Figures and Tables
Figure 1
Predicted and observed annual rates of change of height-adjusted FEV1 for men and women. The circles and error bars represent the mean ± 95% confidence interval of the observed annual rate of loss of height-adjusted FEV1 for subjects grouped by former smokers (mean packs/day = 0) and continued smokers divided into three subgroups by tertiles of mean packs/day. The dashed line connects the means predicted from the longitudinal model.

Figure 2
Decline in FEV1 during 10 years in men and women by smoking habits (never = never smoker, ex = ex-smoker, smoker = current smoker) and age at start of the observation period adjusted for family history of old and socio-economic class in a multiple linear regression model.

Figure 3
Comparison of geometric mean and SEM PC20 values and baseline FEV1% pred between smokers and ex-smokers in 1982 and 1986. The open symbols represent measurements in 1982 and the closed symbols the 1986 values. The asterisks indicate a significant fall in both FEV1% pred and PC20 in smokers over this period according to paired t tests.

Figure 4
The cumulative percentage of the study population responding with a 20% fall in FEV1 is shown for each of the sequential methacholine concentrations that were administered. The shift of the cumulative distribution upward and to the left indicates that there was an overall increase in responsiveness to methacholine during the study interval.
Figure 5
The mean change in AR (ie, LMCR) is plotted against the change in FEV1 over the 5-year interval. Separate plots are made for each smoking category. The continuous-smoking group is shifted to the left, indicating a greater decline in FEV1 compared to the group of sustained quitters. The continuous-smoking group is shifted upward, indicating a tendency for a greater increase in AR for a given decline in FEV1. The effect of changes in FEV1, however, has greater influence on changes in AR than does smoking status.
Figure 6
Mean postbronchodilator forced expiratory volume at 1 second (FEV1) for participants in the smoking intervention and placebo group who were sustained quitters (open circles) and continuous smokers (closed circles). The two curves diverge sharply after baseline.
Figure 7
Mean postbronchodilator forced expiratory volume at 1 second (FEV1) over the course of the study in all participants in whom the measurement was made. Circles/dotted line represent the smoking intervention and placebo group, triangles/solid lines represent the smoking intervention and ipratropium bromide group, and squares/dashed line represent the usual care group.
Figure 8
Lung function improved during Year 1 among quitters, but declined among continuing smokers. The subsequent rate of decline is twice as great among continuing smokers as among sustained quitters. Those who relapsed lost function and those who delayed quitting benefited regardless of when they quit.

Figure 9
Distribution of average annual rates of FEV1 change over 6 yr by smoking status. Numbers along X-axis are midpoints of the FEV1 change intervals. The solid line represents continuous smokers and the dashed line represents never smokers.

Figure 10
Mean FEV1, values in non-smokers (NN), consistent ex-smokers (XX), subjects who quit smoking during follow-up (SQ), and consistent smokers (SS) in several age groups. Data for men are shown in top panel and those for women in bottom panel. Numbers of subjects in each category are shown in parentheses.

Figure 11
Age-adjusted relative risk of hospitalization for chronic obstructive pulmonary disease (COPD) by pack years among smokers who inhaled, in the Copenhagen City Heart Study (CCHS). Note the logarithmic scale. M: male; F: female.

Figure 12
Proportion of subjects in the Bronchial Obstruction in the Nord Trondelag study sample reporting respiratory symptoms by forced expiratory volume in one second (FEV1) % predicted in males (–) and females (——), adjusted by age and pack-yrs. □: wheeze or breathlessness; ●: daily cough in periods; ◆: chronic bronchitis.

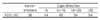
Table 3
Cross-sectional (CS) and longitudinal (LN) estimates of the effects of age and cigarette smoking on FEV1 and FVC

Table 4
Gender-specific decline in FEV1 estimated as changes from 1986 to 1996 in percent of predicted normal value by smoking habits, age group and chronic productive cough(FEV1% predicted 1996-FEV1% predicted 1986; negative result is consistent with decline)

References
1. Willemse BW, Postma DS, Timens W, Hacken NH. The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. 2004. 23:464–476.
2. XU X, Dockery DW, Ware JH, Speizer FE, Ferris BG Jr. Effect of cigarette smoking on rate of loss of pulmonary function in adults: a longitudinal assessment. Am Rev Respir Dis. 1992. 146:1345–1348.
3. Fletcher C, Peto R, Tink C, Speizer FE. The natural history of chronic bronchitis and emphysema. 1976. London: Oxford University Press.
4. Buist AS, Nagy JM, Sexton GJ. The effect of smoking cessation on pulmonary function: a 30-month follow-up of two smoking cessation clinics. Am Rev Respir Dis. 1979. 120:953–957.
5. Camilli AE, Burrows B, Knudson RJ, Lyle SK, Lebowitz MD. Longitudinal changes in forced expiratory volume in one second in adults: effects of smoking and smoking cessation. Am Rev Respir Dis. 1987. 135:794–799.
6. Lindberg A, Larsson LG, Ronmark E, Jonsson AC, Larsson K, Lundback B. Decline in FEV1 in relation to incident chronic obstructive pulmonary disease in a cohort with respiratory symptoms. COPD. 2007. 4:5–13.
7. Langhammer A, Johnsen R, Gulsvik A, Holmen TL, Bjermer L. Sex differences in lung vulnerability to tobacco smoking. Eur Respir J. 2003. 21:1017–1023.
8. Paoletti P, Carrozzi L, Viegi G, Modena P, Ballerin L, Di Pede F, et al. Distribution of bronchial responsiveness in a general population: effect of sex, age, smoking, and level of pulmonary function. Am J Respir Cirt Care Med. 1995. 151:1770–1777.
9. Sparrow D, O'Connor GT, Rosner B, Segal MR, Weiss ST. The influence of age and level of pulmonary function on nonspecific airway responsiveness. The Normative Aging Study. Am Rev Respir Dis. 1991. 143:978–982.
10. Buczko GB, Day A, Vanderdoelen JL, Boucher R, Zamel N. Effects of cigarette smoking and short-term smoking cessation on airway responsiveness to inhaled methacholine. Am Rev Respir Dis. 1984. 129:12–14.
11. Israel RH, Ossip-Klein DJ, Poe RH, Black P, Gerrity E, Greenblatt DW, et al. Bronchial provocation tests before and after cessation of smoking. Respiration. 1988. 54:247–254.
12. Lim TK, Taylor RG, Watson A, Joyce H, Pride NB. Changes in bronchial responsiveness to inhaled histamine over four years in middle aged male smokers and ex-smokers. Thorax. 1988. 43:599–604.
13. Wise RA, Kanner RE, Lindgren P, Connett JE, Altose MD, Enright PL, et al. The effect of smoking intervention and an inhaled bronchodilator on airways reactivity in COPD: the Lung Health Study. Chest. 2003. 124:449–458.
14. Postma DS, de Vries K, Koeter GH, Sluiter HJ. Independent influence of reversibility of air-flow obstruction and nonspecific hyperreactivity on the long-term course of lung function in chronic air-flow obstruction. Am Rev Respir Dis. 1986. 134:276–280.
15. Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, et al. Effects of smoking intervention and the use of an inhaled anticoholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994. 272:1497–1505.
16. Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Cirt Care Med. 2002. 166:675–679.
17. Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease. The Lung Health Study. Am J Respir Cirt Care Med. 2000. 161:381–390.
18. Friedman GD, Siegelaub AB. Changes after quitting cigarette smoking. Circulation. 1980. 61:716–723.
19. Burchfiel CM, Marcus EB, Curb JD, Maclean CJ, Vollmer WM, Johnson LR, et al. Effects of smoking and smoking cessation on longitudinal decline in pulmonary function. Am J Respir Cirt Care Med. 1995. 151:1778–1785.
20. Anto JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J. 2001. 17:982–994.
21. Sherrill DL, Enright P, Cline M, Burrows B, Lebowitz MD. Rates of decline in lung function among subjects who restart cigarette smoking. Chest. 1996. 109:1001–1005.
22. Xu X, Weiss ST, Rijcken B, Schouten JP. Smoking, changes in smoking habits, and rate of decline in FEV1: new insights into gender differences. Eur Respir J. 1994. 7:1056–1061.
23. Vestbo J, Prescott E, Lange P. Association of chronic mucus hypersecretion with FEV1 decline and chronic obstructive pulmonary disease. Copenhagen City Heart Study. Am J Respir Cirt Care Med. 1996. 153:1530–1535.
24. Prescott E, Bjerg AM, Andersen PK, Lange P, Vestbo J. Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur Respir J. 1997. 10:822–827.
25. Lange VJ. Can GOLD stage 0 provide information of prognostic value in Chronic Obstructive Pulmonary Disease? Am Rev Respir Crit Care Med. 2002. 166:329–332.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download