Abstract
Background
A spirometric reference equation was recently developed for the general population in Korea. The applicability of the new Korean equation to clinical practice was examined by comparing it with the Morris equation, which is one of the most popular reference equations used for interpreting the spirometric patterns and for grading the disease severity in Korea.
Methods
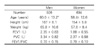
Spirometry was performed on 926 men and 694 women, aged 20 years or older, in November 2004 at the Asan Medical Center, Seoul, Korea. The subjects' age, gender, height, weight, and spirometric values (FEV1 [forced expiratory volume in one second], FVC [forced vital capacity], and FEV1/FVC) were obtained. The spirometric patterns and disease severity were evaluated using both equations, and the results of the Korean equation were compared with the Morris equation. The spirometric patterns were defined as normal, restrictive, obstructive, and undetermined according to the level of FEV1/FVC and FVC. The disease severity was defined according to the level of FEV1 level for subjects with an airflow limitation, and according to the FVC level for those subjects without an airflow limitation.
Results
Spirometric patterns were differently interpreted in 22.5% (208/926) of the men and 24.8% (172/694) of the women after the application of the Korean equation compared with the Morris equation. Of the subjects with airflow limitation, disease severity was differently graded in 30.2% (114/378) of the men and 39.4% (37/94) of the women after the application of the Korean equation. Of the subjects without airflow limitation, disease severity was differently graded in 27.9% (153/548) of the men and 30.2% (181/600) of the women after the application of the Korean equation.
Figures and Tables
 | Figure 1Effect of different reference equations on the interpretation of spirometric patterns. Spirometric patterns were differently interpreted after the change in reference equation from the Morris to the new Korean equation (P<0.001 in both males and females by the chi-square test). Definition: normal pattern, FEV1/ FVC ≥0.7 & FVC ≥80% predicted value; restrictive pattern, FEV1/FVC ≥0.7 & FVC <80% predicted value; obstructive pattern, FEV1/FVC <0.7 & FVC ≥80% predicted value; undetermined pattern, FEV1/FVC <0.7 & FVC <80% predicted value. The number inside each block represents the number of subjects showing each spirometric pattern. |
 | Figure 2Effect of different reference equations on disease severity in subjects with airflow limitation (FEV1/FVC <0.7). Disease severity was differently interpreted after the change in reference equation from the Morris to the new Korean equation (P<0.001 in both males and females by the chi-square test). Disease se verity was defined as mild, moderate, severe, and very severe according to FEV1 (% predicted value) of ≥80%, <80% & ≥50%, <50% & ≥30%, and <30%, respectively. The number inside each block represents the number of subjects showing each grade of disease severity. |
 | Figure 3Effect of different reference equations on disease severity in subjects without airflow limitation (FEV1/FVC ≥0.7). Disease severity was differently interpreted after the change in reference equation from the Morris to the new Korean equation (P<0.001 in both males and females, by the chi-square test). Disease severity was defined as mild, moderate, and severe according to FVC (% predicted value) of <80% & ≥60%, <60% & >50%, and ≤50%, respectively. The number inside each block represents the number of subjects showing each grade of disease severity. |
References
1. Gold WM. Murray JF, Nadel JA, editors. Pulmonary function testing. Textbook of respiratory medicine. 2000. 3rd ed. W.B. Philadelphia: Saunders;781–881.
2. American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991. 144:1202–1218.
3. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry for Korean population. Tuberc Respir Dis. 2005. 58:230–242.
4. Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971. 103:57–67.
5. American Thoracic Society. Standardization of Spirometry: 1994 update. Am J Respir Crit Care Med. 1995. 152:1107–1136.
6. Global initiative for chronic obstructive lung disease: global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. National Heart, Lung, and Blood Institute and World Health Organization. revised 2003; cited 20 August 2004. Bethesda, MD, USA: National Heart, Lung, and Blood Institute, National Institutes of Health;Available from: URL:
http://www.goldcopd.com.
7. American Medical Association. Guides to the evaluation of permanent impairment. 1993. 4th ed. Chicago: American Medical Association.
8. Standards for the diagnosis and treatment of patients with chronic obstructive pulmonary disease. American Thoracic Society and European Respiratory Society. cited 10 June 2004. New York, USA: American Thoracic Society;Available from URL:
http://www.thoracic.org/COPD/.
9. Dykstra BJ, Scanlon PD, Kester MM, Beck KC, Enright PL. Lung volumes in 4,774 patients with obstructive lung disease. Chest. 1999. 115:68–74.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download