Abstract
A thymic carcinoma is a rare malignant neoplasm of the thymus epithelium, which can be distinguished from a benign or invasive thymoma. Contrary to a thymoma, the association of a thymic carcinoma and autoimmune disease is rare, with only a few cases having been reported.
Herein, a case of thymic carcinoma diagnosed concurrently with systemic lupus erythematosus (SLE) is reported. A 49 year-old man presented at our clinic with myalgia. He was diagnosed with SLE, based on an oral ulcer, lymphopenia, and positive ANA and anti-Sm antibodies. Incidentally, a routine chest X-ray showed a large mediastinal mass. Pathological examination of the mediastinal mass revealed an undifferentiated thymic carcinoma, of WHO classification type C. Further work-up for staging showed multiple bone and lung metastases. With a palliative aim, he received systemic chemotherapy, but refused further chemotherapy after the 2nd course. Currently, the patient has not been followed up since the chemotherapy.
Figures and Tables
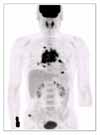
Figure 1
Positron emission tomography revealed the strong FDG uptake on a large irregular mass in anterior mediastinum, multiple lung nodules with bilateral lymphadenopathy, the 8th T-spine, right iliac crest, and the posterior pararenal area. It suggested malignant mediastinal tumor with multiple lung and bone metastases.
References
1. Levine GD, Rosai J. Thymic hyperplasia and neoplasia: a review of current concepts. Hum Pathol. 1978. 9:495–515.
2. Cameron RB. Devita , Hellman , Rosenberg , editors. Neoplasms of the mediastinum. Principles and practice of oncology. 2000. 6th ed. 1024.
3. Sungur A, Ruacan S, Gungen Y, Dalkara T. Myasthenia gravis and primary squamous cell carcinoma of the thymus. Arch Pathol Lab Med. 1993. 117:937–938.
4. Yonekura S, Nagao T, Arimori S, Kobayashi I, Fukuhara N, Mori T. Thymic carcinoma associated with pinealoma and terminating with peroxidase-negative acute myeloid leukemia. Intern Med. 1992. 31:825–827.
5. Thomas CV, Manivel JC. Thymic carcinoma and aplastic anemia: report of a previously undocumented association. Am J Hematol. 1987. 25:333–335.
6. Negron-Soto JM, Cascade PN. Squamous cell carcinoma of the thymus with paraneoplastic hypercalcemia. Clin Imaging. 1995. 19:122–124.
7. Suster S, Rosai J. Thymic carcinoma: a clinicopathologic study of 60 cases. Cancer. 1991. 67:1025–1032.
8. Eng TY, Fuller CD, Jagirdar J, Bains Y, Thomas CR Jr. Thymic carcinoma: state of the art review. Int J Radiat Oncol Biol Phys. 2004. 59:654–664.
9. Fong PH, Wee A, Chan HL, Tan YO. Primary thymic carcinoma and its association with dermatomyositis and pure red cell aplasia. Int J Dermatol. 1992. 31:426–428.
10. Di Cataldo A, Villari L, Milone P, Miano AE, Sambataro MP, Florio G, et al. Thymic carcinoma, systemic lupus erythematosus, and hypertrophic pulmonary osteoarthtopathy. Pediatr Hematol Oncol. 2000. 17:701–706.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download