Abstract
Particulate matter (PM) is suspended dust that has a diameter of <10 µm and can be inhaled by humans and deposited in the lungs, particularly the alveoli. Recent studies have shown that PM has an adverse effect on respiratory diseases. The aim of this article is to review respiratory diseases associated with PM. According to existing studies, PM is associated with chronic obstructive pulmonary disease, bronchial asthma, and several other respiratory diseases and increases the mortality rates of these diseases. Moreover, increased exposure in the high concentration of atmospheric PM is associated with the development of lung cancer. The most simple and common way to protect an individual from airborne PM is to wear a face mask that filters out PM. In areas of high concentration PM, it is recommended to wear a face mask to minimize the exposure to PM. However, the use of N95 or KF94 masks can interfere with respiration in patients with chronic respiratory diseases who exhibit low pulmonary function, leading to an increased risk of respiratory failure. Conclusionally, reduction of the total amount of PM is considered to be important factor and strengthening the national warning notification system to vulnerable patients and proper early management of exacerbated patients will be needed in the future.
Particulate matter (PM) is suspended dust that has a diameter of <10 µm (PM10) and can be inhaled by humans and deposited in the lungs, particularly the alveoli. In addition to PM10, PM with diameter <2.5 µm (PM2.5) and <0.1 (PM0.1) is classified as fine and ultrafine PM, respectively12. A major source of PM is the combustion of fossil fuels from human activity; however, natural sources, such as yellow dust, are also significant. Domestic PM consists of fine dust from China, seasonal yellow dust, and domestic-generated air pollutants34. As PM poses considerable health risks, individual countries have set maximum acceptable concentrations of PM within the atmosphere, based on the results of concentration prediction systems to estimate levels of PM1567.
In 2005, as outlined by the World Health Organization (WHO), the maximum acceptable annual average concentration of PM10 was ≤20 µg/m3, with a limit of ≤50 µg/m3 per 24-hour period. In Korea, the annual and daily average concentrations of PM10 are <50 and <100 µg/m3, respectively. The annual and daily average concentrations of PM2.5 are <15 and 35 µg/m3, respectively. Overall concentrations of PM10 and PM2.5 are above 81 µg/m3 and 36 µg/m3, respectively, and therefore the PM concentration forecast grade is designated as ‘bad’ in Korea (Tables 1, 2)18.
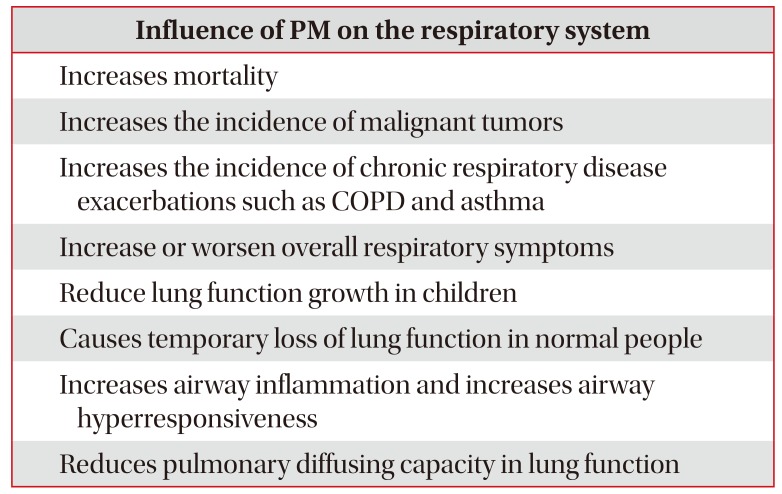
According to current literature, exposure to PM leads to increased pulmonary inflammation and respiratory symptoms aggravation due to oxidative stress and direct toxic injury56. This is particularly dangerous for patients with pre-existing respiratory diseases, as exposure to PM can lead to acute exacerbation of their ailment. It has also been reported that long-term exposure to high concentrations of PM increases the prevalence of chronic obstructive pulmonary disease (COPD) and lung cancer in adults, leading to a decline in pulmonary function9101112. The high concentration of PM in the atmosphere has a profound effect on the prevalence of chronic respiratory diseases, and the risk of acute exacerbation (which can prove fatal)1314. Additionally, PM2.5 exposure is associated with a long recovery time, more leading to an increase in both the mortality rate and the overall medical burden. Therefore, it is of the utmost importance that effective policies and medical practices are put into place to minimize the public health risks associated with PM exposure (Table 3)15.
Pulmonary function is an indicator of respiratory health. Generally, pulmonary function increases from birth until the mid-20s, after which it begins to decrease. Air pollution, especially PM exposure, is associated with decreased pulmonary function, leading to an increase in the rate of lung function decline in adults16171819.
Large-scale cohort studies of the effect of fine dust on pulmonary function in adults are typically based on National Health and Nutrition Examination Surveys (NHANEs). Notably, the Swiss Study on Air Pollution and Lung Diseases in Adults (SAPALDIA), and the German study on the Influence of Air Pollution on Lung Function, Inflammation, and Aging (SALIA), show interesting results. In the SAPALDIA study, 9,651 adults, aged 18–60 years, were monitored over a period of 11 years. The average forced vital capacity (FVC) and mean forced expiratory volume in 1 second (FEV1) decreased by 3.4% and 1.6%, respectively. The PM10 concentration declined during the observation period, which was associated with reduced lung function decline18. In the SALIA study, FEV1 and FVC decreased by 4.7% and 3.4%, respectively, and the FEV1/FVC decreased by 1.1%, with an increase in PM10 concentration by 10 µg/m3 between 1985 and 1994. Thus, lung function was negatively affected, but the decline in pulmonary function was attenuated by reducing PM exposure through environmental improvement13. However, it is not yet fully understood how other factors affect pulmonary function, such as age, other pollutants, individual susceptibility, and genetic factors.
COPD has been widely studied in relation to fine dust exposure in pulmonary diseases1820. Studies showed that the rate of hospitalization of patients suffering from COPD increased with increasing exposure to PM202122. A meta-analysis carried out in Korea showed that COPD admissions increased by ~2.7% (95% confidence interval [CI], 1.9%–3.6%) with an increase in PM10 concentration of 10 µg/m3 (odds ratio [OR], 1.027; 95% CI, 1.019–1.036). In addition, a positive correlation between an increase in PM10 concentration and COPD mortality was also found: COPD mortality increased by 1.1% (95% CI, 0.8%–1.4%) with an increase in PM10 concentration of 10 µg/m3 (OR, 1.011; 95% CI, 1.008–1.014)8. These results strongly suggest that exposure to PM increased both the hospital admission and mortality rate of COPD. Recent studies have shown that hospitalization due to deterioration of COPD is associated more with atmospheric concentrations of PM2.5 versus PM10. This is especially significant for the 14–90-day period prior to hospital admission (relative risk, 1.06–1.32)1415. About 1.6 million deaths from COPD are believed to be due to air pollution23. In Korea, there has been no detailed study on the effect of air pollution and PM on the aggravation of COPD patients; thus, further research is imperative to better understand the effect of PM exposure on COPD patients.
In addition to COPD, asthma has also been studied in relation to fine dust exposure424. Exposure to PM can cause allergic sensitization and asthma exacerbation2425. In asthmatic patients, both the exhaled nitric oxide fraction (FeNO) and airway hyperresponsiveness increases due to aggravation of the allergic inflammatory response. Moreover, asthmatic patients also show reduced lung volume or lung diffusion capacity24. Subsequently, PM exposure has been reported to lead to an increase in hospital visits as symptoms including decreased lung function, coughing, wheezing, and dyspnea worsen. In particular, PM2.5 significantly increased the incidence and prevalence of asthma. According to recent reports, for every 10 µg/m3 increase in PM2.5 concentration, the total number of hospital, out-patient, and emergency room visits increased by 0.67, 0.65, and 0.49%, respectively. These findings indicate a significant correlation between PM exposure and acute asthmatic exacerbations26. In addition, both domestic and international studies have shown that long-term exposure to PM increases the overall prevalence of asthma12.
In 2014, an international study of the relationship between air pollution and idiopathic pulmonary fibrosis (IPF) reported that concentrations of ozone and nitrogen dioxide in airborne fine dust were associated with acute exacerbation of IPF at 6 weeks after initial exposure27. A recent study reported that the FVC of IPF patients was reduced by 46 mL with an increase in PM10 exposure concentration of 5 µg/m3, indicating that the increase of PM was closely associated with the progression of IPF28. In the 2018 French cohort study, Cohorte Fibrose (COFI), it was reported that as the concentration of PM10 and PM2.5 increased by 10 µg/m3, the IPF mortality rate increased significantly, by 2.01- and 7.93-fold, respectively29. These results suggest that an increase in PM exposure significantly decreases pulmonary function, leading to an increase in mortality, as well as acute exacerbation, of IPF30.
In 2013, the WHO and the International Agency for Research on Cancer (IARC) announced that PM is carcinogenic31, and that increased atmospheric PM concentrations are associated with lung cancer development3233. In the European Study of Cohorts of Air Pollution Effects (ESCAPE), the hazard ratio of lung cancer was 1.22 and 1.18 for an increase in PM10 concentration of 10 µg/m3, and in PM2.5 of 5 µg/m3, respectively3435. In a comprehensive meta-analysis conducted in Korea in 2015, the risk of lung cancer increased by 1.09-fold (95% CI, 1.01–1.14) when the concentration of PM2.5 increased by 10 µg/m3. A correlation between PM10 concentration and lung cancer incidence was also observed; however, the correlation was comparatively weak compared to that between lung cancer risk and PM2.5 concentration (1.08-fold increased risk; 95% CI, 1.00–1.17)8. In addition, lung cancer incidence was higher in smokers who were exposed to high amounts of PM2.5; it was confirmed that fine PM affects smokers' lung cancer development to a significantly greater degree relative to healthy people63132. It is estimated that about 500,000 lung cancer deaths can be attributed to air pollution23. Both PM10 and PM2.5 were reported to significantly increase the mortality rate in lung cancer patients in 2017 and 2018 meta-analyses36. Thus, to reduce lung cancer prevalence and mortality, control of PM generation and avoidance of PM exposure, together with smoking cessation, are of the utmost importance33.
PM increases airway inflammation in the lungs, leading to increased levels of both inflammatory cytokines and neutrophils, and an increase in serum 8-isoprostane in bronchoalveolar lavage fluid or induced sputum2537. These findings accord with the incidence of pneumonia, and it is known that the risk and mortality rate of pneumonia increase in both children and adults with higher PM exposure343839. A recent meta-analysis showed that the incidence rate of pneumonia in children increased by 1.5% and 1.8% for every 10 µg/m3 increase in PM10 and PM2.5, respectively, demonstrating the relationship between PM and pneumonia11. In another meta-analysis, the overall mortality rate (relative risk, 1.02) of respiratory disease patients was significantly increased for every 10 µg/m3 increase of PM2.5 in fine dust10.
The most simple and common way to protect against airborne fine dust is to wear a mask that filters out fine dust or gas. Protective masks against PM used in Korea include the N95, KF94, and KF99 models. Such precautionary measures are vital, as natural air pollution phenomena, such as yellow sand, pose severe health risks in Korea. To specifically combat the danger posed by yellow sand, a specialized mask (KF80) has been developed40. Among filtering face respirators, the N95 and KF94 masks are the most commonly used, protecting the respiratory tract from fine dust exposure in industrial workers. These masks are also used to protect against respiratory pathogens in hospitals and public places41. Both the N95 and KF94 masks are superior to the KF80 mask in preventing PM inhalation. However, industrial workers who wear these masks for long periods tend to have subjective complaints, including discomfort when breathing. It is known that, in addition to carbon dioxide accumulation, a decrease in the concentration of inhaled oxygen can lead to an increase in respiratory dead space42. Although the N95 and KF94 masks have no significant effect on pulmonary function in healthy people or patients with mild respiratory issues, for patients with low pulmonary function and high levels of respiratory distress, caution should be taken when using these masks. All filtration masks (KF80, KF94, and N95) are commercially available and can prevent harmful exposure to PM due to the inflow of fine dust into the body. It is recommended that both the general public and people suffering from mild and moderate chronic respiratory diseases and/or cardiovascular diseases use these preventative measures4041. However, the use of N95 and KF94 masks by people with COPD (stage C/D), or advanced IPF is associated with severe respiratory failure; thus, caution is necessary regarding their use. Further research on the effectiveness of masks for preventing PM exposure is needed for patients with advanced respiratory diseases8.
Several studies have shown that exposure to high concentrations of PM leads to an increase in hospitalization and mortality rates in patients suffering from COPD. Acute exacerbation of bronchial asthma and IPF is also linked to high concentrations of PM. Long-term exposure to PM is associated with lung cancer development; particularly, high concentrations of PM2.5 have been linked with acute exacerbation and increased prevalence of chronic respiratory disease in smokers aged 60 years and over. Therefore, patients with chronic respiratory diseases are vulnerable to high concentrations of environmental PM and should limit outdoor activities and use medication regularly to reduce the risk of acute exacerbation. Visiting a medical institution for immediate treatment is recommended if any acute exacerbation symptoms are experienced. In addition, in high PM concentration environments, it is recommended that a face mask be worn to minimize exposure. However, for patients with chronic pulmonary diseases and very low pulmonary function, caution must be taken when using the N95 and KF94 masks. Numerous health problems are associated with PM exposure, all of which can lead to the progression and worsening of lung disease; thus, it is extremely important that national policy helps manage resources of PM and focuses on preventative medical care. Strengthening the notification system to vulnerable patients and proper management of PM production control are considered to be important factors in suppressing prevalence in chronic respiratory disease, decreasing the hospitalization rate, and reducing the mortality associated with acute exacerbations.
References
1. World Health Organization. WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide [Internet]. Geneva: World Health Organization;2005. cited 2019 Dec 10. Available from: http://whqlibdoc.who.int/hq/2006/WHO_SDE_PHE_OEH_06.02_eng.pdf.
2. World Health Organization. Ambient air pollution: a global assessment of exposure and burden of disease [Internet]. Geveva: World Health Organization;2016. cited 2019 Dec 10. Available from: http://apps.who.int/iris/bitstream/10665/250141/1/9789241511353-eng.pdf?ua=1.
3. Ministry of Environment. What is the particulate matter? [Internet]. Sejong: Ministry of Environment;2018. cited 2019 Dec 10. Available from: http://www.me.go.kr/ebook/svs/gt/view/159.
4. Yang HJ, Kim SH, Jang AS, Kim SH, Song WJ, Kim TB, et al. Guideline for the prevention and management of particulate matter/yellow dust-induced adverse health effects on the patients with bronchial asthma. J Korean Med Assoc. 2015; 58:1034–1043.

5. Dockery DW, Pope CA 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993; 329:1753–1759. PMID: 8179653.

6. Pope CA 3rd, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA. 2002; 287:1132–1141. PMID: 11879110.

7. WHO Regional Office for Europe Review of evidence on health aspects of air pollution - revihaap project: technical report. Copenhagen: WHO Regional Office for Europe;2013.
8. Kyung SY, Kim YS, Kim WJ, Park MS, Song JW, Yum H, et al. Guideline for the prevention and management of particulate matter/Asian dust particle-induced adverse health effect on the patients with pulmonary diseases. J Korean Med Assoc. 2015; 58:1060–1069.

9. Zhang S, Li G, Tian L, Guo Q, Pan X. Short-term exposure to air pollution and morbidity of COPD and asthma in East Asian area: a systematic review and meta-analysis. Environ Res. 2016; 148:15–23. PMID: 26995350.

10. Fajersztajn L, Saldiva P, Pereira LA, Leite VF, Buehler AM. Short-term effects of fine particulate matter pollution on daily health events in Latin America: a systematic review and meta-analysis. Int J Public Health. 2017; 62:729–738. PMID: 28255648.

11. Nhung NT, Amini H, Schindler C, Kutlar Joss M, Dien TM, Probst-Hensch N, et al. Short-term association between ambient air pollution and pneumonia in children: a systematic review and meta-analysis of time-series and case-crossover studies. Environ Pollut. 2017; 230:1000–1008. PMID: 28763933.

12. Abbey DE, Burchette RJ, Knutsen SF, McDonnell WF, Lebowitz MD, Enright PL. Long-term particulate and other air pollutants and lung function in nonsmokers. Am J Respir Crit Care Med. 1998; 158:289–298. PMID: 9655742.

13. Schikowski T, Adam M, Marcon A, Cai Y, Vierkotter A, Carsin AE, et al. Association of ambient air pollution with the prevalence and incidence of COPD. Eur Respir J. 2014; 44:614–626. PMID: 24488569.

14. Zielinski M, Gasior M, Jastrzebski D, Desperak A, Ziora D. Influence of particulate matter air pollution on exacerbation of chronic obstructive pulmonary disease depending on aerodynamic diameter and the time of exposure in the selected population with coexistent cardiovascular diseases. Adv Respir Med. 2018; 86:227–233. PMID: 30378650.

15. Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and metaanalysis. Thorax. 2014; 69:660–665. PMID: 24706041.
16. Gauderman WJ, McConnell R, Gilliland F, London S, Thomas D, Avol E, et al. Association between air pollution and lung function growth in southern California children. Am J Respir Crit Care Med. 2000; 162(4 Pt 1):1383–1390. PMID: 11029349.

17. Gehring U, Gruzieva O, Agius RM, Beelen R, Custovic A, Cyrys J, et al. Air pollution exposure and lung function in children: the ESCAPE project. Environ Health Perspect. 2013; 121:1357–1364. PMID: 24076757.

18. Downs SH, Schindler C, Liu LJ, Keidel D, Bayer-Oglesby L, Brutsche MH, et al. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med. 2007; 357:2338–2347. PMID: 18057336.
19. Pope CA 3rd, Ezzati M, Dockery DW. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009; 360:376–386. PMID: 19164188.

20. Gan WQ, FitzGerald JM, Carlsten C, Sadatsafavi M, Brauer M. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med. 2013; 187:721–727. PMID: 23392442.

21. Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016; 11:3079–3091. PMID: 28003742.

22. Sunyer J, Basagana X. Particles, and not gases, are associated with the risk of death in patients with chronic obstructive pulmonary disease. Int J Epidemiol. 2001; 30:1138–1140. PMID: 11689536.

23. Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung SH, Mortimer K, et al. Air pollution and noncommunicable diseases: a review by the Forum of International Respiratory Societies' Environmental Committee, part 2: air pollution and organ systems. Chest. 2019; 155:417–426. PMID: 30419237.
24. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014; 383:1581–1592. PMID: 24792855.

25. Thurston GD, Kipen H, Annesi-Maesano I, Balmes J, Brook RD, Cromar K, et al. A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J. 2017; 49:1600419. PMID: 28077473.

26. Tian Y, Xiang X, Juan J, Sun K, Song J, Cao Y, et al. Fine particulate air pollution and hospital visits for asthma in Beijing, China. Environ Pollut. 2017; 230:227–233. PMID: 28654880.

27. Johannson KA, Vittinghoff E, Lee K, Balmes JR, Ji W, Kaplan GG, et al. Acute exacerbation of idiopathic pulmonary fibrosis associated with air pollution exposure. Eur Respir J. 2014; 43:1124–1131. PMID: 24176998.

28. Winterbottom CJ, Shah RJ, Patterson KC, Kreider ME, Panettieri RA Jr, Rivera-Lebron B, et al. Exposure to ambient particulate matter is associated with accelerated functional decline in idiopathic pulmonary fibrosis. Chest. 2018; 153:1221–1228. PMID: 28802694.

29. Sese L, Nunes H, Cottin V, Sanyal S, Didier M, Carton Z, et al. Role of atmospheric pollution on the natural history of idiopathic pulmonary fibrosis. Thorax. 2018; 73:145–150. PMID: 28798214.

30. Carey IM, Atkinson RW, Kent AJ, van Staa T, Cook DG, Anderson HR. Mortality associations with long-term exposure to outdoor air pollution in a national English cohort. Am J Respir Crit Care Med. 2013; 187:1226–1233. PMID: 23590261.

31. Straif K, Cohen A, Samet J. Air pollution and cancer [Internet]. Lyon: International Agency for Research on Cancer;2013. cited 2019 Dec 10. Available from: http://www.iarc.fr/en/publications/books/sp161/AirPollutionandCancer161.pdf.
32. Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, et al. Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect. 2014; 122:906–911. PMID: 24911630.

33. Huang F, Pan B, Wu J, Chen E, Chen L. Relationship between exposure to PM2.5 and lung cancer incidence and mortality: a meta-analysis. Oncotarget. 2017; 8:43322–43331. PMID: 28487493.

34. MacIntyre EA, Gehring U, Molter A, Fuertes E, Klumper C, Kramer U, et al. Air pollution and respiratory infections during early childhood: an analysis of 10 European birth cohorts within the ESCAPE Project. Environ Health Perspect. 2014; 122:107–113. PMID: 24149084.
35. Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol. 2013; 14:813–822. PMID: 23849838.
36. Kim HB, Shim JY, Park B, Lee YJ. Long-term exposure to air pollutants and cancer mortality: a meta-analysis of cohort studies. Int J Environ Res Public Health. 2018; 15:E2608. PMID: 30469439.

37. Suhaimi NF, Jalaludin J. Biomarker as a research tool in linking exposure to air particles and respiratory health. Biomed Res Int. 2015; 2015:962853. PMID: 25984536.

38. Cai Y, Schikowski T, Adam M, Buschka A, Carsin AE, Jacquemin B, et al. Cross-sectional associations between air pollution and chronic bronchitis: an ESCAPE meta-analysis across five cohorts. Thorax. 2014; 69:1005–1014. PMID: 25112730.

39. Kyung SY, Jeong SH. Adverse health effects of particulate matter. J Korean Med Assoc. 2017; 60:391–398.

40. Langrish JP, Li X, Wang S, Lee MM, Barnes GD, Miller MR, et al. Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environ Health Perspect. 2012; 120:367–372. PMID: 22389220.

41. Langrish JP, Mills NL, Chan JK, Leseman DL, Aitken RJ, Fokkens PH, et al. Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol. 2009; 6:8. PMID: 19284642.

42. Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010; 55:569–577. PMID: 20420727.
Table 1
Overview of guidelines for particulate matter (PM)
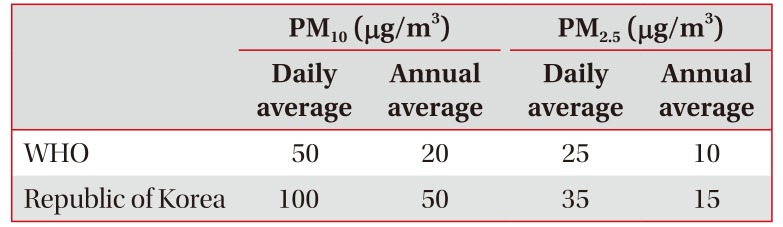
| PM10 (µg/m3) | PM2.5 (µg/m3) | |||
|---|---|---|---|---|
| Daily average | Annual average | Daily average | Annual average | |
| WHO | 50 | 20 | 25 | 10 |
| Republic of Korea | 100 | 50 | 35 | 15 |
Table 2
Particulate matter (PM) concentration forecast grade in Korea
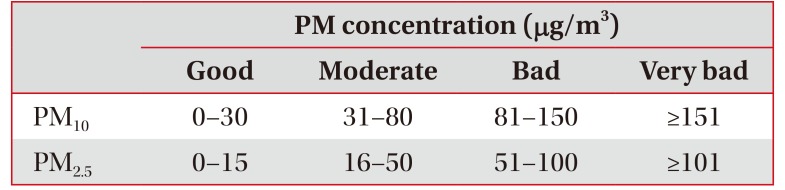
| PM concentration (µg/m3) | ||||
|---|---|---|---|---|
| Good | Moderate | Bad | Very bad | |
| PM10 | 0–30 | 31–80 | 81–150 | ≥151 |
| PM2.5 | 0–15 | 16–50 | 51–100 | ≥101 |
Table 3
Influence of PM on the respiratory system




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download