Abstract
Extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue (MALT lymphoma) is usually indolent. Although it was reported recently that about 20-30% cases of MALT lymphoma presented with a disseminated disease at diagnosis, it was described as a disease localized at diagnosis and remaining stable for a prolonged period. However, only a few cases of MALT lymphoma involved the lung and gastrointestinal tract all at once. We report a case of a 73-year-old man with disseminated MALT lymphoma. He presented with non-productive cough, initial chest radiograph showed a nodule in the right lower lobe.
The diagnosis of stage IV MALT lymphoma was made by CT scan, video-assisted thoracoscopic excisional biopy, gastrofiberscopic biopsy and bone marrow biopsy. The lymphoma involved the lung, stomach and bone marrow at the time of diagnosis. Because he refused chemotherapy, he discharged after Helicobacter pylori eradication without chemotherapy. Regular follow-up examination did not show any evidence of disease progression over 22 months.
Figures and Tables
Figure 2
Chest CT scan shows a 3.3 × 1.7cm sized nodule with spiculated margin in anterior basal segment of right lower lobe.
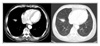
Figure 3
Gastrofibroscopy shows 2.0 and 1.5cm sized elevated, central depressed lesions with mucosal irregularity on the great curvature and lesser curvature of the lower body.
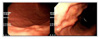
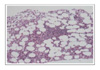
Figure 4
Pathologic findings of the lung nodule (A) The neoplastic lymphoid cells efface pulmonary architecture (H&E × 40). (B) The extranodal marginal zone B cell lymphoma of MALT consists of centrocyte like cells, monocytoid cells and lymphoepithelial lesion (H&E × 100).

Figure 5
Immunohistochemical stain of the lung nodule (A) The CK7 stain reveals lymphoepithelial lesion (× 100). (B) The stain for CD20 shows shows strong positive reaction in tumor cells (× 100).

References
1. Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin's lymphomas: part 1. gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997. 8:727–737.
2. Isaacson P, Wright DH. Extranodal malignant lymphoma arising from mucosa-associated lymphoid tissue. Cancer. 1984. 53:2515–2524.
3. Raderer M, Vorbeck F, Formanek M, Österreicher C, Valencak J, Penz M, et al. Importance of extensive staging in patients with mucosa-associated lymphoid tissue (MALT)-type lymphoma. Br J Cancer. 2000. 83:454–457.
4. Thieblemont C, Berger F, Dumontet C, Moullet I, Bouafia F, Felman P, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed. Blood. 2000. 95:802–806.
5. Graziadei G, Pruneri G, Carboni N, Luminari S, la Targia M, Neri A, et al. Low-grade MALT lymphoma involving multiple mucosal sites and bone marrow. Ann Hematol. 1998. 76:81–83.
6. Moon CM, Kim HM, Choi JW, Seo JH, Won SY, Lee CG, et al. A case of mucosa-associated lymphoid tissue lymphoma in the esophagus accompanied by bronchus-associated lymphoid tissue lymphoma. Korean J Gastrointest Endosc. 2003. 27:137–142.
7. Bae JY, Na HS, Choi JS, Choi JH, Park SG, Jang AS, et al. A case of primary mucosa-associated lymphoid tissue lymphoma of the trachea and colon. Tuberc Respir Dis. 2005. 59:193–197.
8. Isaacson P, Wright DH. Malignant lymphoma of mucosa-associated lymphoid tissue: a distinctive type of B-cell lymphoma. Cancer. 1983. 52:1410–1416.
9. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JKC, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994. 84:1361–1392.
10. Kim JH, Kim WS, Ko YH, Song SY, Oh SY, Kim KH, et al. Clinical investigation of gastric MALT lymphoma. Korean J Med. 2001. 61:417–423.
11. Oh SY, Kim WS, Kim JH, Song SY, Kim KH, Nam EM, et al. Extra-gastric MALT lymphoma: analysis of 50 cases. Korean J Med. 2000. 59:261–267.
12. Jee SR, Seol SY. Low-grade mucosa-associated lymphoid tissue lymphoma of stomach. Korean J Gastroenterol. 2005. 45:312–320.
13. Tsang RW, Gospodarowicz MK, Pintilile M, Bezjak A, Wells W, Hodgson DC, et al. Stage I and II MALT lymphoma: results of treatment with radiotherapy. Int J Radiat Oncol Biol Phys. 2001. 50:1258–1264.
14. Hitchcock S, Ng AK, Fisher DC, Silver B, Bernardo MP, Dorfman DM, et al. Treatment outcome of mucosa-associated lymphoid tissue/marginal zone non-Hodgikin's lymphoma. Int J Radiat Oncol Biol Phys. 2002. 52:1058–1066.
15. Zinzani PL, Stefoni V, Musuraca G, Tani M, Alinari L, Gabriele A, et al. Fludarabine-containing chemotherapy as frontline treatment of nongastrointestinal mucosa-associated lymphoid tissue lymphoma. Cancer. 2004. 100:2190–2194.
16. Horning SJ, Rosenberg SA. The natural history of initially untreated low-grade non-Hodgkin's lymphomas. N Engl J Med. 1984. 311:1471–1475.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download