of pheochromocytoma is paroxysmal hypertension accompanied with various signs and symptoms that are due to the excess of catecholamines or other bioactive substances. Yet the diagnosis is sometimes difficult to make because its clinical presentation is quite variable. Especially, hemoptysis is a very rare symptom, so the diagnosis is often missed or delayed. Without making the correct diagnosis and then subsequently administering treatment, the condition may be fatal. We herein report on a 68 year-old woman who was admitted because of abdominal pain and hemoptysis. The initial radiologic findings suggested pulmonary edema with alveolar hemorrhage. The urine catecholamine levels were elevated and she developed catecholamine-induced cardiomyopathy. We performed bronchial arterial embolization and we administered alpha blocker medication for controlling the hemoptysis and hypertension. After the temporary symptomatic improvement, her clinical course was aggravated by pneumonia and pulmonary edema. In spite of performing definitive surgery for pheochromocytoma, she died of postoperative hemodynamic instability.
Figures and Tables
Figure 1
Chest X-ray (A) and chest CT (B) shows patchy and geographic air-space fillings in the both lungs. This findings are suggestive of pulmonary edema combined with diffuse alveolar hemorrhage.

Figure 2
Abdomen CT reveals an about 3.5×3.3 cm-sized well defined heterogeneously enhanced mass (arrow) in right adrenal gland. It was heterogeneously enhanced with central hypodense area.
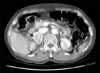
Figure 3
Echocardiography on 3rd admission day (A, B) shows hyperkinesia on mid ventricular wall and apical ballooning on systolic phase. After 1 week treatment, follow up echocardiography (C, D) shows good systolic function with no regional wall motion abnormality.

Figure 4
Tumor is composed of well defined tumor cell nest (Zellballen) bounded by a delicate fibrovascular stroma. The cells are variable in size and shape and have a finely granular basophilic cytoplasm with round to ovoid nucleoli (A, H&E stain, ×100). In immunohistochemical stain, the tumor cells are positive to chromogranin (B, chromogranin stain, ×100).

References
1. Kizer JR, Koniaris LS, Edelman JD, St John Sutton MG. Pheochrocytoma crisis, cardiomyopathy, and hemodynamic collapse. Chest. 2000. 118:1221–1223.
2. Wu GY, Doshi AA, Haas GJ. Pheochromocytoma induced cardiogenic shock with rapid recovery of ventricular function. Eur J Heart Fail. 2007. 9:212–214.
3. Frymoyer PA, Anderson GH Jr, Blair DC. Hemoptysis as a presenting symptom of pheochromocytoma. J Clin Hypertens. 1986. 2:65–67.
4. Jung YS, Kim JG, Song SK, Kwon SK, Choi YS, Jang TW, et al. A case of pheochromocytoma accompanied with hemoptysis. Kosin Med J. 2000. 15:103–107.
5. Iino S, Nagashima N, Akiba H, Ban Ymiyamoto M. Hemoptysis and palpitation (with hypertension): pheochromocytoma. Nippon Rinsho. 1975. Spec No:918–919. 1394–1395.
6. Joshi R, Manni A. Pheochromocytoma manifested as noncardiogenic pulmonary edema. South Med J. 1993. 86:826–828.
7. Takeshita T, Shima H, Oishi S, Machida N, Uchiyama K. Noncardiogenic pulmonary edema as the first manifestation of pheochromocytoma. Radiat Med. 2005. 23:133–138.
8. Gatzoulis KA, Tolis G, Theopistou A, Gialafos JH, Toutouzas PK. Cardiomyopathy due to a pheochromocytoma. A reversible entity. Acta Cardiol. 1998. 53:227–229.
9. Minno AM, Bennett WA, Kvale WF. Pheochromocytoma: a study of 15 cases diagnosed at autopsy. N Engl J Med. 1954. 251:959–965.
10. de Graeff , Muller H, Moolenaar AJ. Pheochromocytoma: a report of seven cases. Acta Med Scand. 1959. 164:419–430.
11. Kimura Y, Ozawa H, Igarashi M, Iwamoto T, Nishiya K, Urano T, et al. A pheochromocytoma causing limited coagulopathy with hemoptysis. Tokai J Exp Clin Med. 2005. 30:35–39.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download