Abstract
Background
B-type natriuretic peptide (BNP) has been shown to be strong mortality predictors in a wide variety of cardiovascular syndromes. Little is known about BNP in patients with acute respiratory distress syndrome (ARDS). We studied whether BNP can predict mortality in patients with ARDS.
Method
Echocardiographic study was done to all patients with ARDS, and we excluded patient with low ejection fraction (less than 50%) or showing any features of diastolic dysfunction. 47 patients were enrolled between December, 2003 and February, 2006. Parameters including BNP were obtained within 24h hours at the time of enrollment.
Result
Mean BNP concentrations and APACHE II scores differed between the survivors and nonsurvivors (BNP, 219.5 ± 57.7 pg/mL vs 492.3 ± 88.8 pg/mL; p=0.013, APACHE II score, 17.4 ± 1.6 vs 23.1 ± 1.3, p=0.009, respectively). With the use of the threshold value for BNP of 585 pg/mL, the specificity for the prediction of mortality was 94%. The threshold value for APACHE II of 15.5 showed sensitivity of 87%. 'APACHE II + 11×logBNP' showed sensitivity 63%, and specificity 82%, using threshold value for 46.14.
Among patients with congestive heart failure (CHF), B-type natriuretic peptide (BNP) concentrations reflect left ventricular end-diastolic pressure, left ventricular ejection fraction, and New York Heart Association heart failure class1-5. Assay for BNP has shown comparable accuracy in diagnosing, monitoring and establishing prognosis in patients with heart failure6-9. Although there were some reports that BNP can be elevated in patients with ARDS10,11, little is known about the correlation between BNP and mortality in patients with ARDS. Some articles about BNP in patients with shock or respiratory failure were published, but the enrolled patients were not 100% ARDS patients12-14. Moreover, many of enrolled patients showed low ejection fraction, and this definitely affected the BNP concentration. We performed this study to see if BNP concentrations were elevated in patients with ARDS who had normal ejection fraction and evaluate the relationship between BNP and other variables. We also investigated if BNP and other variables could show difference between survivors and nonsurvivors and could predict mortality.
This was a prospective observational study. Consecutive patients admitted to medical, cardiac, and surgical intensive care units of The Kangnam St. Mary's Hospital who met inclusion criteria were enrolled. The study period was from December, 2003 to February, 2006. Written informed consent was obtained from either patient or next of kin. The Kangnam St. Mary's Hospital Institutional Review Board approved the study.
Patients were included who had acute respiratory failure (partial pressure of oxygen in arterial blood (PaO2) / fractional concentration of inspired oxygen (FiO2) ≤ 200 mmHg), bilateral infiltration on chest radiography, and no clinical evidence of increased left arterial pressure. Echocardiographic study was done and patients with ejection fraction (EF) lower than 50% or showing any features of diastolic dysfunction were ruled out. We also excluded patients younger than 18 years.
BNP, PaO2, FiO2, C-reactive protein (CRP), Acute Physiology and Chronic Health Evaluation II (APACHE II) score, and EF were obtained within 24h hours at the time of enrollment. Patients were followed up, and 30-day survival was documented. Blood samples were obtained from peripheral blood. BNP was measured using the quantitative immunofluorescence assay Triage BNP (Biosite, San Diego, USA) on 5 ml of whole blood drawn in an ethylenediaminetetraacetic acid (EDTA) tube. This assay can detect BNP levels in the 5-5000 pg/mL range. APACHE II scores were calculated using data available from the 24-hr period at the time of enrollment. Transthoracic echocardiography is performed routinely in patients with ARDS. Systolic left ventricle (LV) dysfunction was defined as an EF below 50%. In patients without systolic LV dysfunction, diastolic dysfunction was defined as transmitral flow parameters consistent with one of the three patterns of diastolic dysfunction: impaired relaxation (LV peak E-wave velocity / LV peak A-wave velocity (E/A) < 1 and E-wave deceleration time (EDT) > 240 ms), pseudonormalization (1 < E/A < 2 and 150 < EDT < 200 ms) or restricted filling (E/A > 2 and EDT < 150 ms)15. Right ventricle (RV) dysfunction was defined as an RV-end diastolic area (EDA)/LV-EDA ratio grater than 0.616. Pulmonary hypertension was defined when pulmonary regurgitation velocity > 2m/sec17. High Positive End-Expiratory Pressures (PEEP) was defined as more than 15 cmH2O. The patients, researchers, physicians, and echocardiographers were blinded to the BNP concentrations.
Independent samples T test was done to compare means of continuous variables. Chi-square test was used for analysis of categorical variables. Correlations between each variable were evaluated by bivariate analysis with Pearson correlation. Receiver operating characteristic (ROC) curves for BNP and APACHE II score were constructed to predict mortality. All statistical analyses were performed with SPSS software (Chicago, IL, USA).
From 2003 December to 2006 February, 103 patients were diagnosed as ARDS. 17 patients refused to be enrolled. 14 patients were excluded because of failure of BNP sampling or echocardiographic examination within 24h hours of diagnosis. 25 patients showed LV dysfunction. So among 103 patients, 47 patients met inclusion criteria. 33 patients were on the intubated state during BNP sampling, 36 were during echocardiographic examination.
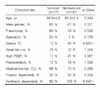
Seventeen patients were alive and thirty patients were dead at day 30. The baseline characteristics of the study group are shown in Table 1. Percentage of sepsis and ventilator dependent showed significant differences (Sepsis, 12% vs 43%; p=0.026, Ventilator dependent, 82% vs 100%; p=0.042, respectively). Others did not differ significantly. BNP concentration and APACHE II score differ significantly between those who survived and those who died (BNP, 219.5 ± 57.7 pg/mL vs 492.3± 88.8 pg/mL; p=0.013, APACHE II score, 17.4 ± 1.6 vs 23.1 ± 1.3: p=0.009, respectively). Figure 1 and 2 show these differences. Parameters other than APACHE II score and BNP failed to show difference (Table 2). BNP concentration and EF were not different significantly between non-intubated and intubated group (BNP ; non-intubated : 331.7 ± 109.8 pg/mL vs intubated : 419.8 ± 77.3 pg/mL, p=0.517, EF ; non-intubated : 59.3 ± 2.1 % vs intubated : 60.3 ± 1.2 %, p=0.686).
BNP concentration was correlated with serum creatinine level (r = 0.374, p = 0.010), but not with EF, age, PaO2, FiO2, PaO2/FiO2, CRP, and APACHE II score. APACHE II score was correlated with PaO2/FiO2 (r = -0.292, p = 0.047), Cr (r = 0.375, p = 0.009) (Table 3).
In total enrolled patients, mean BNP concentration was 393 ± 63 pg/mL, and 66% of patients showed elevated BNP level (> 100 pg/mL). We examined percentage of patients who are BNP > 100 pg/mL and mean BNP concentration between variable medical conditions(Table 4). These conditions can be causes of raised plasma BNP level18. Sepsis patients showed significantly increased percentage of BNP elevation, but mean BNP didn't differ significantly. In other conditions, although higher percentages were seen, p values were more than 0.05.
With the use of the threshold value for BNP of 585 pg/mL, the sensitivity for the prediction of mortality was 43%, with specificity of 94%, and area under the curve (AUC) of 0.678. The threshold value for APACHE II of 15.5 showed sensitivity of 87%, specificity of 47%, and AUC of 0.710 (Figure 3). In order to combine these two factors, we used log-transformed BNP values. 'APACHE II + 11×logBNP' showed the best result of AUC (0.747). Using the threshold value for 46.14, sensitivity was 63%, and specificity was 82% (Figure 4). Sensitivity, specificity, PPV, NPV, AUC for BNP, APACHE II, and APACHE II + 11×logBNP are given in Table 5.
BNP can be elevated not only in CHF patients but also other critically ill patients12,19. Little is known in ARDS patients. Maeder and colleagues10 reported one case of ARDS patient who showed marked elevation of BNP in spite of normal ejection fraction. Although there are some articles about BNP in respiratory failure patients13,14, none of them were about only ARDS patients. We wanted to evaluate the relationship between BNP and mortality in ARDS patients, and also to exclude the effect of LV dysfunction on BNP. So, we enrolled patients who met the diagnostic criteria of ARDS, and ruled out any patients who had less than 50% of ejection fraction and/or any features of diastolic dysfunction. This can explain the relatively small number of patients in this study in spite of long study period.
BNP concentrations among those who died were higher than those who survived in shock patients12. Although APACHE II score is well known predictor of mortality in critically ill patients, there was no significant difference in APACHE II score between two groups in that study. In a Jefic D et al's study, mean BNP concentrations did not differ between the survivors and nonsurvivors in respiratory failure patients, and mean APACHE II scores were higher in nonsurvivors than in survivors13. In our study, not only BNP concentrations but also APACHE II scores are elevated significantly in patients who died. Our study is unique in that we enrolled only ARDS patients and ruled out LV dysfunction patients. This may be the reason of the different result compared to previous two similar studies. What we tried to show was BNP could be elevated in ARDS patients without the effect of LV dysfunction, and this elevation could be related to the mortality. We clearly showed that BNP concentrations and APACHE II scores were elevated significantly in nonsurvivors. BNP is useful biomarkers for the diagnosis of HF. However, BNP might be raised to different degrees in critical illness and various pulmonary diseases. In these situations, BNP may also serve as markers of severity and prognosis18. ARDS is one of these diseases, and we showed BNP > 585 pg/mL has a high specificity for the prediction of mortality.
APACHE II score is well known predictor of mortality in critical illness patients. BNP also seems to be the predictor of mortality. APACHE II score and BNP were not correlated significantly in critically ill patients19. In our study, the result was also same. We hypothesized that BNP could reflect certain conditions which APACHE II score couldn't cover. So, we combined there two markers hoping they could produce synergistic result in predicting mortality. BNP concentrations showed wide variation compared to APCHE II score, so log BNP was used to correct this problem. The concept of log BNP was adapted from previous published study12. Although there was no reference in combination of these two scores, we could prove 'APACHE II + 11×logBNP' was better than BNP or APACHE II in predicting mortality.
It is well known that the BNP is elevated in patients with low ejection fraction. However, in our study, there was no correlation between BNP concentration and EF. This may be due to the exclusion of patients who showed low ejection fraction. This result can tell we effectively eliminated the effect of LV dysfunction on BNP in our study, and we could examine more pure effect of ARDS on BNP concentration.
Sepsis, renal failure, pulmonary hypertension, right ventricular dysfunction, high PEEP, and shock state can be the cause of raised plasma BNP levels18. In ARDS patients, these conditions may coexist commonly. This may explain the reason of elevated level of BNP in ARDS. The high mortality rate in patients with high BNP levels may reflect these conditions. However, in our study, only sepsis patients showed just increased percentage of BNP elevation. We are not sure the elevation of BNP is due to sepsis in our study. No other medical conditions affected significantly the level of BNP. BNP concentration was also seemed not to be affected by the intubated state. Maybe this is because the number of enrolled patients was small, and/or there were another factors that we don't know which can elevate BNP levels. Recently, Karmpaliotis et al published similar result as ours20. BNP appears useful in excluding cardiogenic pulmonary edema, but some ARDS patients showed elevation of BNP in the absence of CHF. Among those patients, high BNP concentration was associated with mortality. Unfortunately, they also could not explain the pathogenesis of this result.
The limitation of our study is the small number of patients. A second limitation is that we only measured a single BNP concentration at the time of enrollment. As BNP is known to fluctuate, serial measurement of BNP may be more useful than single. Another limitation is that we did not measure N-terminal pro BNP (NT-pro BNP) which is also well known useful marker for the diagnosis of heart failure.
Our results are useful as they reflect information of only ARDS patients. All enrolled patients were compatible with the diagnostic criteria of ARDS. They are also unique in that they had normal ejection fraction. We showed that BNP and APACHE II score could predict mortality. When we combined these two factors, we could get better results. Further study about BNP in ARDS patients should be done.
Figures and Tables
 | Figure 1Box and whiskers plots of median B-type natriuretic peptide (BNP) concentrations among surviving patients vs. those dying during the study. The median BNP concentrations among those dying were significantly higher than those surviving (p = 0.013). |
 | Figure 2Box and whiskers plots of median acute physiology and chronic health evaluation (APACHE) II scores among surviving patients vs. those dying during the study. The median APACHE II scores among those dying were significantly higher than those surviving (p = 0.009). |
 | Figure 3Receiver operating characteristic curve for BNP (left) APACHE II score (right) for the prediction of mortality. BNP: B-type natriuretic peptide; APACHE: Acute Physiology and Chronic Health Evaluation |
 | Figure 4Receiver operating characteristic curve for 'APACHE II score + 11×log BNP' for the prediction of mortality.
BNP: B-type natriuretic peptide; APACHE: Acute Physiology and Chronic Health Evaluation
|
References
1. Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002. 347:161–167.
2. Vasan RS, Benjamin EJ, Larson MG, Leip EP, Wang TJ, Wilson PW, et al. Plasma natriuretic peptides for community screening for left ventricular hypertrophy and systolic dysfunction: the Framingham heart study. JAMA. 2002. 288:1252–1259.
3. Maisel AS, Koon J, Krishnaswamy P, Kazenegra R, Clopton P, Gardetto N, et al. Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J. 2001. 141:367–374.
4. Omland T, Aakvaag A, Bonarjee VV, Caidahl K, Lie RT, Nilsen DW, et al. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation. 1996. 93:1963–1969.
5. Krishnaswamy P, Lubien E, Clopton P, Koon J, Kazanegra R, Wanner E, et al. Utility of B-natriuretic peptide levels in identifying patients with left ventricular systolic or diastolic dysfunction. Am J Med. 2001. 111:274–279.
6. Hammerer-Lercher A, Neubauer E, Muller S, Pachinger O, Puschendorf B, Mair J. Head-to-head comparison of N-terminal pro-brain natriuretic peptide, brain natriuretic peptide and N-terminal pro-atrial natriuretic peptide in diagnosing left ventricular dysfunction. Clin Chim Acta. 2001. 310:193–197.
7. Mair J, Hammerer-Lercher A, Puschendorf B. The impact of cardiac natriuretic peptide determination on the diagnosis and management of heart failure. Clin Chem Lab Med. 2001. 39:571–588.
8. Bettencourt P. NT-proBNP and BNP: biomarkers for heart failure management. Eur J Heart Fail. 2004. 6:359–363.
9. Yeo KT, Wu AH, Apple FS, Kroll MH, Christenson RH, Lewandrowski KB, et al. Multicenter evaluation of the Roche NT-proBNP assay and comparison to the Biosite Triage BNP assay. Clin Chim Acta. 2003. 338:107–115.
10. Maeder M, Ammann P, Rickli H, Diethelm M. Elevation of B-type natriuretic peptide levels in acute respiratory distress syndrome. Swiss Med Wkly. 2003. 133:515–518.
11. Mitaka C, Hirata Y, Nagura T, Tsunoda Y, Itoh M, Amaha K. Increased plasma concentrations of brain natriuretic peptide in patients with acute lung injury. J Crit Care. 1997. 12:66–71.
12. Tung RH, Garcia C, Morss AM, Pino RM, Fifer MA, Thompson BT, et al. Utility of B-type natriuretic peptide for the evaluation of intensive care unit shock. Crit Care Med. 2004. 32:1643–1647.
13. Jefic D, Lee JW, Jefic D, Savoy-Moore RT, Rosman HS. Utility of B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide in evaluation of respiratory failure in critically ill patients. Chest. 2005. 128:288–295.
14. Bal L, Thierry S, Brocas E, Van de Louw A, Pottecher J, Hours S, et al. B-type natriuretic peptide (BNP) and N-terminal-proBNP for heart failure diagnosis in shock or acute respiratory distress. Acta Anaesthesiol Scand. 2006. 50:340–347.
15. Garcia MJ, Thomas JD, Klein AL. New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol. 1998. 32:865–875.
16. Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F. Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med. 2002. 166:1310–1319.
17. Feigenbaum H, Armstrong WF, Ryan T. Feigenbaum's Echocardiography. 2005. 6th ed. Philadelphia: Lippincott Williams & Wilkins;209.
18. Phua J, Lim TK, Lee KH. B-type natriuretic peptide: issues for the intensivist and pulmonologist. Crit Care Med. 2005. 33:2094–2013.
19. Berendes E, Van Aken H, Raufhake C, Schmidt C, Assmann G, Walter M. Differential secretion of atrial and brain natriuretic peptide in critically ill patients. Anesth Analg. 2001. 93:676–682.
20. Karmpaliotis D, Kirtane AJ, Ruisi CP, Polonsky T, Malhotra A, Talmor D, et al. Diagnostic and prognostic utility of brain natriuretic Peptide in subjects admitted to the ICU with hypoxic respiratory failure due to noncardiogenic and cardiogenic pulmonary edema. Chest. 2007. 131:964–971.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download