Abstract
Background
Toxocariasis is a common cause of eosinophilia and eosinophilic lung disease in Korea. We analyzed the characteristics of eosinophilic lung disease in toxocariasis.
Method
One hundred and forty one patients with eosinophilia caused by a toxocara larval infection were evaluated from September 1, 2001 through March 30, 2006. The plain chest x-ray, chest CT(computed tomography), and bronchoalveolar larvage(BAL) were examined. A diagnosis of toxocariasis was made by ELISA using that secretory-excretory antigen from the T. canis larvae.
Results
Toxocarial eosinophilic lung diseases was diagnosed in 32 out of 141 patients. Ground glass attenuation was the main feature on the CT scans in 23 out of 141 patients (71.9%). Thirteen patients (40.6%) had a random in zonal distribution on CT. Pleural effusion was observed in 9 patients (28.1%). Twenty eight patients (87.5%) complained of respiratory symptoms. Eleven patients (34.4%) had gastrointestinal symptoms and 12 patients (37.5%) had liver infiltration.
Figures and Tables
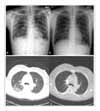 | Figure 1(A) Chest X-ray from 27 year-old male patient with toxocariasis showing numerous, poorly defined multiple patchy increased densities area scattered in both upper and lower lobe. 1(B) After 1months later, Chest X-ray reveals nealry disappered numerous, poorly defined multiple patchy increased densities area scattered in both upper and lower lobe (C) Chest computed tomography scan from 47 year-old female patient with toxocariasis showing multifocal patch or ill defined nodular ground glass opacity in right lung and left upper lobe. (D)After 5months later, Chest computed tomography scan reveals nearly disappered multifocal patch or ill defined nodular ground glass opacity in right lung and left upper lobe. |
References
1. Alberts WM. Eosinophilic intestitial lung disease. Curr Opin Pulm Med. 2004. 10:419–424.
2. Albera C, Ghio P. Eosinophils in eosinophilic pneumonia. Eur Respir J. 1996. 9:2437–2439.
3. Mochimaru H, Kawamoto M, Fukuda Y, Kudoh S. Clinicopathological differences between acute and chronic eosinophilic pneumonia. Respilogy. 2005. 10:76–85.
4. Inoue K, Inoue Y, Arai T, Nawa Y, Kashiwa Y, Yamamato S, et al. Chronic eosinophilic pneumonia due to visceral larva migrans. Intern Med. 2002. 41:478–482.
5. Lee SP. Pathophysiology of hypersensitivity in human by Toxocara canis larval infection. 2001. Chung-Ang University Doctoral Thesis.
6. Kwon NH, Oh MJ, Lee SP, Lee BJ, Choi DC. The prevalence and diagnostic value of toxocariasis in unknown eosinophilia. Ann Hematol. 2006. 85:233–238.
7. Lim JH, Lee KS. Eosinophilic infiltration in Korea: idiopathic? Korean J Radiol. 2006. 7:4–6.
8. Cho SY, Kong Y, Kim SI, Kang SY. Measurement of 150 kDa protein of Taenia solium metacestodes by antibody-sandwich ELISA in cerebrospinal fluid of neurocysticercosis patients. Korean J Parasitol. 1992. 30:299–307.
9. Allen JN, Davis WB. Eosinophilic lung disease. Am J Respir Crit Care Med. 1994. 150:1423–1438.
10. Cheon JE, Lee KS, Jung GS, Chung MH, Cho YD. Acute eosinophilic pneumonia: radiographic and CT findings in six patients. Am J Roentgenol. 1996. 167:1195–1199.
11. Johkoh T, Muller NL, Akira M, Ichikado K, Suga M, Ando M, et al. Eosionophilic lung diseases: diagnostic accuracy of thin-section CT iin 111 patients. Radiology. 2000. 216:773–780.
12. Bernstein IL, Boushey HA, Cherniack RM, Fink JN, Fulmer JD, Goetzl EJ, et al. Summary and recommendations of a workshop on the investigative use of fiberoptic bronchoscopy and bronchoalveolar lavage in asthmatic patients. Chest. 1985. 88:136–138.
13. Beaver PC, Synder CH, Carrera GM, Dent JH, Lafferty JW. Chronic eosinophilia due to visceral larva migrans: report of three cases. Pediatrics. 1952. 9:7–19.
14. Deutz A, Fuchs K, Auer H, Kerbl U, Aspock H, Kofer J. Toxocaro-infestations in Austria: a study on the risk of infection of farmers, slaughterhouse staff, hunters and veterinarians. Parasitol Res. 2005. 97:390–394.
15. Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev. 2003. 16:265–272.
16. Baldisserotto M, Conchin CF, Soares Mda G, Araujo MA, Kramer B. Ultrasound findings in children with toxocariasis: report on 18 cases. Pediatr Radiol. 1999. 29:316–319.
17. Lee SP, Lim YH, Choi DC. Hepatic infiltration with eosinophilia: is a new disease syndrome? [Abstract]. J Allergy Clin Immunol. 1999. 103:S112.
18. Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepidemiological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002. 40:113–117.
19. Jacquier P, Gttstein B, Stinglin Y, Eckri J. Immunodiagnosis of toxocarosis in humans: evaluation of a new enzyme-linked immunosorbent assay kit. J Clin Microbiol. 1991. 29:1831–1835.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download