Abstract
A 29-year-old female patient presented with exertional dyspnea that she had suffered with for 2 months. The chest X-ray displayed right pleural effusion that was diagnosed as chyle, according to the level of cholesterol and triglyceride in the pleural fluid. VATS (video assisted thoracic surgery) of the right lung was performed on the 7th day of hospitalization for obtaining a lung biopsy and to control the of pneumochylothorax. On the 11th hospitalization day, VATS of left lung was also performed to control the recurrent pneumothorax via pleurodesis. The lung biopsy showed moderate amounts of spindle-shaped and rounded cells (so-called LAM cells), which were reactive to actin and HMB45 (on immunohistochemical stains). We report here on a rare case of lymphangioleiomyomatosis combined with chylothorax and bilateral pneumothroraces.
Figures and Tables
Figure 1
Pleural fluid before (left) and after (right) centrifugation. The centrifugation resulted in a change of color of the pleural fluid from deep brown (left) to yellow (right) - instead of clearing of pleural fluid- suggesting that the pleural fluid is not empyema. The change of color of pleural fluid may be explained by the precipitation of red cells after centrifugation.

Figure 2
The chest radiograph obtained at 1st hospitalization day displays total haziness of right whole lung field and mild mediastinal deviation to the left hemithorax, suggesting large amount of pleural effusion (A). The chest radiograph obtained on the 3rd hospitalization day displays right pneumothorax. The amount of pleural effusion was considerably decreased after catheter drainage (B). The chest radiograph obtained on the 5th hospitalization day displays bilateral pneumothoraces. The right pleural effusion is nearly resolved (C). The chest CT scan with lung window setting shows multiple, uniform and variable-sized, small cysts with thin and regular wall in both lungs (D,E).
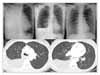
Figure 3
H&E stain (A, B). The cystic space is empty and shows moderate amounts of spindle-shaped and rounded cells (so-called LAM cells, arrow) in its periphery (×40, A). The proliferating LAM cells are spindle, round, or oval shaped (×400, B). Immunohistochemical stain (C,D). LAM cells are positive to smooth muscle actin (×400, C), as well as to HMB45 (×400, D).

References
1. Kang SY, Yoon KH, Yoo JH, Kang HM, Yang MH. A case of pulmonary lymphangioleiomyomatosis. Tuberc Respir Dis. 1992. 39:266–270.
2. Kang SB, Park SJ, Lee SH, Jung DY, Yoo JH, Kim JY, et al. A case of lymphangioleiomyomatosis with renal angiomyolipoma. Tuberc Respir Dis. 2001. 50:245–251.
3. Corrin B, Liebow AA, Friedman PJ. Pulmonary lymphangioleiomyomatosis. A review. Am J Pathol. 1975. 79:348–382.
4. Kim SW, Choi JS, Na MH, Yu JH, Lim SP, Lee Y. Lymphagioleiomyomatosis with bilateral chylothorax: 1 case report. Korean J Thorac Cardiovasc Surg. 2004. 37:1029–1031.
5. Sung SW, Kim JH, Kim YT, Seo JW, Yoo CG, Kim YH, et al. Bilateral sequential lung transplantation for a case with respiratory failure due to lymphangioleiomyomatosis. Korean J Thorac Cardiovasc Surg. 2000. 33:88–95.
6. Oh YM, Mo EK, Jang SH, Yoo CG, Kim YW, Seo JW, et al. Pulmonary lymphangioleiomyomatosis in Korea. Thorax. 1999. 54:618–621.
7. Almoosa KF, Ryu JH, Mendez J, Huggins JT, Young LR, Sullivan EJ, et al. Management of pneumothorax in lymphangioleiomyomatosis: effects on recurrence and lung transplantation complications. Chest. 2006. 129:1274–1281.
8. Kitaichi M, Nishimura K, Itoh H, Izumi T. Pulmonary Lymphangioleiomyomatosis: a report of 46 patients including a clinicopathologic study of prognostic factors. Am J Respir Crit Care Med. 1995. 151:527–533.
9. Taylor JR, Ryu J, Colby TV, Raffin TA. Lymphangioleiomyomatosis: clinical course in 32 patients. N Engl J Med. 1990. 323:1254–1260.
10. Chuang ML, Tsai YH, Pang LC. Early chylopneumothorax in a patient with pulmonary lymphangioleiomyomatosis. J Formos Med Assoc. 1993. 92:278–282.
11. Johnson S. Rare diseases. 1. Lymphangioleiomyomatosis: clinical features, management and basic mechanisms. Thorax. 1999. 54:254–264.
12. Urban T, Lazor R, Lacronique J, Murris M, Labrune S, Valeyre D, et al. Pulmonary lymphangioleiomyomatosis. A study of 69 patients. Medicine (Baltimore). 1999. 78:321–337.
13. Aberle DR, Hansell DM, Brown K, Tashkin DP. Lymphangioleiomyomatosis: CT, chest radiographic, and functional correlations. Radiology. 1990. 176:381–387.
14. Han SG, Heo JH, Lee KI, Kim HJ, Pai YM, Whang YH, et al. A case of idiopathic bilateral chylothorax treated by conservative approach. Tuberc Respir Dis. 1998. 45:1082–1086.
15. Ryu JH, Doerr CH, Fisher SD, Olson EJ, Sahn SA. Chylothorax in lymphangioleiomyomatosis. Chest. 2003. 123:623–627.
16. Eliasson AH, Phillips YY, Tenholder MF. Treatment of lymphangioleiomyomatosis: a meta-analysis. Chest. 1989. 196:1352–1355.
17. Rossi GA, Balbi B, Oddera S, Lantero S, Ravazzoni C. Response to treatment with an analog of the luteinizing releasing hormone in a patient with pulmonary lymphangioleiomyomatosis. Am Rev Respir Dis. 1991. 143:174–176.
18. Boehler A, Speich R, Russi EW, Weder W. Lung transplantation for lymphangioleiomyomatosis. N Engl J Med. 1996. 335:1275–1280.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download