Abstract
Background
The causes of the pleural effusion are remained unclear in a the substantial number of patients with exudative effusions determined by an examination of the fluid obtained via thoracentesis. Among the various tools for diagnosing exudative pleural effusions, thoracoscopy has a high diagnostic yield for cancer and tuberculosis. Medical thoracoscopy can also be carried out under local anesthesia with mild sedation. The aim of this study was to determine diagnostic accuracy and safety of medical thoracoscopy.
Methods
Twenty-five patients with exudative pleural effusions of an unknown cause underwent medical thoracoscopy between October 2005 and September 2006 in Konyang University Hospital. The clinical data such as age, gender, preoperative pulmonary function, amounts of pleural effusion on lateral decubitus radiography were collected. The vital signs were recorded, and arterial blood gas analyses were performed five times during medical thoracoscopy in order to evaluate the cardiopulmonary status and acid-base changes.
Results
The mean age of the patients was 56.8 years (range 22-79). The mean depth of the effusion on lateral decubitus radiography (LDR) was 27.49 mm. The medical thoracoscopic pleural biopsy was diagnostic in 24 patients (96.0%), with a diagnosis of tuberculosis pleurisy in 9 patients (36%), malignant effusions in 8 patients (32%), and parapneumonic effusions in 7 patients (28%). Medical thoracoscopy failed to confirm the cause of the pleural effusion in one patient, who was diagnosed with tuberculosis by a pericardial biopsy. There were no significant changes in blood pressure, heart rate, acid-base and no major complications in all cases during medical thoracoscopy (p>0.05).
Figures and Tables
 | Figure 1The instruments of 5 mm minithoracoscopy.
Top. 5 mm trocar (WOLF Company, Knittlingen, Germany). 1.8 mm aspiration needile (WOLF Company, Knittlingen, Germany). 5 mm telescope (WOLF Company, Knittlingen, Germany). Endohook electrocautery (WOLF Company, Knittlingen, Germany)
Bottom. 5 mm thoracoscopic grasping forcep. (Tyco-AutoSuture Tyco Healthcare, Gosport, UK)
|
 | Figure 2The comparisons of 5 mm & 10 mm trocar and telescope.
Top. 5 mm trocar (WOLF Company, Knittlingen, Germany ). 10 mm trocar (WOLF Company, Knittlingen, Germany). 5 mm telescope (WOLFCompany, Knittlingen, Germany)
Bottom. 10 mm telescope (WOLF Company, Knittlingen, Germany)
|
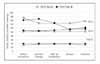
 | Figure 3Changes of PaO2, PaCO2 and MAP in patients aged below or above 65 years old through the process of medical thoracoscopy.
All values were measured during supplement of 5 ml/min of oxygen via mask.
PaO2: arterial oxygen tension; PaCO2: arterial carbon dioxide tension; MAP: mean arterial pressure.
|
 | Figure 4Changes of PaO2, PaCO2 and MAP by sex differences through the process of medical thoracoscopy.
All values were measured during supplement of 5 ml/min of oxygen via mask.
PaO2: arterial oxygen tension PaCO2: arterial carbon dioxide tension MAP: mean arterial pressure.
|
 | Figure 5Changes of PaO2, PaCO2 and MAP in patients with LDR below or above 27.4 mm through the process of medical thoracoscopy.
All values were measured during supplement of 5 ml/min of oxygen via mask.
PaO2: arterial oxygen tension PaCO2: arterial carbon dioxide tension MAP: mean arterial pressure LDR: depth of pleural effusion on lateral decubitus radiography.
|
 | Figure 6Changes of PaO2, PaCO2 and MAP in patient with FEV1% below or above 50 through the process of medical thoracoscopy.
All values were measured during supplement of 5 ml/min of oxygen via mask.
PaO2 : arterial oxygen tension PaCO2 : arterial carbon dioxide tension MAP: mean arterial pressure.
|
References
1. Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002. 346:1971–1977.
2. Maskell NA, Butland RJ. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003. 58:suppl2. ii8–ii17.
3. Baumann MH. Closed needle biopsy of the pleura is a valuable diagnostic procedure. J Broncho. 1998. 5:327–331.
4. Salyer WR, Eggleston JC, Erozan YS. Efficacy of pleural needle biopsy and pleural fluid cytopathology in the diagnosis of malignant neoplasm involving the pleura. Chest. 1975. 67:536–539.
5. Kennedy L, Sahn SA. Noninvasive evaluation of the patient with a pleural effusion. Chest Surg Clin N Am. 1994. 4:451–465.
6. Valdes L, Alvarez D, San Jose E, Penela P, Valle JM, Garcia-Pazos JM, et al. Tuberculous pleurisy: a study of 254 patients. Arch Intern Med. 1998. 158:2017–2021.
7. Prakash UB, Reiman HM. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion: analysis of 414 cases. Mayo Clin Proc. 1985. 60:158–164.
8. Harris RJ, Kavuru MS, Rice TW, Kirby TJ. The diagnostic and therapeutic utility of thoracoscopy: a review. Chest. 1995. 108:828–841.
9. Kim WJ, Lee HY, Lee SH, Cho SJ, Park WS, Kim JK, et al. Diagnostic accuracy of 2-mm minithoracoscopic pleural biopsy for pleural effusion. Tuberc Respir Dis. 2004. 57:138–142.
10. Malthaner RA, Inculet RI. Minithoracoscopy for pleural effusions. Can Respir J. 1998. 5:253–254.
11. Mathur PN, Astoul P, Boutin C. Medical thorac oscopy: technical details. Clin Chest Med. 1995. 16:479–486.
12. Brandt HJ, Loddenkemper R, Mai J. Atlas of diagnostic thoracoscopy: indications-technique. 1985. New York: Thieme.
13. Ohtsuka T, Imanaka K, Endoh M, Kohno T, Nakajima J, Kotsuka Y, et al. Hemodynamic effects of carbon dioxide insufflation under single-lung ventilation during thoracoscopy. Ann Thorac Surg. 1999. 68:29–33.
14. Oldenburg FA Jr, Newhouse MT. Thoracoscopy. A safe, accurate diagnostic procedure using the rigid thoracoscope and local anesthesia. Chest. 1979. 75:45–50.
15. Moss AJ, Wynar B. Tachycardia in house officers presenting cases at grand rounds. Ann Intern Med. 1970. 72:255–256.
16. Jacobaeus HC. Über die Möglichkeit, die Zystoskopie bei Untersuchung seröser Höhlen anzuwenden. Munch Med Wschr. 1910. 40:2090–2092.
17. Miller JI Jr. Therapeutic thoracoscopy: new horizons for an established procedure. Ann Thorac Surg. 1991. 52:1036–1037.
18. LoCicero J 2nd. Minimally invasive thoracic surgery, video-assisted thoracic surgery and thoracoscopy. Chest. 1992. 102:330–331.
19. Inderbitzi R. Chirurgische Thorakoskopie. 1993. 1st ed. Berlin: Springer.
20. Tape TG, Blank LL, Wigton RS. Procedural skills of practicing pulmonologist: a national survey of 1,000 members of the American College of Physicians. Am J Respir Crit Care Med. 1995. 151:282–287.
21. Faurschou P, Madsen F, Viskum K. Thoracoscopy: influence of the procedure on some respiratory and cardiac values. Thorax. 1983. 38:341–343.
22. Page RD, Jeffrey RR, Donnelly RJ. Thoracoscopy: a review of 121 consecutive surgical procedures. Ann Thorac Surg. 1989. 48:66–68.
23. Boutin C, Viallat JR, Cargnino P, Farisse P, Choux R. La thoracoscopie en 1980: revue general. Poumon Coeur. 1981. 37:9–11.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download