Abstract
Background and Objectives
The rigid coupling between the delivery wire and the right atrial disk has been occasionally encountered during transcatheter closure of atrial septal defect (ASD). Therefore the device frequently makes a perpendicular angle, and the leading edge of left atrial disk slips through the defect and prolapses into right atrium (RA) before it is properly placed in the septum. The purpose of this study is to investigate relating factors to the need of technical modification in transcatheter closure of large ASD and to evaluate relevant morphologic characteristics of atrial septal rim in this situation.
Subjects and Methods
From July, 2003 to May, 2007, 312 patients underwent transcatheter occlusion of ASD with Amplatzer Septal Occluder® (ASO, AGA medical corporation, Golden Valley, MN, USA) at Yonsei Cardiovascular Center and among them 109 patients had large ASD (≥25 mm) and these patients were enrolled in our study. Patients were divided into two groups according to the deploying methods of the device (Group I: standard method, Group II: modified methods). Assessments of the defects and its surrounding rims were made by echocardiography.
Results
There were no differences between 2 groups in age, body weight and height except for balloon-stretched diameter (stop-flow technique) and device size. Group II patients with modified methods showed larger balloon-stretched diameter and device size than group I patients with standard method. The mean length of anterosuperior (AS) rim in group II was significantly shorter than group I (p<0.05). As the size of the device used in procedure increased, there was a trend towards increase in the need of modified methods.
Conclusion
This study shows that AS rim deficiency and the size of ASD may be the relating factors to the need of technical modification in transcatheter closure of ASD. Therefore, when the initial try with standard method is not successful in large ASD with deficient AS rim, we suggest that changing strategy of implantation may save time and efforts and possibly reduce the risk of complications associated with prolonged procedure.
Transcatheter closure of secundum atrial septal defect (ASD) with Amplatzer Septal Occluder® (ASO, AGA medical corporation, Golden Valley, MN, USA) has become an effective and reliable alternative therapy to operation in most patients with ASD.1-6) Compared with surgical repair, transcatheter closure is safer and more physiologic, and the treatment results are similar, and as a result, transcatheter closure has surfaced to replace operation in recent years.3-5)
Owing to its design, the ASO can even be used in patients with large ASD associated with deficient rims. However, the major problem in closing a large ASD is malalignment of the device to the plane of defect. The delivery system of AGA Amplatzer has a rigid coupling between the delivery wire and the right atrial disk, which accounts for the relatively perpendicular orientation of the left atrial disk to the atrial septal plane.7)8) This character of the device results in the prolapse of the left atrium (LA) disk to right atrium (RA) during deployment (Fig. 1). There have been many efforts to overcome limitations derived from the inherent design of the ASO delivery system and many have succeeded using technical modifications.9-13) The purpose of this study is to investigate the relating factors to the need of technical modification in transcatheter closure of large ASD (≥25 mm) and to evaluate the relevant morphologic characteristics of atrial septal rim in these patients.
A total of 312 patients underwent transcatheter occlusion of secundum ASD with ASO at Yonsei Cardiovascular Center from July, 2003 to May, 2007. Among them, 109 (35%) patients (male 34; female 75) had more than 25 mm sized ASD and these patients were enrolled in the study. The patients were divided by the methods of deployment of ASO into two groups as group I, standard method group, and group II, modified method group. When the initial attempt of standard method failed, modified method was applied.
Assessments of the defects were measured by balloon-occlusive diameter (BOD) and its surrounding rims were based on transesophageal or intracardiac echocardiography, performed at the time of closure. The measurement of defect size based on BOD was performed according to the previous report.14) The analysis of the echocardiographic studies were performed according to the recommendations of the American Society of Echocardiogrphy.15) Echocardiographic studies were performed and images were acquired and digitally stored for offline analysis with each study by experienced physicians. Anteroinferior (AI) rim was measured as the distance to atrioventricular valve, posterosuperior (PS) rim was measured as the distance to superior vena cava, posteroinferio (PI) rim was measured as the distance to inferior vena cava, and anterosuperior (AS) rim was measured as the distance to aortic posterior wall. The two total septal lengths, anteroposterior septal length (APSL) and superoinferior septal length (SISL) was also measured and calculated. APSL was the total length between PS, ASD, and AI, and SISL was the total length between PI, ASD, and AS. AS rim was measured in the short-axis view, PS and PI rims were measured in the long-axis view or the bicaval view. AI rim was measure in 4-chamber view. In some of the cases, combinations of different views were used to determine the rim length. Any rim length was considered deficient if its length was less than 5 mm (Fig. 2).
The profiles of the enrolled patients are summarized in Table 1. The mean age of the patients in group I was 34.7±15.5 years, 24 were male and 50 were female, the mean weight was 56±13.2 kg, the mean height was 158.8±13.1 cm, and the mean body surface area (BSA) was 1.55±0.24 kg/m2. The mean age of patients in group II was 32.9±13.6 years, 10 were male and 25 were female, the mean weight was 56.4±12.0 kg, the mean height was 159.2±12.9 cm, and the mean BSA was 1.58±0.23 kg/m2. The mean BOD size in group I and group II were 29.4±4.1 mm and 32.2±3.8 mm, respectively. The mean device size in group I was 29.4±4.0 mm and the mean device size in group II was 32.3±3.44 mm. The Qp/Qs in group I and II were 2.35±0.63 and 2.63±0.94, respectively. There were no differences between the 2 groups in age, body weight, sex ratio, and height. Group II showed a larger BOD and device size, which was statistically significant (p<0.01). Qp/Qs ratio in group II was larger than group I, but it wast statistically insignificant. In the 35 patients who underwent modified techniques, 21 patients underwent right upper pulmonary vein (RUPV) technique,9) 9 patients underwent left upper pulmonary vein (LUPV) technique,7) 3 patients underwent dilator assisted technique,16) and 2 patients underwent balloon-assisted technique.10)
The morphologic characteristics of the atrial septal rim in the enrolled patients are shown in Table 2. In group I, the mean PS rim length was 13.1±4.9 mm, the mean AI rim length was 15.5±5.3 mm, the mean PI rim length was 11.2±6.1 mm, and the mean AS rim length was 6.4±4.1 mm. In group II, the mean PS rim length was 12.7±4.3 mm, the mean AI rim length was 13.5±4.3 mm, the mean PI rim length was 12.7±4.2 mm, and the mean AS rim length was 2.5±2.6 mm. The mean length of AS rim in group II was significantly shorter than group I (p<0.01), but none of the other parameters showed significant difference. The mean APSL in group I and group II were 51.3±7.6 mm and 51.7±8.1 mm, respectively, and the mean SISL in group I and group II were 63.1±8.9 mm and 66.2±10.2 mm, respectively. Both APSL and SISL did not show any statistical difference between both groups.
In group I with standard method, 48 patients (65%) had central defect and 20 patients (27%) had AS defect, shown in Fig. 3A. In group II with modified method, only 6 patients (17%) had central defect, whereas 22 patients (63%) had AS defect, shown in Fig. 3B. In both groups I and II, 54 patients had central defect and 42 patients had AS defect. When the patients with ASD had sufficient rims, 87% of procedure was successfully performed by standard method and 13% needed modified technique, but with AS rim deficiency, modified techniques were needed in 53% of the procedures (Fig. 4). Furthermore, as the size of the device used in the procedure increased, there was a tendency towards increase in the frequency of use of modified methods (Fig. 5).
Many factors contribute to the difficulty involved in transcatheter closure of large secundum ASD. Over the course of time, alternative techniques of device deployment have improved, making more ASD amendable using ASO, but they still remain a challenge.
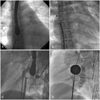
Numerous alternative techniques have been reported to facilitate transcatheter closure of large secundum ASDs,11) and our institute utilizes many of the reported modified techniques. The LUPV technique (Fig. 6A), which can be used in both children and adults, is engagement of LA disk within LUPV, followed by a rapid release of the waist and RA disk.7) The RUPV technique (Fig. 6B), recommended, but not limited, to larger patients, is partial deployment of LA disk in RUPV while maintaining contact with the posterior superior septum, followed by quick and successive deployment of the waist and RA disk.9) In the above 2 methods, it is important to place the LA disk exactly in pulmonary vein and the procedure must be performed with gentle movements until the deployment of RA disk, to avoid damage to the atrial wall. Dilator assisted technique, also known as Wahab technique (Fig. 6C), is using a long dilator, usually the delivery sheath being used, to hold the LA disk inside LA, preventing it from prolapsing across the defect.16) The balloon-assisted technique (Fig. 6D), first describe by Dalvi et al.10) in 2005, has a concept similar to the Wahab technique, but uses the balloon catheter to support the LA disk from prolapsing across the defect. These 4 techniques are the most popular modified techniques used and they were used in our patients who were enrolled in the study. In our institute, the RUPV method is the most frequently applied technique.
Our study revealed that the proportion of AS rim deficiency was higher in patients with modified methods, modified methods were needed more frequently in large-sized ASD. Therefore it demonstrated that AS rim deficiency and the size of ASD may be the core relating factors to the need of technical modification in transcatheter closure of ASD. There have been many studies describing the different modified techniques used in large ASDs,7)9)10)16) but our study is the first to analyze the factors involved in the decision of whether to employ the modified technique or not. With the prediction of a possible need of modified technique, the interventionist may be able to prepare, prior to the procedure, which may increase the success rate of the procedure. Also, by preparing, the procedure time may be reduced, which in result may moderate the complications engaged with long procedure time.
Our study was limited to patients of a single institute and only limited interventionists were involved. Further investigation with a larger pool of patients involving diverse interventionists with different techniques is pertinent in the future.
In conclusion, our study revealed that AS rim deficiency and the size of ASD may be the 2 most important relating factors to the need of technical modification in transcatheter closure of ASD. Therefore, when the initial attempt with standard method is not successful, we suggest that changing strategy of implantation may save time and efforts and possibly reduce the risk of complications associated with prolonged procedure.
Figures and Tables
Fig. 1
Diagram showing the relationship between atrial septum and device. The prolapse of left atrial disk during deployment can be observed. SVC: superior vena cava, PV: pulmonary vein, IVC: inferior vena cava, CS: coronary sinus, AAo: ascending aorta, TV: tricuspid valve.

Fig. 2
Two dimensional echocardiography findings. A: diagram showing the measuring locations of septal rims. B, C and D: measurements of the rims with transesophageal echocardiography (TEE). Using the still images obtained by TEE, the rim lengths were measured in the modified 4 chamber view and the short axis view. E and F: measurements of the rims with intracardiac echocardiography (ICE). Using the still images obtained by ICE, the rim lengths were measured in the short axis view and the long axis view. SVC: superior vena cava, PS: posterosuperior rim, ASD: atrial septal defect, AS: anterosuperior rim, AAo: ascending aorta, PI: posteroinferio rim, AI: anteroinferior rim, CS: coronary sinus, IVC: inferior vena cava, LA: left atrium, LV: left ventricle, RV: right ventricle.

Fig. 3
Anatomical characteristics of defects according to deployment methods. A: in group I with standard method, 48 patients (65%) had central defect and 20 patients (27%) had anterosuperior (AS) defect. B: in group II with modified method, only 6 patients (17%) had central defect, whereas 22 patients (63%) had AS defect. PS: posterosuperior, AI: anteroinferior, PI: posteroinferior.
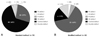
Fig. 4
The different deployment method in atrial septal defect (ASD) patients with central defect and anterosuperior (AS) rim defect. With sufficient rims, 87% of procedure was successfully performed by standard method and 13% needed modified technique, but with AS rim deficiency, modified techniques were needed in 53% of the procedure.

Fig. 5
The different deployment method according to employed device size. As the size of the device used in the procedure increased, there was a tendency towards increase in the frequency of use of modified methods.

References
1. Rao PS. Catheter closure of atrial septal defects. J Invasive Cardiol. 2003. 15:398–400.
2. Ebeid MR. Percutaneous catheter closure of secundum atrial septal defects: a review. J Invasive Cardiol. 2002. 14:25–31.
3. Berger F, Vogel M, Alexi-Meskishvili V, Lange PE. Comparison of results and complications of surgical and Amplatzer device closure of atrial septal defects. J Thorac Cardiovasc Surg. 1999. 118:674–678. discussion 678-80.
4. Chessa M, Carminati M, Butera G, et al. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol. 2002. 39:1061–1065.
5. Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol. 2002. 39:1836–1844.
6. Spies C, Hijazi ZM. Transcatheter closure of secundum atrial septal defects in the elderly. Korean Circ J. 2009. 39:47–51.
7. Varma C, Benson LN, Silversides C, et al. Outcomes and alternative techniques for device closure of the large secundum atrial septal defect. Catheter Cardiovasc Interv. 2004. 61:131–139.
8. Aeschbacher BC, Chatterjee T, Meier B. Transesophageal echocardiography to evaluate success of transcatheter closure of large secundum atrial septal defects in adults using the buttoned device. Mayo Clin Proc. 2000. 75:913–920.
9. Berger F, Ewert P, Dhnert I, et al. Interventional occlusion of atrial septum defects larter than 20 mm in diameter. Z Kardiol. 2000. 89:1119–1125.
10. Dalvi BV, Pinto RJ, Gupta A. New technique for device closure of large atrial septal defects. Catheter Cardiovasc Interv. 2005. 64:102–107.
11. Fu YC, Cao QL, Hijazi ZM. Device closure of large atrial septal defects: technical considerations. J Cardiovasc Med (Hagerstown). 2007. 8:30–33.
12. Kutty S, Asnes JD, Srinath G, Preminger TJ, Prieto LR, Latson LA. Use of a straight, side-hole delivery sheath for improved delivery of Amplatzer ASD occluder. Catheter Cardiovasc Interv. 2007. 69:15–20.
13. Staniloae CS, El-Khally Z, Ibrahim R, Dore A, De Guise P, Mercier LA. Percutaneous closure of secundum atrial septal defect in adults a single center experience with the Amplatzer septal occluder. J Invasive Cardiol. 2003. 15:393–397.
14. Zhu W, Cao QL, Rhodes J, Hijazi ZM. Measurement of atrial septal defect size: a comparative study between three-dimensional transesophageal echocardiography and the standard balloon sizing methods. Pediatr Cardiol. 2000. 21:465–469.
15. Douglas PS, DeCara JM, Devereux RB, et al. Echocardiographic imaging in clinical trials: American Society of Echocardiography Standards for echocardiography core laboratories: endorsed by the American College of Cardiology Foundation. J Am Soc Echocardiogr. 2009. 22:755–765.
16. Wahab HA, Bairam AR, Cao Q, Hijazi ZM. Novel technique to prevent prolapse of the Amplatzer septal occluder through large atrial septal defect. Catheter Cardiovasc Interv. 2003. 60:543–545.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download