Abstract
Background
Caudal block is a common technique in children for reducing postoperative pain, and there have been several reports on the variations of the sacral canal in children. However, previous studies have mainly focused on the needle trajectory for caudal block, and there is limited information on the structural variations of the sacrum in children. The purpose of this study was to analyze the anatomic variations of sacral canals in children.
Methods
Three-dimensional computed tomographic images were analyzed. The data from the images included ① fusion of the sacral vertebral laminae and the sacral intervertebral space ② existence of the sacral cornua and ③ the types of sacral hiatus. The types of sacral hiatus were classified into 3 groups: group I (fusion of S3 or S4 vertebral laminae), group II (unfused vertebral arch with the distance of the S3 and S4 vertebral laminae < 50% of the distance between the cornua), and group III (unfused vertebral arch with the distance of the S3 or S4 vertebral laminae ≥ 50% of the distance between the cornua).
Results
A total of 143 children were included in this study. All of the sacral vertebral arches were not fused in 22 children (15.4%). Cornua were not identified bilaterally in 5 (3.5%) and unilaterally in 6 (4.2%) children. In the sacral hiatus, group II and group III were identified in 22 (15.4%) and 31 (21.7%) children, respectively.
Caudal epidural block is a procedure that is commonly performed as anesthesia for an operation and as postoperative pain control in children [1,2]. The procedure has been known to have a high success rate and a low risk of complications in comparison to other neuraxial block procedures which can be performed in children [1,3]. However, many studies conducted with adults and children have shown that there are many variations in important anatomical structures for the procedure [4,5,6,7]. These variations increase the difficulty of the procedure and increase the risk of complications. In addition, the sacrum of children is at an immature stage where ossification has not yet been completed [8], and a severe complication such as dural puncture could take place if those who perform the procedure fail to recognize the variations.
Until now, anatomical investigation for caudal epidural block in children has been performed by means of fetal cadaver [5] and MRI [9]. However, both of the studies did not consider the development process of the sacral canal depending on the age of the children and only focused on the optimal needle trajectory for effective caudal epidural block. In addition, studies have never been conducted either on the assessment of risk for caudal epidural block according to the characteristics of children's sacrum or on the analysis of the sacral canal with 3-dimensional computed tomography (3D-CT) images for caudal epidural block. In this study, 3D-CT images of Korean children were used to investigate the anatomical variation of the sacrum.
This study was conducted after acquiring the approval of the IRB with which the authors are affiliated with (IRB No. B-1311/228-112). The subjects of this study were the patients under the age of 18 who underwent 3D hip CT or pelvis CT at our institution between January 2010 and October 2013. Among the patients, those who had a fracture or tumor invasion to the sacrum or those whose 3D image resolution was low were excluded from this study. The CT images were reconstructed with a 3D image reconstruction system (Rapidia™, Infinite healthcare Co., Ltd, Seoul, Korea), and the resulting images were obtained through the Picture Archiving and Communication System.
First, existence of the sacral cornua (Fig. 1 'D' and 'E') was verified in the sacral bone images (Fig. 1) reconstructed by 3D-CT. When the sacral cornua were not identified in the 3D-CT images, the superior articular process of the 5th sacral vertebra (S5), which would become a sacral cornu later, was identified in the sagittal view. When the S5 superior articular process was indistinguishable from the posterior margin of the S5 body, it was defined as 'sacral cornua nonexistence.' Next, the distance between the sacral cornuae (DSC) was measured ('A' line in Fig. 1) to verify the midline fusion of the S3 and S4 lamina. If there was no fusion, the distance between sacral laminae (DSL) was measured ('B' line in Fig. 1). Finally, the fusion of the S1/2 and S2/3 sacral intervertebral spaces ('C' line in Fig. 1) was checked. Busoni and Sarti [10] introduced the epidural block through the S2/3 sacral intervertebral space before fusion in the sacrum in 1987 and named the procedure as "sacral intervertebral epidural block." Based on this finding, the fusion of the S2/3 sacral intervertebral space ('C' line in Fig. 1), and the related fusion of the S1/2 sacral intervertebral space were also verified.
Assuming that the risk of caudal block may be dependent on the types of sacral hiatus, the distance between the S3 vertebral arches or between the S4 vertebral arches was compared with the DSC in the 3D-CT images to classify the structural variations of the sacrum with reference to the following criteria (Fig. 2):
In addition, considering the previous result that the incidence of spinal bifida occulta was high in the patients with cerebral palsy [11], patients diagnosed with cerebral palsy were separated from patients without cerebral palsy to classify the structural variations of the sacrum.
IBM SPSS statistics® version 17.0 (IBM Corporation, NY, USA) was used for the statistical analysis. A linear by linear association test was performed to analyze the degree of lamina fusion in each age group. The difference in the structural variations of the sacrum between the patients with and without cerebral palsy was analyzed with the χ2 test. Statistical significance was defined as P < 0.05.
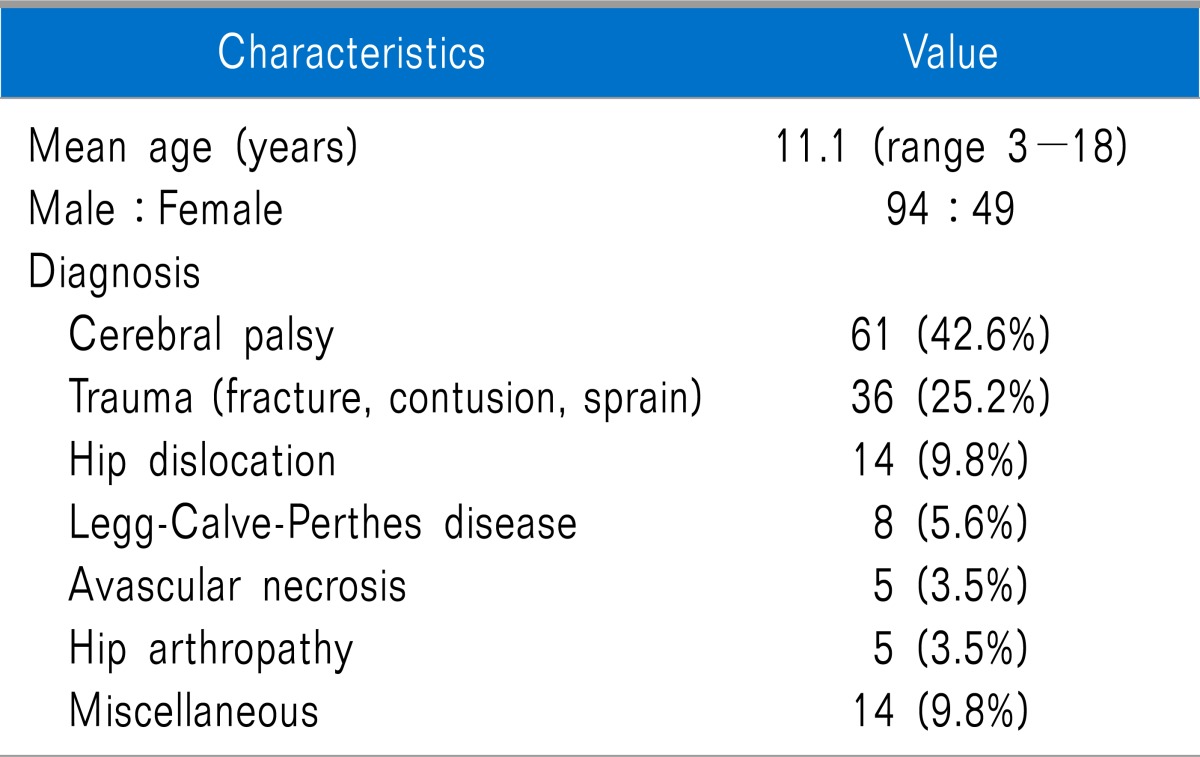
Among 162 young children, 6 patients were excluded because the sacrum could not be identified due to fracture or tumor invasion of the sacrum. Thirteen patients were excluded because the 3D images to be used in the study had not been reconstructed, or the resolution of the images was too low to analyze. Finally, 143 patients were included in this study. Table 1 shows the demographic data of the patients.
Among the 143 subjects, the number of patients who had no fusion in all the S1-4 vertebral laminae was 22 (15.4%), and their mean age was 7.6 (ranging from 3 to 16) years. The number of patients who had fusion in all the S1-4 vertebral laminae was 30 (21.0%), and their mean age was 13.3 (ranging from 3 to 18) years. The number of patients who had fusion in all the sacral vertebral laminae and intervertebral spaces was 14 (9.8%), and their mean age was 14.9 (ranging from 12 to 18) years. Among the 143 patients, L5 vertebral laminae were fused in all patients. The sacral cornua were not identified on both sides in 5 patients, and were identified on only one side in 6 patients.
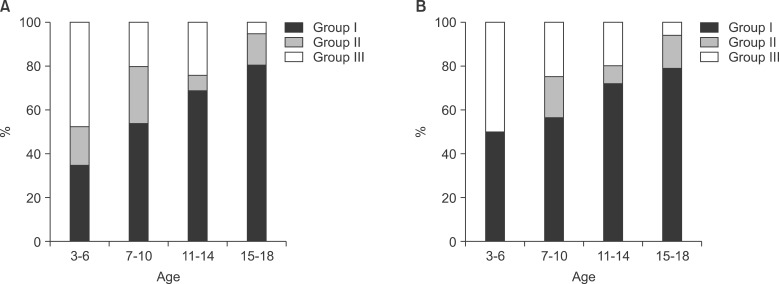
According to the fusion status of sacral laminae, the number of patients in Group 1 was 90 (62.9%), 22 (15.4%) in Group II, and 31 (21.7%) in Group III. As the age increased, the number of patients in Group 1 increased (Fig 3A, P = 0.040).
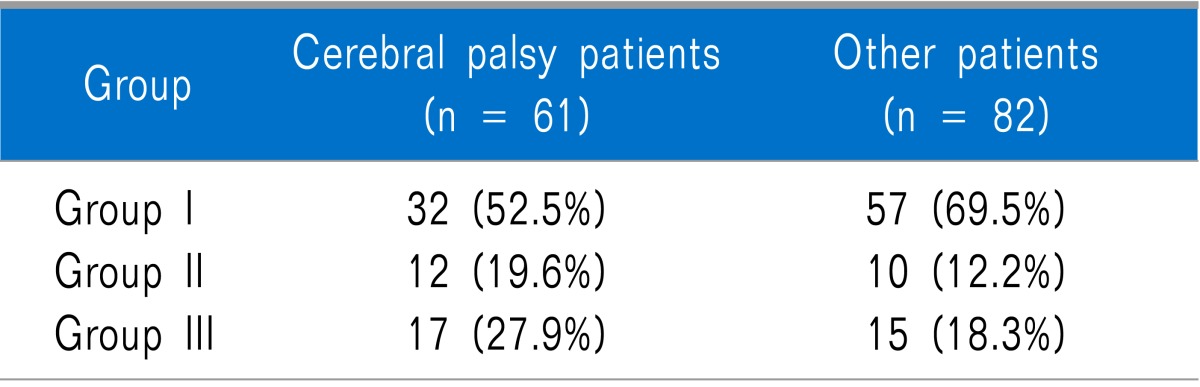
Considering the previous study result that the incidence of spinal bifida occulta was higher in the patients with cerebral palsy patients than those of a normal population [11], the patients diagnosed with cerebral palsy were separated from the patients without cerebral palsy to classify the sacral hiatus type (Table 2). However, the distribution of the sacral hiatus types was not significantly different between patients with and without cerebral palsy in our study (P = 0.123). Even in the patients without cerebral palsy, there were the patients whose sacrum was not fused; the number of patients in Group II was 10 (12.2%) and 15 (18.3%) in Group III, indicating that some of the patients without cerebral palsy did have the non-fused sacrum. Additionally, in the patients without cerebral palsy, the number of patients in Group 1 was higher (Fig 3B, P = 0.032), as the age increased.
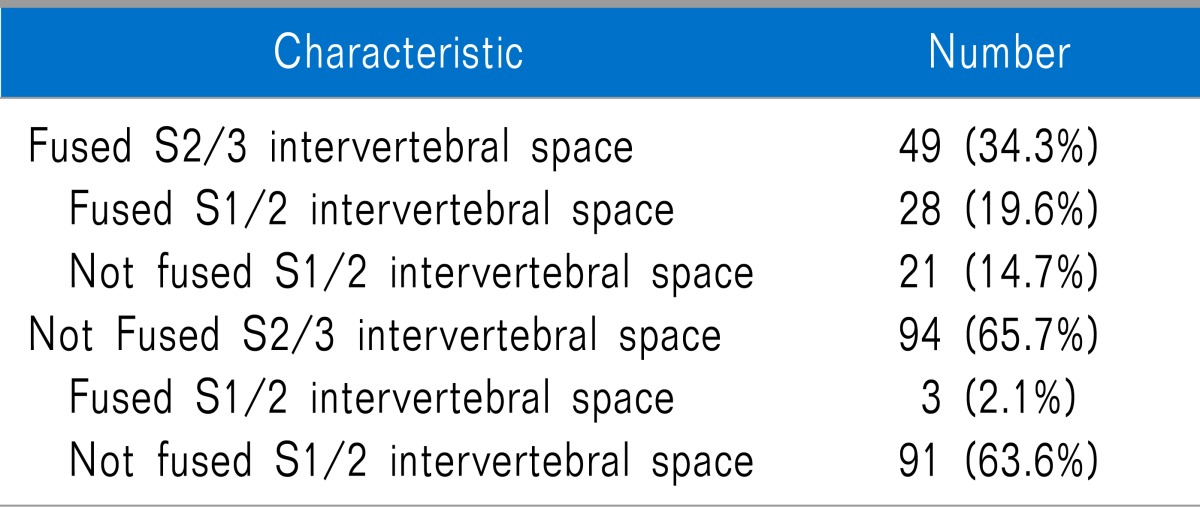
With respect to the fusion of the sacral intervertebral space, the fusion of all the segments was not complete in 80 patients out of 143 patients (56.0%), while the fusion was complete in 16 patients (11.2%). Table 3 shows the classification of the patients with reference to the S2/3 intervertebral space fusion. In addition, 49 (34.3%) out of the 143 patients showed the fusion of the S2/3 intervertebral space which was necessary for sacral intervertebral block.
Caudal epidural block is a procedure commonly performed in children for surgeries or pain control in the low extremities. In most cases, caudal epidural block is simply performed with a blind method, often palpating the sacral hiatus and perforating the sacrococcygeal ligament covering the sacral hiatus [12]. It was reported that the apex of sacral hiatus is at the S4 level in 68.42% of adults and at the S3 level in 97.36% of adults [4].
The anatomical structure of the lumbosacral epidural canal in children is quite different from that of adults. In the early postnatal period, the sacrum consists of five vertebrae. In this period, the sacrum has a shape similar to that of the lumbar spine, and the fusion of the sacrum is complete at an age between 25 and 30 [10]. In other words, ossification is not complete in the sacrum even at a level higher than the S3/4 level; thus, there is a space through which the sacral canal may be accessed. Therefore, when a needle is inserted through the space, the distance between the needle and the dural sac becomes shorter than the distance when the needle is inserted through the sacral hiatus. Moreover, the distance between the dural sac and the sacrococcygeal ligament is shorter in children than in adults, and the risk of dural puncture is higher when a needle is inserted at a high level.
Aggarwal et al. [5] reported in a study conducted with 39 fetal cadavers that the terminal of the dural sac was most frequently at the S2 level (58.97%), followed by the S3 level (12.82%). In addition, they reported that the apex of sacral hiatus was observed most frequently at the S3 level, indicating that the distance between the apex of the hiatus and the dura was only 3 to 13 mm. Shin et al. [13] conducted a study with 317 young patients under anesthesia with ultrasonography and reported that the dural sac level was at the upper S2 level on average and at a level below the S2 and S3 levels in 7.57% of the young patients. Therefore, it may be presumed that fusion of the vertebral arch at the S3 level has a significant effect on the risk of inadvertent dural puncture caused by the cephalad insertion of a needle.
In this study, the sacral hiatus types were classified with reference to the potential risk of dural puncture which may take place during caudal epidural block. Group I included the patients who had the fusion of the S3 or S4 vertebral arch and thus the lowest possibility of inadvertent dural puncture because the needling point is determined at the level of the S3 level or lower. Group II included the patients whose sacral hiatus apex was open. Although dural puncture may take place if a needle is inserted through the opened sacral hiatus apex, the distance between the vertebral arches of S3 or S4 is shorter than that of Group III. Hence, the possibility of a needle insertion through the opened sacral hiatus apex was relatively low, and the distance between the vertebral arches becomes shorter, moving to the cephalad. Therefore, Group II has a lower risk in comparison to Group III in that those who perform the procedure may predict the position of the sacral hiatus apex. Group III included patients whose distance between the vertebral arches of S3 or S4 was longer than that of Group II, and thus, a needle may be inserted into the space more easily, and the precise position of the sacral hiatus apex may not be easily identified by those who perform the procedure. Therefore, Group III has the highest risk of inadvertent dural puncture. In this study, the number of patients in Group III was 31 (21.7%). Even among the patients without cerebral palsy, the number of patients in Group III was 15 (18.3%). As mentioned above, because the sacral bone ossification progresses over age, the number of patients in Group I increased as the age increased.
In their study using 114 dry sacral bones, Aggarwal et al. [4] measured the position of the sacral hiatus apex and reported that the position was at S4 in 68.42% of the subjects, at S3 in 14.03%, and at S2 in 2.64%. Sekiguchi et al. [6] also conducted a similar study and reported that the position of the sacral hiatus was at S4 in 65% of the subjects, S3 in 15%, S2 in 4%, and S1 in 1%. In our study, the proportion of patients who showed fusion of the S4 vertebral arch (which forms the apex of the sacral hiatus later at the S4 level) was 28%. The result was different from that of Aggarwal et al. because the ossification of the young aged patients was incomplete; and thus, the sacral hiatus formation was not complete in our study. In other words, the rate of ossification was different from patient to patient in our study: one 3-year old patient showed fusion of all the vertebral arches and complete formation of the sacral hiatus while a 16-year old patient showed no fusion of any vertebral arches.
Busoni and Sarti [10] firstly introduced epidural block through the sacral intervertebral space of the sacrum before fusion, and a couple of studies were conducted in this regard [14,15]. In this method, a line connecting the posterior superior iliac spine on both sides is drawn to identify the S2 vertebral arch, and then a needle is inserted through the S2/3 intervertebral space. However, complete fusion of the S2/3 space was found in 49 young patients (34.3%), the youngest among whom was 4 years old. Moreover, 21 patients (14.7%) among the 49 young patients showed no fusion of the S1/2 space. Therefore, when the method described above is used, the needle may be inserted to the S1/2 level, which is more risky. In addition, 91 patients (63.6%) out of the 94 patients (65.7%) who showed no fusion of the S2/3 intervertebral space still have the risk of inserting the needle to the more risky S1/2 level.
In this study, the sacral cornu could be identified on none of the two sides in 5 patients (3.5%), and on only one side in 6 patients (4.2%). This result is greatly different from the result of Sekiguchi et al. [6] (absent cornu 54% and unilateral cornu 25%) and the result of Aggarwal et al. [7] (no palpable cornu 14.3% and unilateral palpable cornu 24.5%). In a study conducted by Sekiguchi et al., the height of the bony protrusion was directly measured, and a protrusion longer than 3 mm was defined as a cornu. On the other hand, two authors identified the cornu by direct palpation in the study conducted by Aggarwal et al. In our study, the cornu could not be directly palpated because the cornu was indirectly identified with 3D images. In addition, it was difficult to set the standard for protrusion because the age of the patients varied. Therefore, we defined a cornu as the S5 articular process identified in the sagittal view of the 3D-CT images, which was the limitation of our study.
On the other hand, Griffiths et al. [11] conducted a study with 79 cerebral palsy patients from the age of 5 to 16 with radiography and reported that spina bifida occulta was found in 32% of the patients. Ozaras et al. [16] analyzed 28 spina bifida patients and stated that those patients had a high possibility of accompanying cerebral palsy. In this study, however, there was no significant difference in the distribution of the sacral hiatus types between the patients with and without cerebral palsy. Even when the patients with cerebral palsy were excluded to consider the previous results, the number of patients in Group II was 10 (12.2%) and 15 in Group III (18.3%), indicating that the anatomical variations that increase the risk of caudal epidural block still exist.
The weak point of this study is that the study was conducted in an indirect way with 3D-CT images, not in a direct way with cadavers. Therefore, as described above, the frequency of cornua anomaly was significantly lower than that of previous studies. In addition, the subjects of this study included not normal young children but the young patients with various congenital disorders at the hip and pelvis, and thus, the sacral canal development process of the subjects may be different from that of normal young children. The common congenital disorders were cerebral palsy, Legg-Calve-Pertes disease, developmental dislocation of hip, and arthrogryposis. Except for cerebral palsy, however, none of the congenital disorders have been reported to have an effect on the formation of the sacral canal.
This study was conducted to analyze the sacral hiatus of children with 3D-CT images. While the purpose of previous studies was to find an efficient method for approaching the sacral canal, our study was the first one in which the risk of caudal epidural block was assessed in children. In conclusion, degree of sacral fusion is less in children than in adults, and the exact location of the sacral hiatus is more difficult to be identified in children. Therefore, great efforts should be made to understand the process of sacral vertebra development and to investigate anatomical structures with imaging instruments such as ultrasonography to identify the anatomical structure precisely.
References
1. Najman IE, Frederico TN, Segurado AV, Kimachi PP. Caudal epidural anesthesia: an anesthetic technique exclusive for pediatric use? Is it possible to use it in adults? What is the role of the ultrasound in this context? Rev Bras Anestesiol. 2011; 61:95–109. PMID: 21334512.

2. Beyaz SG. Comparison of postoperative analgesic efficacy of caudal block versus dorsal penile nerve block with levobupivacaine for circumcision in children. Korean J Pain. 2011; 24:31–35. PMID: 21390176.

3. Brenner L, Kettner SC, Marhofer P, Latzke D, Willschke H, Kimberger O, et al. Caudal anaesthesia under sedation: a prospective analysis of 512 infants and children. Br J Anaesth. 2010; 104:751–755. PMID: 20385572.

4. Aggarwal A, Aggarwal A, Harjeet , Sahni D. Morphometry of sacral hiatus and its clinical relevance in caudal epidural block. Surg Radiol Anat. 2009; 31:793–800. PMID: 19578805.

5. Aggarwal A, Sahni D, Kaur H, Batra YK, Sondekoppam Vijayashankar R. The caudal space in fetuses: an anatomical study. J Anesth. 2012; 26:206–212. PMID: 22076688.

6. Sekiguchi M, Yabuki S, Satoh K, Kikuchi S. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004; 20:51–54. PMID: 14668657.

7. Aggarwal A, Kaur H, Batra YK, Aggarwal AK, Rajeev S, Sahni D. Anatomic consideration of caudal epidural space: a cadaver study. Clin Anat. 2009; 22:730–737. PMID: 19637298.

8. Broome DR, Hayman LA, Herrick RC, Braverman RM, Glass RB, Fahr LM. Postnatal maturation of the sacrum and coccyx: MR imaging, helical CT, and conventional radiography. AJR Am J Roentgenol. 1998; 170:1061–1066. PMID: 9530059.

9. Adewale L, Dearlove O, Wilson B, Hindle K, Robinson DN. The caudal canal in children: a study using magnetic resonance imaging. Paediatr Anaesth. 2000; 10:137–141. PMID: 10736075.

10. Busoni P, Sarti A. Sacral intervertebral epidural block. Anesthesiology. 1987; 67:993–995. PMID: 3688545.

11. Griffiths GJ, Evans KT, Roberts GM, Lloyd KN. The radiology of the hip joints and pelvis in cerebral palsy. Clin Radiol. 1977; 28:187–191. PMID: 870280.

12. Senoglu N, Senoglu M, Oksuz H, Gumusalan Y, Yuksel KZ, Zencirci B, et al. Landmarks of the sacral hiatus for caudal epidural block: an anatomical study. Br J Anaesth. 2005; 95:692–695. PMID: 16155035.

13. Shin SK, Hong JY, Kim WO, Koo BN, Kim JE, Kil HK. Ultrasound evaluation of the sacral area and comparison of sacral interspinous and hiatal approach for caudal block in children. Anesthesiology. 2009; 111:1135–1140. PMID: 19809281.

14. Nishiyama T, Hanaoka K, Ochiai Y. The median approach to transsacral epidural block. Anesth Analg. 2002; 95:1067–1070. PMID: 12351296.

15. Kumagai M, Yamashita M. Sacral intervertebral approach for epidural anaesthesia in infants and children: application of "drip and tube" method. Anaesth Intensive Care. 1995; 23:469–471. PMID: 7485939.

16. Ozaras N, Yalcin S, Ofluoglu D, Gureri B, Cabukoglu C, Erol B. Are some cases of spina bifida combined with cerebral palsy? A study of 28 cases. Eura Medicophys. 2005; 41:239–242. PMID: 16249782.
Fig. 1
Three-dimensional CT image; A: distance between sacral cornua, B: distance between S4 vertebral laminae; C: sacral intervertebral space, D & E: both sacral cornua.
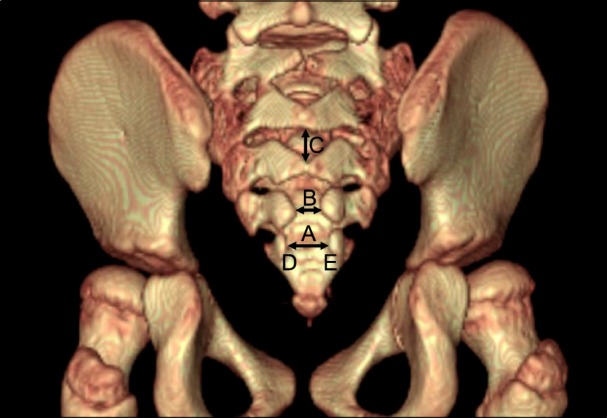
Fig. 2
Classification of the sacral hiatus by three-dimensional CT image; (A) Group I; fused S3; (B) Group II; not fused S3 and S4 laminae, distance of S3 vertebral laminae less than 50% of distance between sacral cornua; (C) Group III; not fused S3 or S4 laminae, distance of S3 and S4 vertebral laminae more than 50% of the distance between the sacral cornua. The 3 groups were classified by the fusion of the S3 or S4 vertebral laminae and the distance of the sacral vertebral laminae.
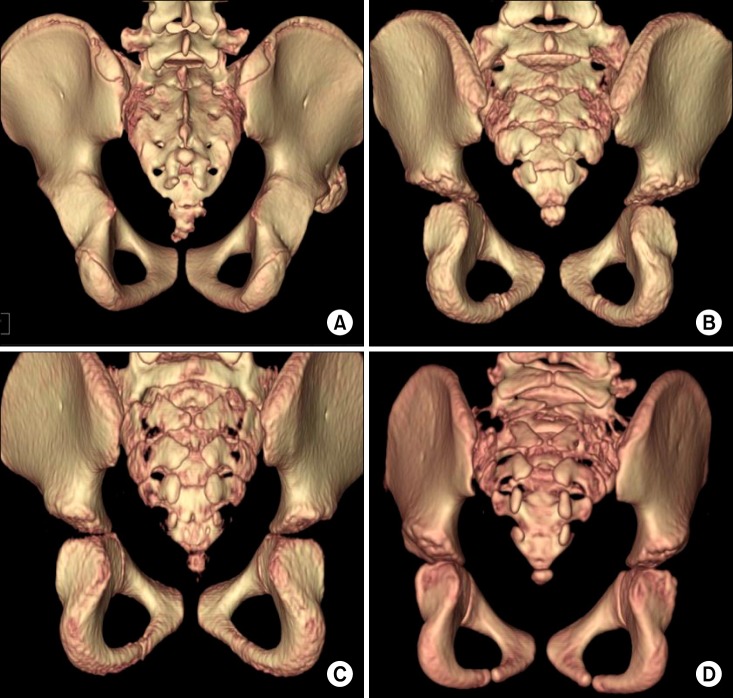
Fig. 3
Proportion of groups I, II and III distributed by age. The proportion of group I increase with age. (A) including all study patients (P = 0.040), (B) excluding cerebral palsy patients (P = 0.032).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download