Abstract
The aim of this study was to assess the potential of a prone chest CT for the evaluation of esophageal cancer, as compared with a routine supine chest CT. 69 patients (67±18 years old) with pathologically confirmed esophageal cancers underwent MDCT in the supine and prone positions. The supine CT was performed first, followed by the prone position. Localization and staging of individual esophageal lesions on both the prone and supine CTs were assessed by two thoracic radiologists, using a scoring system that consisted of three confidence scales, and the results were correlated with the endoscopic and surgical findings. The mean confidence score for the detection of esophageal cancer was higher in the prone position (2.58±0.74) than that in the supine position (2.42±0.83) with statistical significance (p=0.002). The mean confidence score for predicting local invasion in the selected patients (n=18) who underwent esophagectomy was also higher in the prone position (2.39±0.85) than that in the supine position (2.06±0.73) with statistical significance (p=0.01). In 10 of 11 cases that showed definitive determination for periesophageal infiltration or adjacent organ invasion on the prone CT (score 3), the corresponding findings were also observed in the post-operative evaluations. In conclusion, prone chest CT for evaluating esophageal cancer could have advantages in regards to the localization of esophageal cancer and predicting local invasion compared to that of routine supine CT and can improve the diagnostic accuracy of chest CTs.
Computed tomography (CT) is widely used for preoperative staging and obtaining information on the tumor size, location, extension, and respectability in a hollow viscus.1 Due to advanced multi-detector CT (MDCT) technology, a proper contrast material injection technique offers improved differentiation of tumor tissue from the normal mucosa in patients with esophageal cancer.2 The advance of MDCT with the three-dimensional CT protocols, including CT esophagography, may provide better preoperative staging, treatment planning, and restaging after treatment of esophageal cancer.134 However, the esophagus is a long hollow muscular tube that is poorly distensible and is surrounded by many vital organs.3 In addition, the esophagus also lacks a serosal layer, which makes it difficult to detect subtle changes in the spreading of diseases and allows malignant esophageal lesions to spread via the lymphatics to regional lymph nodes and directly into the adjacent structures.5 For these reasons, detection of esophageal cancer and the evaluation of invasion into the adjacent structures by esophageal lesion on MDCT are still challenging. Of course, endoscopic ultrasound is another modality that is highly sensitive in detecting the depth of tumor invasion and may be more sensitive in differentiating T1 from T2 disease.6 Nevertheless, CT still plays an important role in diagnosing and staging esophageal cancer, especially in cases of T3 and T4.
The esophagus is usually not fixed in the mediastinum of patients with esophageal cancer and will consequently move anteriorly, from 1.5 to 2 cm, when patient swallow barium while lying in the prone position.7 Therefore, it may be possible to increase the space between the esophagus and the vertebral bodies and aorta if this position is used.
Several previous studies have reported on CT techniques when the patient is in the prone position. van den Hoed et al.8 reported that additional patient positions do not improve the CT prediction of aortic invasion of esophageal cancer. However, Wayman et al.9 reported that modification of the CT protocol to include scanning in the prone position can improve the accuracy in the staging of esophageal cancer. There have been only few studies that evaluated the effectiveness of prone CT for the evaluation of esophageal cancer. However, these studies were restricted to areas of local invasion and the results are still controversial. Thus, the aim of this study was to assess the utility of MDCT with the patient in the prone position for evaluation of localization as well as the staging of esophageal cancer, including local invasion.
This study was approved by the Institutional Review Board of Chonnam National University Hospital, Gwangju, Korea (IRB : I-2007-05-044). For eight months, 69 consecutive patients with pathologically confirmed esophageal cancer and who underwent CT scanning for the localization and staging of tumors were enrolled. Before CT scanning, informed consent, which included information on the goals of our study and the increased risk due to the radiation dose in two positions (prone and supine), was obtained from all 69 patients.
The patients included 63 men and 6 women, whose age ranged from 45 to 85 years (mean age of 67 years). The locations of the cancers were 39 (56%) in the mid esophagus, 24 (35%) in the lower esophagus, and 6 (9%) in the upper esophagus on the endoscopic exam. Histopathologic types of the cancers confirmed by endoscopic biopsies included 65 cases (94%) of squamous cell carcinoma which arose from the mid esophagus in 38 (59%), the lower esophagus in 21 (32%) and the upper esophagus in 6 (9%), and 4 cases (6%) of adenocarcinoma which arose from the lower esophagus in 3 (75%) and the mid esophagus in 1 (25%). The treatments for the carcinomas included surgical resection for 18 (26%), combined chemotherapy and radiation therapy for 33 (48%), chemotherapy for 2 (3%), radiation therapy for 1 (1%), and loss of follow up for 15 (22%).
CT scanning was performed using multi-detector row CT scanners (Light Speed 16 or Light Speed VCT, GE Medical systems, WI, USA ; Sensation Cardiac 64, Seimens Medical Solution, Forchheim, Germany) in all patients. Chest CT scans were obtained after intravenous injection of 120-130 mL of nonionic contrast medium (Iohexol, Omnipaque®, Amersham health, Cork, Ireland; Iopromid, Ultravist 300®,, Bayer Schering Pharma, Berlin, Germany) at a rate of 2 mL/sec. The scanning parameters are summarized in Table 1, according to the different scanners. All patients ingested 300–600 mL of tap water and 4 g of effervescent granulate (Top effervescent-G granules, Taejoon Pharm, Seoul, Korea) before CT scanning to allow for adequate dilatation of the esophageal lumen. All CT scans were performed with the patient first in the supine position. The patient was then scanned in the prone position.
Two sets of MDCT images (supine and prone) for the localization of esophageal cancer, the determination of the presence or absence of periesophageal infiltration or adjacent organ invasion and the presence of periesophageal lymphadenopathy (LAP) were reviewed by two thoracic radiologists with 11 and 6 years of experience, respectively, and this was done independently of the interpretation of the CT images. The reviewers were blinded to the endoscopic and surgical findings. All CT images were reviewed on a picture archive and communication system workstations (PACS; Marotech 5.4, Seoul, Korea). The cases were randomly presented in each reading session. The reviewers were allowed to adjust the window width and level on the PACS monitor. Discrepancies in the assessment were resolved by consensus. The supine and prone CTs were anonymized and reviewed independently on separated occasions. The CT assessment was finally compared with the endoscopic findings in all cases and post-operative findings in the surgical cases.
The applied criteria for the diagnosis of esophageal cancer were abnormal enhancement or an irregular mucosal surface or thickening of the esophageal wall (>3 mm).1 CT examinations of the relative detectability of esophageal cancer were graded using a three-point confidence scale: 1, no detectable lesion or no corresponding site with the endoscopic finding on the chest CT; 2, suspicious lesion on the chest CT, with a corresponding site in the endoscopic finding; 3, a definite esophageal mass lesion on the chest CT.
The location of detectable esophageal cancer on the CT was also described according to the Union Internationale Contre Le Cancer classification such as the upper, mid and lower esophagus and this location was retrospectively compared with the results of the endoscopic findings.
Evaluation of periesophageal infiltration or adjacent organ invasion was performed for patients who had a suspicious esophageal lesion or definite esophageal cancer. The applied criteria for periesophageal infiltration or adjacent organ invasion were strands in the periesophageal fat plane or a mass effect, and loss of fat planes with the adjacent mediastinal organs.1 A three-point confidence scale was used to determine whether there was infiltration or organ invasion on the supine CT and prone CT: 1, impossible to determine infiltration or invasion: 2. Suspicion of infiltration or invasion: 3, definitely possible infiltration or invasion.
The applied criteria for periesophageal significant LAP were an enlarged lymph node (shortest diameter: >6 mm) or a morphologically round node (longitudinal-transverse diameter ratio <1.5) or an abnormal enhancing pattern.1 Significant LAP on the CT examinations was graded using a three-point confidence scale for individual LNs: 1, no lymph node metastasis: 2, suspicion of lymph node metastasis: and 3, definite lymph node metastasis. The presence or absence of periesophageal infiltration or adjacent organ invasion and the presence of periesophageal LAP was pathologically correlated with post-surgical findings in surgical cases (26%, n=18/69).
A paired t-test was performed using the Statistical Package for Social Sciences for statistical analysis using Windows (version 13.0, Chicago, Illinois, USA).
The data was expressed as mean±standard deviations for continuous variables and percentages for categorical data.
Assessment of the localization of esophageal cancer, determination of the presence or absence of periesophageal infiltration or adjacent organ invasion and the presence of periesophageal LAP was first performed for the supine and prone CT, and the differences between the supine and prone CTs were then evaluated. A p-value of less than 0.05 was considered to be a statistically significant difference.
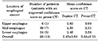
For the localization of esophageal cancer, the prone CT (2.58±0.74) had a higher mean confidence score than the supine CT (2.42±0.83) (p=0.002) (Table 2). Diagnostic improvement for the localization of esophageal cancer for the prone CT was observed at all three locations when compared with that of the supine CT (Table 2). In the advanced esophageal malignancy (T3 and T4, 32/69 cases), there was no significant difference in the localization of esophageal cancer between the supine and prone positions. The lesions in 21 cases (30.4%) were determined to be superficial esophageal cancer in the endoscopic findings such as localized surface lesions, slightly elevated lesions or depressed lesions. In 11 of the 21 cases (52.4%) of superficial lesion, focal or diffuse wall thickening on prone CT was well visualized when compared with that on the supine CT by the virtue of dilatation of the esophageal lumen (Fig. 1). In 3 of the 21 cases (14.3%), an esophageal lesion was identified only on the prone CT, but not on the supine CT. In 7 of the 21 cases (33.3%), an esophageal lesion was not observed by either CT exam.
In 13 (18.8%) of the 69 cases, the localization of esophageal malignancies were different between on the supine and on the prone CT. Among these 13 cases, 12 esophageal lesions were better identified on the prone CT than the supine CT (1 in the upper esophagus, 7 in the mid esophagus, 4 in the lower esophagus). The one upper esophageal lesion was detected as concentric and irregular wall thickenings, which was much more clearly identified on the prone CT than the supine CT. In 4 of the 7 mid-esophageal lesions (57.1%), focal wall thickenings were observed on the prone CT as a score 2, but the lesions were not detected on the supine CT (score 1) (Fig. 1). These 4 lesions were confirmed by esophageal endoscopy, and two among these 4 lesions were confirmed as T1 cancer by post-operative pathologic exams. The remaining 3 cases of mid-esophageal lesions were categorized as score 3 on the prone CT, but as score 2 on the supine CT. Three of the 4 lower esophageal lesions (75%) showed a score 3 on the prone CT, but a score 2 on the supine CT. The remaining lesion (25%) showed score 2 on the prone CT as eccentric wall thickening with focal enhancing area, which was not detected in the supine CT (score 1). In one case of a protruding lesion in the lower esophagus, the esophageal lesion was better identified on the supine CT than the prone CT, because of the relatively increased dilatation of the esophageal lumen on the supine CT than the prone CT.
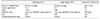
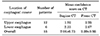
Periesophageal infiltrations (local invasion) of esophageal carcinomas were suspected in 54 cases on the chest CT. In these 54 cases, prone CT had a higher mean confidence score than supine CT (2.91 vs 2.65) in all three esophageal locations (upper, mid, and lower esophagus) with a statistically significant difference (p=0.01) (Table 3).
In regards to local invasion, different scores were observed in 15 of the 54 cases (27.8%) between the supine and the prone CT. Among these 15 cases, 14 cases (93.3%) were well visualized on the prone CT and one case (6.7%) was clearly observed on the supine CT. Of these 14 lesions that were more clearly visualized on the prone CT, 8 were in the mid-esophagus, 5 in the lower esophagus, and 1 in the upper esophagus. Eleven from these 14 cases (78.6%) were demonstrated to be superficial esophageal carcinomas by esophageal endoscopy.
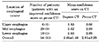
Surgical esophagectomy was performed in 18 of 69 patients, of which 12 (66.7%) were in the mid-esophagus and 6 (33.3%) were in the lower esophagus, and of which postoperative T stages were T1 in 13 cases (72.2%), T2 in 3 cases (16.7%), and T3 in 2 cases (11.1%). In the comparison of preoperative predictability for periesophageal infiltration on CT for these 18 cases, Prone CT had a higher mean confidence score (2.39) than supine CT (2.06), and showed a statistically significant difference (p=0.01) (Table 4). In 6 of the 18 cases (33.3%), the image qualities for determining periesophageal infiltrations were higher on the prone CT than supine CT, which corresponded with the surgical findings (Fig. 2). 11 cases showed definitive determination for absence or presence (score 3) for periesophageal infiltration on the prone CT. Among these 11 cases, 10 cases were confirmed by the post-operative findings, except for one case of underestimation by the prone CT.
To assess periesophageal metastatic LAP, 2 of 54 cases, which showed visible lymph nodes on the chest CT, had a higher confidence score on the prone CT (mean confidence score: 2.33) than the supine CT (mean confidence score: 2.27) which did not represent a statistically significant difference (p=0.08). In one case, a suspicious lymph node abutting the esophageal lesion around the left gastric artery on the supine CT was determined to be definite metastatic LAP based on the prone CT by the virtue of the broader interspace between the liver and esophagus. In the other case, a LAP in the post-esophageal space around the lower esophagus was not identified on the supine CT, but prone CT showed definite metastatic LAP containing a peripheral rim-enhancement and central low attenuated area, by virtue of the broaden interspace between the vertebra and esophagus (Fig. 3).
Many investigators have recommended a routine CT examination before treatment planning.1011121314 Nevertheless, there has been debate on the sensitivity and specificity of CT for detecting mediastinal invasion by esophageal cancer, although the overall sensitivity (from 75% to 100%) and specificity (from 78% to 95%) of CT for detecting mediastinal invasion is relatively high.101314 Maerz et al.15 concluded that CT scans are useful for identifying advanced diseases and predicting respectability, but it is not sensitive enough for evaluating less advanced diseases. Although CT has been used for preoperative evaluation of esophageal cancer, the major role of CT has been the depiction of lymph nodes, distant metastases, or both rather than the evaluation of the local status of esophageal cancer.2 However, Umeoka et al.2 introduced triple-phase dynamic CT for the evaluation of esophageal cancer and suggested that the second arterial phase of dynamic CT was the optimal phase for visualizing esophageal cancer. Some authors134 have insisted that MDCT can be utilized for such applications by using multiplanar reformation or 3D reconstruction, including CT esophagogrphy, for the diagnosis and staging of esophageal cancer. However, good organ distension and postprocessing techniques are needed to obtain good results with MDCTs.1 It is still difficult to evaluate esophageal cancer with MDCT despite the use of water and effervescent granulate as a negative contrast agent because of its poor distensibility and relatively long length. The use of an effervescent agent requires considerable patient cooperation and proper timing for scanning in order to achieve optimal distension of the esophagus.6 In addition, the sensitivity of CT for detecting metastases to the lymph nodes is also low.1116
Ball et al.17 reported remarkable changes in the position of organs on computed tomography when the patient was scanned in the prone position. Gravitational movement of the heart increases the space between the left atrium and the vertebral bodies, and the esophagus moves more ventrally to the aorta. Within the abdomen, prone positioning produces a ventral as well as caudal shift of the liver, spleen and kidneys. Based on these findings, previous studies have evaluated the effect of adjusting the patient's position with the goal of achieving proper distention and fluid distribution in the hollow viscus during CT examination to help diagnose and stage malignances of a movable and distensible hollow viscus such as the esophagus and the gastrointestinal tract. For example, CT scanning in the supine, prone, and left posterior oblique position was performed with drug induced hypotonia and water filling to improve the detection of gastric antric lesions.18 For colonic malignancy, CT colonography was scanned with the patient in both the supine and prone positions to improve the detection ratio.19
In our study, prone CT did not improve the detectability of upper esophageal lesions, but 19% (12/63) the mid or lower esophageal malignancies were better identified by prone CT when compared to that of supine CT. The detectability of advanced esophageal cancer didn't show a statistically significant difference between the supine and prone positions. However, the detectability of protruding lesions or eccentric wall thickening of superficial esophageal malignancy (52%, n=11/21) was improved on the prone CT by virtue of the relatively broader interspace between the heart and esophagus and the dilatation of the esophageal lumen when compared with the routine supine position. Generally, no detectable lesions (score 1) on the supine CT were up-scored as suspicious lesions (score 2) on the prone CT, and the suspicious lesions (score 2) on the supine CT were up-scored as definite esophageal lesion (score 3) in prone CT. However, there were no cases where there was no detectable lesion (score 1) on the supine CT and a definite esophageal lesion (score 3) on the prone CT.
To assess local invasion, 26% of the cases (n=14/54) had a higher confidence score on the prone CT than on the supine CT with a statistically significant difference (p=0.01). The same results were observed in selected patients who underwent esophagectomy with a statistically significant difference (p=0.01). The patient group with esophagectomy had a relatively low grade stage and a statistically higher confidence score for preoperative prone CT than supine CT, which means that the preoperative predictability of local invasion was statistically higher for prone CT than supine CT, especially for the early stages of esophageal cancer. As discussed by Wayman et al.,9 a false positive suggestion of tumor invasion to adjacent structures could potentially deprive a patient of curative surgery and it would be highly beneficial if the prone scans could decrease the number of false positives. This result would reinforce their insistence that if an esophageal cancer can be shown to be inoperable because of infiltration or adhesion to the mediastinal structure, and particularly, the aorta in the routine supine position, then an additional prone CT may help increase the confidence of excluding or diagnosing invasion by moving the tumor relative to the aorta in the prone position.9 There was no statistical significance according to the distribution of esophageal malignancy between the prone and supine CTs because of the small number of upper esophageal lesions. In addition, there was no statistically significant difference in regards to assessing periesophageal metastatic LAP. It is well known that enlarged periesohageal lymph nodes near the tumor are difficult to distinguish from contiguous tumor spread.11 But in two cases of our study, the detectability of periesophageal LAPs was higher on the prone CT when compared with supine CT by virtue of the broader interspace between the esophagus and adjacent organs such as liver or vertebra. So, in certain situations, the prone CT may also be useful for evaluating periesophageal metastatic LAP.
This study had several limitations. First, the number of patients with esophagectomy was relatively small and some patients were dropped during follow up. So, some suspicious lesions (local invasion or LAP) were not confirmed surgically. Further prospective studies using a larger number of patients are needed to validate our results. The second limitation is the different scanning time after contrast enhancement between the supine and prone CT. The esophageal lesion on the supine CT was scanned on the arterial phase, in contrast to being scanned on the delayed enhancement phase as was done for the prone CT. Third, the amount of ingested water was different for each patient, which was adjusted according to the body condition of the patient, and the time interval between the ingestion of water and the CT scan was also different for each patient. So, some patients showed effective esophageal dilatation by virtue of the ingested water whereas other patients did not show effective dilatation.
In conclusion, prone CT for esophageal cancer would have the advantages of preoperatively detecting cancer and predicting local invasion, and this would improve the diagnostic ability of chest CTs for patients with esophageal cancer.
Figures and Tables
FIG. 1
A 75-year-old man with squamous cell carcinoma in the distal esophagus. (A) The axial contrast-enhanced CT scan with the patient in the supine position shows a collapsed esophageal lumen without any detectable mass-like lesion. (B) The axial contrast-enhanced CT scan with the patient in the prone position demonstrates eccentric nodular wall thickening (arrow) by virtue of the broaden interspace between the heart and vertebra and the distended esophagus.

FIG. 2
A 61-year-old man with squamous cell carcinoma in the mid esophagus. (A and B) The axial contrast enhanced CT scans (A and B) show a protruding mass (black arrows in A and B) in the esophagus. The axial CT scan with the patient in the supine position (A) demonstrates the esophagus, which abuts against the thoracic aorta (arrowheads), with suspicious invasion. However, the axial CT scan with the patient in the prone position (B) clearly demonstrates a fat plane (arrowheads) between the esophageal tumor and thoracic aorta, without evidence of invasion. Esophagectomy was performed in this patient and the postoperative TNM stage was determined to be T2 N0 M0.

FIG. 3
A 72-year-old man with mid esophageal cancer. (A) The axial contrast-enhanced CT scan with the patient in the supine position shows a hypo-attenuation lesion (white arrow) in the distal esophagus. (B) The axial contrast-enhanced CT scan with the patient in the prone position clearly shows the presence of hypo-attenuation lesion (white arrow in A) that is a necrotizing metastatic lymph node (arrowheads) rather than an esophageal lesion by virtue of the broaden interspace between the esophagus and the vertebral body.

TABLE 2
Comparison of localization of esophageal cancer between the supine chest CT and the prone chest CT (n=69)
References
1. Panebianco V, Grazhdani H, Iafrate F, Petroni M, Anzidei M, Laghi A, et al. 3D CT protocol in the assessment of the esophageal neoplastic lesions: can it improve TNM staging? Eur Radiol. 2006; 16:414–421.


2. Umeoka S, Koyama T, Togashi K, Saga T, Watanabe G, Shimada Y, et al. Esophageal cancer: evaluation with triple-phase dynamic CT--initial experience. Radiology. 2006; 239:777–783.


3. Ba-Ssalamah A, Zacherl J, Noebauer-Huhmann IM, Uffmann M, Matzek WK, Pinker K, et al. Dedicated multi-detector CT of the esophagus: spectrum of diseases. Abdom Imaging. 2009; 34:3–18.


4. Kim SH, Lee JM, Han JK, Kim YH, Lee JY, Lee HJ, et al. Three-dimensional MDCT imaging and CT esophagography for evaluation of esophageal tumors: preliminary study. Eur Radiol. 2006; 16:2418–2426.


5. Agrawal B. CT findings in patients with esophageal carcinoma and its correlation with esophagographic findings. Open J Radiol. 2018; 8:109–124.

6. Faigel DO. The role of endoscopic ultrasound in esophageal cancer. Gastroenterol Hepatol (N Y). 2019; 15:519–521.


7. Luo LN, He LJ, Gao XY, Huang XX, Shan HB, Luo GY, et al. Evaluation of preoperative staging for esophageal squamous cell carcinoma. World J Gastroenterol. 2016; 22:6683–6689.



8. van den Hoed RD, Feldberg MA, van Leeuwen MS, van Dalen T, Obertop H, Kooyman CD, et al. CT prediction of irresectability in esophageal carcinoma: value of additional patient positions and relation to patient outcome. Abdom Imaging. 1997; 22:132–137.


9. Wayman J, Chakraverty S, Griffin SM, Doyle GJ, Keir MJ, Simpson W. Evaluation of local invasion by oesophageal carcinoma--a prospective study of prone computed tomography scanning. Postgrad Med J. 2001; 77:181–184.



11. Yamabe Y, Kuroki Y, Ishikawa T, Miyakawa K, Kuroki S, Sekiguchi R. Tumor staging of advanced esophageal cancer: combination of double-contrast esophagography and contrast-enhanced CT. AJR Am J Roentgenol. 2008; 191:753–757.


12. Zhou SL, Zhou XY, Liu XJ, Bo GJ, Gu Y, Chen W. Comparison of dual source computed tomography (CT) and diffusion-weighted magnetic resonance imaging (MRI) for pathological classification of esophageal cancer. Int J Clin Exp Med. 2018; 11:12578–12584.
13. Pongpornsup S, Posri S, Totanarungroj K. Diagnostic accuracy of multidetector computed tomography (MDCT) in evaluation for mediastinal invasion of esophageal cancer. J Med Assoc Thai. 2012; 95:704–711.

14. Legmann P, Marmuse JP, Rjob S, Benacerraf R. Preoperative computed tomography for transhiatal esophagectomy. Invest Radiol. 1991; 26:987–991.


15. Maerz LL, Deveney CW, Lopez RR, McConnell DB. Role of computed tomographic scans in the staging of esophageal and proximal gastric malignancies. Am J Surg. 1993; 165:558–560.

16. Yoon YC, Lee KS, Shim YM, Kim BT, Kim K, Kim TS. Metastasis to regional lymph nodes in patients with esophageal squamous cell carcinoma: CT versus FDG PET for presurgical detection prospective study. Radiology. 2003; 227:764–770.


17. Ball WS, Wicks JD, Mettler FA Jr. Prone-supine change in organ position: CT demonstration. AJR Am J Roentgenol. 1980; 135:815–820.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download