Abstract
Background
It is not known with certainty whether patients with persistently positive sputum smear results who have also had negative sputum culture results require prolongation of treatment for tuberculosis in order to avoid an increased risk of eventual relapse. The purpose of the present study was to retrospectively describe the treatment characteristics and evaluate the appropriate duration of treatment in these patients.
Methods
Sixty of 69 patients with sputum smear positive and culture negative tests at 5 months after first line anti-tuberculous chemotherapy from 2002 to 2003 were retrospectively analyzed. Exclusion criteria included incomplete treatment or resistance to rifampicin or two additional antibiotics, as determined by a drug susceptibility test (DST).
Results
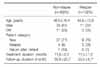
Smear conversion of the study subjects was observed after 8.3±2.3 months treatment, and the patients were culture negative after 2.0±0.8 months. The relapse rates of the study subjects were 3.8, 10.0, and 25.8% after 1, 2, and 5 years of anti-tuberculosis chemotherapy, respectively. The relapse rates were not significantly affected by a series of risk factors such as age, sex, presence of diabetes, a sputum culture examination after 2 months treatment, previous treatment history, chest radiograph, and duration of the treatment (p>0.05).
Figures and Tables
References
1. British Thoracic Association. A controlled trial of six months chemotherapy in pulmonary tuberculosis. First report: results during chemotherapy. Br J Dis Chest. 1981. 75:141–153.
2. Korea Center for Disease Control & Prevention. 2007 Tuberculosis. 2007. Seoul: Korea Center for Disease Control & Prevention.
3. Kim TC, Blackman RS, Heatwole KM, Kim T, Rochester DF. Acid-fast bacilli in sputum smears of patients with pulmonary tuberculosis. Am Rev Respir Dis. 1984. 129:264–268.
4. Al-Moamary MS, Black W, Bessuille E, Elwood RK, Vedal S. The significance of the persistent presence of acid-fast bacilli in sputum smears in pulmonary tuberculosis. Chest. 1999. 116:726–731.
5. Vidal R, Martin-Casabona N, Juan A, Falgueras T, Miravitlles M. Incidence and significance of acid fast bacilli in sputum smears at the end of antituberculous treatment. Chest. 1996. 109:1562–1565.
6. Sundaram V, Fujiwara PI, Driver CR, Osahan SS, Munsiff SS. Yield of continued monthly sputum evaluation among tuberculosis patients after culture conversion. Int J Tuberc Lung Dis. 2002. 6:238–245.
7. National Tuberculosis Association of the USA. Diagnostic standards and classification of tuberculosis. 1961. New York: National Tuberculosis Association.
8. Veen J, Raviglione M, Rieder HL, Migliori GB, Graf P, Grzemska M, et al. Standardized tuberculosis treatment outcome monitoring in Europe. Eur Respir J. 1998. 12:505–510. Recommendations of a Working Group of the World Health Organization (WHO) and the European Region of the International Union Against Tuberculosis and Lung Disease (IUATLD) for uniform reporting by cohort analysis of treatment outcome in tuberculosis patients.
9. Guler M, Unsal E, Dursun B, Aydln O, Capan N. Factors influencing sputum smear and culture conversion time among patients with new case pulmonary tuberculosis. Int J Clin Pract. 2007. 61:231–235.
10. Chang SC, Yoon YM, Hong YP. Relapse rates within one year after the completion of treatment with short course chemotherapy for pulmonary tuberculosis under programme conditions. Tuberc Respir Dis. 1987. 34:137–143.
11. Frieden T. Toman's Tuberculosis: case detection, treatment, and monitoring - questions and answers. 2004. 2nd ed. Geneva: World Health Organization.
12. Panjabi R, Comstock GW, Golub JE. Recurrent tuberculosis and its risk factors: adequately treated patients are still at high risk. Int J Tuberc Lung Dis. 2007. 11:828–837.
13. Verver S, Warren RM, Beyers N, Richardson M, van der Spuy GD, Borgdorff MW, et al. Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med. 2005. 171:1430–1435.
14. Tam CM, Chan SL, Kam KM, Goodall RL, Mitchison DA. Rifapentine and isoniazid in the continuation phase of a 6-month regimen. Final report at 5 years: prognostic value of various measures. Int J Tuberc Lung Dis. 2002. 6:3–10.
15. Ormerod LP, Horsfield N, Green RM. Can a nine-month regimen be used to treat isoniazid resistant tuberculosis diagnosed after standard treatment is started? J Infect. 2001. 42:1–3.
16. Koh WJ, Kwon OJ, Yu CM, Jeon K, Kim KC, Lee BH, et al. Treatment of isoniazid-resistant pulmonary tuberculosis. Tuberc Respir Dis. 2004. 56:248–260.
17. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download