Abstract
Purpose
The purpose of this study was to identify factors affecting health promotion behavior among workers with high risk of metabolic syndrome. This study was based on the planned behavior theory.
Methods
The participants were 167 workers at high risk of metabolic syndrome. Data were collected using a structured questionnaire. Surveyed variables were attitude, subjective norm, perceived behavioral control, intention, and health promotion behavior. Data were analyzed using descriptive statistics, t-test, ANOVA, Pearson's correlation coefficients, and hierarchical regression analysis with SPSS/WIN 22.0.
Results
Perceived behavioral control affected the intention of health promotion behavior among the workers with high risk of metabolic syndrome. It explained 62% of variance in the intention of health promotion behavior (F=40.09, p<.001). Perceived behavioral control and occupation affected health promotion behavior among the risk workers with high risk of metabolic syndrome. The two factors explained 16% of variance in health promotion behavior (F=4.95, p<.001).
Conclusion
The findings of this study suggest that perceived behavioral control is the only factor affecting health promotion behavior when the theory of planned behavior was applied. Therefore, intervention programs for improving health promotion behavior should be focused on strengthening perceived behavioral control.
Figures and Tables
Table 1
Sociodemographic Characteristics (N=167)

Table 2
Metabolic Syndrome Risk Factor Characteristics (N=167)

†Blood sugar: Normal group<100 mg/dL, High risk group≥100 mg/dL; ‡Systolic blood pressure: Normal group<130 mmHg, High risk group≥130 mmHg; §Diastolic blood pressure: Normal group<85 mmHg, High risk group≥85 mmHg; ∥Triglyceride level: Normal group<150 mg/dL, High risk group≥150 mg/dL; ¶High-density lipoprotein cholesterol: Male) Normal group>40 mg/dL, High risk group≤40 mg/dL, Female) Normal group>50mg/dL, High risk group≤50mg/dL; #Waist circumference: Male) Normal group<90 cm, High risk group≥90 cm, Female) Normal<85 cm, High risk group≥85 cm.
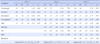
Table 3
Health Promotion Behavior Intention and Health Promotion Behavior in Accordance with Sociodemographic Characteristics (N=16)
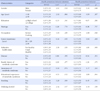
Table 4
Factors Affecting Health Promotion Behavior Intention (N=167)

Table 5
Factors Affecting Health Promotion Behavior (N=167)
References
1. Oh SW. Shows the prevalence of metabolic syndrome in adults over 30 years old 28.8%! [Internet]. Seoul: Ministry of Health and Welfare, Division of Health Policy;2012. cited 2014 Mar 10. Available from: http://www.mw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=268137&page=1.
2. Ryu S, Song J, Choi BY, Lee SJ, Kim WS, Chang YS, et al. Incidence and risk factors for metabolic syndrome in Korean male workers, age 30 to 39. Ann Epidemiol. 2007; 17(4):245–252. DOI: 10.1016/j.annepidem.2006.10.001.
3. Kim CJ, Park JB, Kim BT. Lifestyle characteristics, metabolic syndrome risk factors and risk of cardiovascular disease among workers in Kyeongki-do. Korean J Occup Health Nurs. 2008; 17(2):230–238.
4. Park SY, Yang YJ, Kim YR. Effects of nutrition education using a ubiquitous healthcare (u-health) service on metabolic syndrome in male workers. Korean J Nutr. 2011; 44(3):231–242. DOI: 10.4163/kjn.2011.44.3.231.

5. Maruyama C, Kimura M, Okumura H, Hayashi K, Arao T. Effect of a worksite-based intervention program on metabolic parameters in middle-aged male white-collar workers: A randomized controlled trial. Prev Med. 2010; 51(1):11–17. DOI: 10.1016/j.ypmed.2010.04.008.

6. Wannamethee SG, Shaper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: Effects of lifestyle changes. J Am Geriatr Soc. 2006; 54(12):1909–1914. DOI: 10.1111/j.1532-5415.2006.00974.x.

7. Kim YH, Park RJ, Park WJ, Kim MB, Moon JD. Predictors of metabolic syndrome among shipyard workers and its prevalence. Korean J Occup Environ Med. 2009; 21(3):209–217.

8. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005; 112(17):2735–2752.
9. Tsai TY, Cheng JF, Lai YM. Prevalence of metabolic syndrome and related factors in Taiwanese high-tech industry workers. Clinics (Sao Paulo). 2011; 66(9):1531–1535.

10. Kang JY, Cho SW, Lee JY, Sung SH, Park YK, Paek YM, et al. The effects of a worksite on-line health education program on metabolic syndrome risk factors and nurtient intakes of male workers. Korean J Nutr. 2010; 43(1):57–68. DOI: 10.4163/kjn.2010.43.1.57.
11. Bae SS. Approaches and theories of health promotion. Seoul: Gyechuk Munwhasa;2012. p. 524.
12. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991; 50(2):179–211. DOI: 10.1016/0749-5978(91)90020-T.

13. Bae SS, Lee HJ, Lee CO, Jo HS. Predicting exercise behavior in female workers: An application of the theory of planned behavior. Korean J Health Educ Promot. 2003; 20(1):173–186.
14. Lee HJ, Jo BH. Factors affection intentions for health behaviors among male office workers: An analysis based on the theory of planned behavior. Korean J Occup Health Nurs. 2002; 11(1):31–43.
15. Payne N, Jones F, Harris PR. The role of perceived need within the theory of planned behavior: A comparison of exercise and healthy eating. Br J Health Psychol. 2004; 9(Pt 4):489–504.
16. Korean Academy of Medical Science. Metabolic syndrome: An overview [Internet]. Seoul: Korean Academy of Medical Science;2010. cited 2014 January 26. Available from: http://www.kams.or.kr/health/sub3.html.
17. Kang SW. Development of a lifestyle evaluation tool for patients with metabolic syndrome [dissertation]. [Seoul]: Yonsei University;2007. 120.
18. Plotnikoff RC, Lubans DR, Costigan SA, McCargar L. A test of the theory of planned behavior to predict physical activity in an overweight/obese population sample of adolescents from Alberta, Canada. Health Educ Behav. 2013; 40(4):415–425. DOI: 10.1177/1090198112455642.

19. Park BH, Lee MS, Hong JY, Bae SH, Kim EY, Kim KK, et al. The stages of physical activity and exercise behavior: An integrated approach to the theory of planned behavior. Asia Pac J Public Health. 2009; 21(1):71–83. DOI: 10.1177/1010539508327089.

20. Andrykowski MA, Beacham AO, Schmidt JE, Harper FW. Application of the theory of planned behavior to understand intentions to engage in physical and psychosocial health behaviors after cancer diagnosis. Psychooncology. 2006; 15(9):759–771.

21. Yeongdeungpo-gu Health Center. Metabolic syndrome free screening program [Internet]. Seoul: Yeongdeungpo-gu Health Center;2011. cited 2014 January 15. Available from: http://www.ydp.go.kr/health/page.do?mCode=E120020000.
22. National Health Insurance Service. Health screenings statistical yearbook in 2012. Seoul: National Health Insurance Service;2013. 12. Report No.: 11-B550928-000048-10.
23. Choi ES. The metabolic syndrome and associated risk factors among male workers in an electronics manufacturing company. Korean J Occup Environ Med. 2006; 18(1):35–45.

24. Gardner RE, Hausenblas HA. Exercise and diet determinants of overweight women participating in an exercise and diet program: A peospective examination of the theory of planned behavior. Women Health. 2005; 42(4):37–62.
25. Hunt HR, Gross AM. Prediction of exercise in patients across various stages of bariatric surgery: A comparison of the merits of the theory of reasoned action versus the theory of planned behavior. Behav Modif. 2009; 33(6):795–817. DOI: 10.1177/0145445509348055.

26. Conner M, Sandberg T, Norman P. Using action planning to promote exercise behavior. Ann Behav Med. 2010; 40(1):65–76. DOI: 10.1007/s12160-010-9190-8.

27. Murnaghan DA, Blachard CM, Rodgers WM, LaRosa JN, Mac-Quarrie CR, MacLellan DL, et al. Predictors of physical activity, healthy eating and being smoke-free in teens: A theory of planned behavior approach. Psychol Health. 2010; 25(8):925–941. DOI: 10.1080/08870440902866894.
28. de Bruijn GJ, Rhodes RE. Exploring exercise behavior, intention and habit strength relationships. Scand J Med Sci Sports. 2011; 21(3):482–491. DOI: 10.1111/j.1600-0838.2009.01064.x.

29. Chung HJ, Rho SJ, Lee KH. The effects of cooking operations duties and kitchen facilities on fatigue. J East Asian Soc Diet Life. 2008; 18(3):405–414.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download