Abstract
Purpose
Although upper airway cough syndrome (UACS) is one of the most common causes of chronic cough, there are few reports on the effects of intranasal steroids (INS) on improvement of cough in patients with chronic cough caused by UACS. Here, we observed improvement in cough depending on prescribed medications, including INS, in patients with chronic cough caused exclusively by UACS in the clinical setting.
Methods
Patients with chronic cough caused exclusively by UACS were selected by the retrospective review of medical records. Durations and kinds of prescribed medications, nasal and postnasal drip symptoms, and results of paranasal sinus series at first visit were evaluated. According to the improvement of cough at the second visit, the patients were divided into the improved and unimproved groups. Odds ratios of each medication in the improved group were analyzed by logistic regression adjusted for age, sex, smoking history, duration of treatment, prescriptions of medications, presence of nasal and postnasal drip symptoms, and results of paranasal sinus series.
Results
A total of 122 patients with chronic cough caused exclusively by UACS were comprised of 38 patients in the improved group and 84 patients in the unimproved group. INS were prescribed to 45 patients, and the number of patients with INS prescription were significantly higher in the unimproved group than that in not-improved group (55.3% vs. 28.6%, P=0.008). The odds ratio of INS prescription was significantly higher in the improved group (odds ratio, 4.78; 95% confidence interval, 1.03-22.3; P=0.046).
Figures and Tables
Fig. 1
Improvement of cough in patients with and without prescription of intranasal steroids (INS). Cough improved significantly in the patients with prescription of INS than in the patients without INS prescription. P-value was obtained through Mann-Whitney U-test.
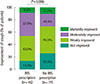
Table 1
Demographic and clinical characteristics of subjects by groups according to improvement of cough

Table 3
Odds ratios for improved group by the kinds of medications (n=122)
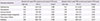
PND, postnasal drip; PNS, paranasal sinus; CI, confidence interval.
*P-values were obtained through logistic regression analysis adjusted for age, sex, smoking history, duration of treatment, and prescriptions of medications which are entered as one block. †P-values were obtained through logistic regression analysis adjusted for age, sex, smoking history, duration of treatment, prescriptions of medications, presence of nasal and PND symptoms, and results of PNS series which are entered as one block.
References
1. Pratter MR. Chronic upper airway cough syndrome secondary to rhinosinus diseases (previously referred to as postnasal drip syndrome): ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 63S–71S.
2. Pratter MR, Bartter T, Akers S, DuBois J. An algorithmic approach to chronic cough. Ann Intern Med. 1993; 119:977–983.

3. Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 1S–23S.
4. Pratter MR, Brightling CE, Boulet LP, Irwin RS. An empiric integrative approach to the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 222S–231S.
5. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.

6. Gawchik S, Goldstein S, Prenner B, John A. Relief of cough and nasal symptoms associated with allergic rhinitis by mometasone furoate nasal spray. Ann Allergy Asthma Immunol. 2003; 90:416–421.

7. Macedo P, Saleh H, Torrego A, Arbery J, MacKay I, Durham SR, et al. Postnasal drip and chronic cough: an open interventional study. Respir Med. 2009; 103:1700–1705.

8. Global Initiative for Asthma. Global strategy for asthma management and prevention 2014 [Internet]. Global Initiative for Asthma;cited 2014 Jun 14. Available from: http://www.ginasthma.org/GINA-Report,-Global-Strategy-for-Asthma-Management-and-Prevention.
9. Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 80S–94S.
10. Brightling CE. Chronic cough due to nonasthmatic eosinophilic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 116S–121S.
11. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of COPD 2014 [Internet]. Global Initiative for Chronic Obstructive Lung Disease;cited 2014 Jun 14. Available from: http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html.
12. Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:1 Suppl. 59S–62S.
13. Plevkova J, Song WJ. Chronic cough in subjects with upper airway diseases - analysis of mechanisms and clinical applications. Asia Pac Allergy. 2013; 3:127–135.

14. Birring SS. Controversies in the evaluation and management of chronic cough. Am J Respir Crit Care Med. 2011; 183:708–715.

15. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
16. Loh CY, Chao SS, Chan YH, Wang DY. A clinical survey on compliance in the treatment of rhinitis using nasal steroids. Allergy. 2004; 59:1168–1172.

17. Raj AA, Birring SS. Clinical assessment of chronic cough severity. Pulm Pharmacol Ther. 2007; 20:334–337.

18. French CT, Irwin RS, Fletcher KE, Adams TM. Evaluation of a cough-specific quality-of-life questionnaire. Chest. 2002; 121:1123–1131.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download