Abstract
Background
Malignancies are a common and important causes of exudative pleural effusions. Several tumor markers have been studied because the pleural fluid cytology and pleural biopsy specimens do not provide a diagnosis in a high percentage of malignant effusions. In an attempt to overcome this limitation, procalcitonin and C-reactive protein (CRP) in pleural effusions and serum, which are known to be inflammation markers, were measured to determine if they can differentiate an exudate from trasndate as well as the diverse causes of exudative pleural effusion.
Methods
178 consecutive patients with pleural effusion (malignant 57, tuberculous 51, parapneumonic 31, empyema 5, miscellaneous benign 7, transudative 27)were studied prospectively. The standard parameters of pleural effusion and measured serum and pleural procalcitonin were examined using in immunoluminometric assay. The level of CRP in serum and pleural fluid was determined by turbidimetric immunoassay.
Results
The pleural procalcitonin levels in the exudate were significantly higher than those in the transudate, 0.81±3.09 ng/mL and 0.12±0.12 ng/mL, respectively (p=0.007). The pleural CRP levels were significantly higher in the exudate than the transudate, 2.83±3.31 mg/dL and 0.74±0.67 mg/dL, respectively (p<0.001). The pleural procalcitonin levels in the benign effusion were significantly higher than those in the malignant effusion, 1.15±3.82 ng/mL and 0.25±0.92 ng/mL, respectively (p=0.032). The pleural CRP levels were significantly higher in the benign effusion than in the malignant effusion, 3.68±3.78 mg/dL and 1.42±1.54 mg/dL, respectively (p<0.001). The pleural procalcitonin levels in the non-tuberculous effusion were significantly higher than those in the tuberculous effusion, 1.16±3.75 ng/mL and 0.13±0.37 ng/mL, respectively (p=0.008).
Figures and Tables
Figure 1
Receiver operating characteristic curve of pleural fluid C-reactive protein (CRP) concentrations for discriminating exudate from transudate. The area under the curve value was 0.752 (p=0.0001). Specificity and sensitivity value for pleural fluid CRP were 96.3% and 45.0% at the 2.06 mg/dL cut-off value.
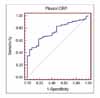
Figure 2
Receiver operating characteristic curves of pleural fluid C-reactive protein (CRP) and procalcitonin (PCT) concentrations for discriminating benign effusions from malignant effusions. The area under the curve values were 0.729 and 0.591, respectively. Specificity and sensitivity values for pleural fluid CRP and PCT were 86.0% and 53.2%, and 84.2% and 40.4% at the 2.28 mg/dL and 0.11 ng/mL cut-off values, respectively.

Table 1
Pleural leukocyte count, protein, LDH, ADA, ADA2, procalcitonin (PCT), and CRP in patients with pleural effusion

References
1. Romero S, Fernandez C, Arriero JM, Espasa A, Candela A, Martin C, et al. CEA, CA 15-3 and CYFRA 21-1 in serum and pleural fluid of patients with pleural effusions. Eur Respir J. 1996. 9:17–23.
2. Porcel JM, Vives M, Esquerda A, Salud A, Perez B, Rodriguez-Panadero F. Use of a panel of tumor markers (carcinoembryonic antigen, cancer antigen 125, carbohydrate antigen 15-3, and cytokeratin 19 fragments) in pleural fluid for the differential diagnosis of benign and malignant effusions. Chest. 2004. 126:1757–1763.
3. Castelli GP, Poqnani C, Meisner M, Stuani A, Bellomi D, Sqarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care. 2004. 8:234–242.
4. Chan YL, Tseng CP, Tsay PK, Chang SS, Chiu TF, Chen JC. Procalcitonin as a marker of bacterial infection in the emergency department: an observational study. Crit Care. 2004. 8:12–20.
5. Bartter T, Santarelli R, Akers SM, Pratter MR. The evaluation of pleural effusion. Chest. 1994. 106:1209–1214.
6. Light RW. Diagnostic principles in pleural disease. Eur Respir J. 1997. 10:476–481.
7. McKenna JM, Chandrasekhar AJ, Henkin RE. Diagnostic value of carcinoembryonic antigen in exudative pleural effusions. Chest. 1980. 78:587–590.
8. Light RW, Macgregor MI, Luchsinger PC, Ball WC Jr. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972. 77:507–513.
9. Romero S, Candela A, Martin C, Hernandez L, Trigo C, Gil J. Evaluation of different criteria for the separation of pleural transudates from exudates. Chest. 1993. 104:399–404.
10. Burgess LJ, Maritz FJ, Taljaard JJ. Comparative analysis of the biochemical parameters used to distinguish between pleural transudates and exudates. Chest. 1995. 107:1604–1609.
11. Castano Vidriales JL, Amores Antequera C. Use of pleural fluid C-reactive protein in laboratory diagnosis of pleural effusions. Eur J Med. 1992. 1:201–207.
12. Alexandrakis MG, Coulocheri SA, Bouros D, Vlachonikolis IG, Eliopoulos GD. Significance of alpha-2-macroglobulin, alpha-1-acid glycoprotein, and C-reactive protein in pleural effusion differentiation. Respiration. 2000. 67:30–35.
13. Ghillani PP, Motte P, Troalen F, Jullienne A, Gardet P, Le Chevalier T, et al. Identification and measurement of calcitonin precursors in serum of patients with malignant diseases. Cancer Res. 1989. 49:6845–6851.
14. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C, et al. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993. 341:515–518.
15. Mackiewicz A, Speroff T, Ganapathi MK, Kushner I. Effects of cytokine combinations on acute phase protein production in two human hepatoma cell lines. J Immunol. 1991. 146:3032–3037.
16. Xirouchaki N, Tzanakis N, Bouros D, Kyriakou D, Karkavitsas N, Alexandrakis M, et al. Diagnostic value of interleukin-1alpha, interleukin-6, and tumor necrosis factor in pleural effusions. Chest. 2002. 121:815–820.
17. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994. 79:1605–1608.
18. Maskell NA, Butland RJ. Pleural Diseases Group. Standards of Care Committee. British Thoracic Society. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003. 58:Suppl 2. ii8–ii17.
19. Loddenkemper R. Light RW, Gary Lee YC, editors. Medical thoracoscopy. Textbook of pleural diseases. 2003. London: Arnold;498–512.
20. Lee JH, Chang JH. Diagnostic utility of serum and pleural fluid carcinoembryonic antigen, neuron-specific enolase, and cytokeratin 19 fragments in patients with effusions from primary lung cancer. Chest. 2005. 128:2298–2303.
21. Aoe K, Hiraki A, Murakami T, Eda R, Maeda T, Sugi K, et al. Diagnostic significance of interferon-gamma in tuberculous pleural effusions. Chest. 2003. 123:740–744.
22. Hiraki A, Aoe K, Eda R, Maeda T, Murakami T, Sugi K, et al. Comparison of six biological markers for the diagnosis of tuberculous pleuritis. Chest. 2003. 125:987–989.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download