Abstract
Figures and Tables
Figure 1
A, Panoramic radiograph acquired before marsupialization of the cyst. B, Pretreatment computed tomographic images acquired before marsupialization of the cyst.
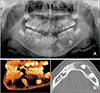
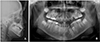
Figure 2
A, Panoramic radiographs acquired 3 months after the initiation of marsupialization of the cyst. B, Panoramic radiographs acquired 9 months after the initiation of marsupialization of the cyst. C, Computed tomographic images acquired 9 months after the initiation of marsupialization showing a reduction in the size of the cyst. D, Schematic illustration of the impacted teeth during marsupialization of the cyst.

Figure 6
A, A removable appliance design. Six hooks were added to the appliance to control the direction of the force. B, Intraoral photographs showing treatment progress with a removable appliance. C, After 6 months of wearing the removable appliance.

Figure 7
A, Intraoral photographs showing treatment progress with fixed orthodontic appliances. B, After correcting the axis of the distally tipped mandibular incisors and obtaining space for the restoration of the mandibular left second premolar.

Figure 10
A, Posttreatment lateral cephalogram. B, Superimpositions before and after orthodontic treatment. C, Posttreatment panoramic radiograph.

Figure 11
Post-retention radiographs acquired 2.5 years after debonding. A, Lateral cephalogram; B, panoramic radiograph.

Table 1
Results of the cephalometric analyses before and after orthodontic treatment
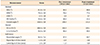
SNA, Angle of the lines connecting sella, nasion, and point A; SNB, angle of the lines connecting sella, nasion, and point B; ANB, angle of the lines connecting point A, nasion, and point B; SN, the plane formed by sella and nasion; GoGn, the plane formed by gonion and gnathion; U1, upper central incisor; L1, lower central incisor; E line, a line drawn from pronasale to soft tissue pogonion.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download