Abstract
We assessed the success rate of empirical antifungal therapy with itraconazole and evaluated risk factors for predicting the failure of empirical antifungal therapy. A multicenter, prospective, observational study was performed in patients with hematological malignancies who had neutropenic fever and received empirical antifungal therapy with itraconazole at 22 centers. A total of 391 patients who had abnormal findings on chest imaging tests (31.0%) or a positive result of enzyme immunoassay for serum galactomannan (17.6%) showed a 56.5% overall success rate. Positive galactomannan tests before the initiation of the empirical antifungal therapy (P=0.026, hazard ratio [HR], 2.28; 95% confidence interval [CI], 1.10-4.69) and abnormal findings on the chest imaging tests before initiation of the empirical antifungal therapy (P=0.022, HR, 2.03; 95% CI, 1.11-3.71) were significantly associated with poor outcomes for the empirical antifungal therapy. Eight patients (2.0%) had premature discontinuation of itraconazole therapy due to toxicity. It is suggested that positive galactomannan tests and abnormal findings on the chest imaging tests at the time of initiation of the empirical antifungal therapy are risk factors for predicting the failure of the empirical antifungal therapy with itraconazole.
Most patients with hematological malignancies belong to the intermediate-to-high risk group of infection (1). Among the various causes of infection, invasive fungal disease (IFD) is one of the most important causes of morbidity and mortality (2). European data report an overall incidence of 4.6% of IFD in patients with hematological malignancies (3). Therefore, early diagnosis and proper treatment of IFD is very important. However, it is difficult to make a definitive diagnosis of proven IFD because most patients with suspected IFD are usually hemodynamically unstable and accompanied by advanced coagulation deficits (4, 5). To overcome these issues, the use of empirical antifungal therapy for suspected IFD has been established for neutropenic cancer patients with persistent fever, despite the use of broad-spectrum antibiotics (6-9); and appropriate empirical antifungal therapy is still a very important strategy in the management of patients with hematological malignancies (10).
Although deoxycholate amphotericin B (D-AMB) has been used in empirical antifungal therapy, liposomal amphotericin B (L-AMB), itraconazole, voriconazole, or caspofungin are commonly recommended for empirical antifungal therapy (11, 12). Because the efficacies of these antifungal agents as an empirical antifungal therapy were similar (13-17), we could generalize the results of this study with itraconazole. The previous trials using itraconazole for empirical antifungal therapy enrolled a relatively small number of patients and used different criteria of success for empirical antifungal therapy (14, 18-20). Under such conditions, it was very difficult to compare the efficacy of itraconazole for empirical antifungal therapy with that of other antifungal agents. In addition, it is also difficult to evaluate risk factors for failure of empirical antifungal therapy.
This study was a multicenter, prospective, observational study conducted at 22 medical centers in Korea. Between July 2008 and March 2009, 438 patients with hematological malignancies who had persistent or recurrent neutropenic fever had been enrolled. The primary objective of this study was to evaluate the overall success rate of empirical antifungal therapy with itraconazole. The secondary objective was to define the risk factors for failure of empirical antifungal therapy with itraconazole. To compare the effect of the time to initiation of empirical antifungal therapy on the efficacy and safety of empirical antifungal therapy with itraconazole, we divided the patients into 2 groups (1-3 days vs ≥4 days after the onset of neutropenic fever) because empirical antifungal therapy is usually recommended when the fever does not resolve within 3-to-7 days of initial administration of antibacterial agents (5, 8, 9). Efficacy was assessed for the patients who received intravenous (IV) itraconazole for 3 or more days. Safety was assessed for all patients who received at least one dose of IV itraconazole.
Patients 18 yr or older with persistent (more than 2 days) or recurrent neutropenic fever despite empirical broad-spectrum systemic antibacterial therapy (9) were eligible. Fever was defined as a single oral temperature of above 38.3℃ or a temperature of above 38.0℃ for 1 hr (8, 9). Neutropenia was defined as an absolute neutrophil count (ANC)<500/µL, or an ANC<1,000/µL with a predicted decrease to below 500/µL (8, 9). We started the granulocyte colony stimulating factor (G-CSF) administration from the day of the ANC<1,000/µL until recovery of ANC>3,000/µL. The patients with possible or probable categories of IFD according to the European Organization for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) criteria were enrolled (4). Patients with a proven IFD were not eligible. However, we included patients with candidiasis. Other exclusion criteria were a history of hypersensitivity to itraconazole, a severe liver dysfunction (defined as a bilirubin level>3 times the upper limit of normal [ULN] or an aminotransferase/alkaline phosphatase level>5 times the ULN) and severe renal dysfunction (defined as a calculated creatinine clearance<30 mL/min) (21).
IV itraconazole (Janssen Pharmaceutica, Beerse, Belgium) at a dose of 200 mg was administered every 12 hr for the first 2 days, followed by 200 mg once a day for the 14th day at maximum. After using IV itraconazole, an oral solution form of itraconazole at a dose of 200-400 mg/day replaced IV itraconazole when necessary. The patients with no evidence of baseline or breakthrough fungal infections were recommended to continue empirical antifungal therapy with IV itraconazole until defervescence and recovery from neutropenia (ANC>500/µL for at least 3 successive days). The patients who received a combination therapy with other antifungal agents were excluded.
The efficacy assessments for empirical antifungal therapy have been determined by 5 endpoints that have been used in previous studies (13, 15, 16). Treatment was considered successful if all 5 of the following criteria were met: 1) successful treatment of any baseline fungal infection, 2) the absence of any breakthrough fungal infection, 3) survival for at least 7 days after discontinuation of itraconazole therapy, 4) resolution of fever (defined as a temperature below 38℃ for at least 2 days) during neutropenia, and 5) no premature discontinuation of the itraconazole therapy because of drug-related toxicity or lack of efficacy.
Baseline fungal infections were defined as those that developed within the first 48 hr after entry into the study (13, 15, 16). Breakthrough fungal infections were defined as those that occurred from the 3rd day of treatment of IV itraconazole therapy or within 7 days after completion of itraconazole therapy (13, 15, 16). The diagnosis of baseline or breakthrough fungal infection was confirmed when the patients were diagnosed as proven or probable IFD according to the EORTC/MSG consensus criteria (4).
The patients who received empirical IV itraconazole therapy between the 1st and 3rd day after initiation of antibacterial therapy for neutropenic fever were defined as the "early administration" group. And the other patients who used empirical IV itraconazole therapy from the 4th day of antibacterial therapy were considered as the "routine administration" group.
The safety assessments were performed according to the NCI Common Terminology Criteria for Adverse Effects, version 3.0 (22). Clinical adverse events were monitored prospectively and toxicities were defined as 2 or more grade toxicity and an increment of one or more grades above the baseline grade level.
The defervescence rate prior to the recovery of ANC expected in this study was 40%±10% based on the results of previous studies (14, 20). The calculated number of patients was 369 based on a 95% confidence interval (CI) with estimated differences of 10%. We also estimated a total sample size of 440 considering about a 15% drop-out rate. Categorical values were compared using a chi-square test or Fisher's exact test. Continuous variables were compared using an independent sample t-test. All results were considered statistically significant at P<0.05. Two-sided 95% CIs were calculated where appropriate. The multivariate logistic regression analysis using identified significant factors in univariate analysis was performed. All calculations were performed with the SPSS system, version 18.0 (SPSS, Inc., Chicago, IL, USA).
This study was conducted according to the Declaration of Helsinki and approved by institutional review board of Severance Hospital (IRB No. 4-2008-0232) and the institutional review boards of 21 other participating institutions. All subjected patients signed an informed consent. This study was registered on National Cancer Institute (NCI) website, NCT01060462.
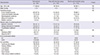
Among the 438 patients recruited, 9 were excluded because the patients did not receive IV itraconazole for 3 or more days while 38 patients were excluded because of inappropriate inclusion/exclusion criteria. A total of 391 patients was analyzed. The clinical characteristics are summarized in Table 1. The median age was 50 yr (range, 18-78 yr). At the initiation of empirical antifungal therapy, 291 patients (74.4%) had the status of residual hematological malignancies and 174 patients (44.5%) had a high score of Eastern Cooperative Oncology Group (ECOG) performance status (≥2). Co-morbidities were reported in 129 patients (33.0%). There were no differences in these clinical characteristics between the "early administration" group and the "routine administration" group (Table 1).
At the initiation of empirical antifungal therapy, 121 patients (31.0%) showed abnormalities (some evidence of infection) on chest X-rays or high-resolution computerized tomography (CT); and 23.2% of patients (22/95) had definite evidences of fungal infection on chest CT such as dense, well-circumscribed lesions(s) with or without a halo sign, air-crescent sign and cavity (4). Thirty-nine (17.6%) out of 221 patients had a positive result of enzyme immunoassay for serum galactomannan when using a cut-off index of 0.5 (23, 24). Among the 22 patients with definite evidences of fungal infection, 11 patients performed serum galactomannan tests and 4 patients showed a positive galactomannan test. The median duration of baseline (prior to starting IV itraconazole) neutropenia (ANC<500/µL) was 7 days (interquartile range, 4-11). Prolonged baseline neutropenia (>10 days) was observed in 29.4% (n=115) of the patients. The median duration of severe baseline neutropenia (ANC<100/µL) was 5 days (interquartile range, 2-9). Prolonged severe neutropenia (>10 days with ANC<100/µL) was observed in 61 patients (15.6%). Baseline duration of neutropenia was shorter in the patients from the "early administration" group compared with the "routine administration" group (Table 2). The median time to the start of empirical antifungal therapy with IV itraconazole after developing neutropenic fever was 2 days (range, 1-18 days).
Approximately half of patients had received antifungal prophylaxis (n=190, 48.6%) and about half of them received a fluconazole as antifungal prophylaxis. The rate of prophylactic use of antifungal agents was lower in the patients in the "early administration" group (43.1%) compared with the "routine administration" group (61.7%) (P=0.001, Table 2). Thirty patients (7.7%) had baseline fungal infections.
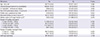
The median treatment duration of IV itraconazole for empirical antifungal therapy was 9 days (range, 3-41 days). Forty-five patients (11.5%) switched from IV to the oral solution itraconazole. The overall success rate was 56.5% and there was no significant difference in the success rate between the two groups (Table 3). Of the 30 patients with baseline fungal infections, 15 patients (50.0%) had a successful outcome. Among 20 patients with invasive aspergillosis as a baseline fungal infection, 10 patients had a successful outcome. The rate of breakthrough of fungal infections was 2.8% (11/391) and 9 of those patients were probable or proven invasive aspergillosis. Other breakthrough fungal infections were candidiasis (n=1) and coccidioidomycosis (n=1). The proportion of patients who survived for at least 7 days after completion of itraconazole therapy was 94.1% and the rate of resolution of fever during the neutropenic period was 59.3%. Premature discontinuation of itraconazole therapy because of toxicity or lack of efficacy occurred in 96 patients (24.6%). After failure of empirical antifungal therapy with itraconazole, 76 patients (19.4%) received second-line IV antifungal therapies with D-AMB (n=71), L-AMB (n=2), caspofungin (n=1), fluconazole (n=1), or voriconazole (n=1). The success rate was significantly lower in the patients with positive galactomannan test and/or definite evidences of fungal infection on imaging study (pre-emptive therapy, 42.1%, 24/57) than the patients with negative galactomannan test and no evidences of fungal infection (58.9%, 103/175, P=0.032)
Adverse events that might be related to itraconazole developed in 79 patients (18.0%). Hepatotoxicity (n=68, 15.5%) and nephrotoxicity (n=11, 2.5%) were commonly observed. Three patients experienced a generalized skin rash. Eight patients (2.0%) had premature discontinuation of itraconazole therapy due to toxicity. The causes of withdrawal from itraconazole therapy were hepatotoxicity (n=6), nephrotoxicity (n=2) and skin toxicity (n=1).
There were no significant differences in success rates according to the underlying hematological malignancies (Table 4). The patients with cardiovascular co-morbidity were relatively less likely to achieve a successful outcome with empirical antifungal therapy (P=0.056). Abnormal findings on chest X-rays or CT and positive galactomannan tests before initiation of empirical antifungal therapy were significantly associated with decreased success rates (P=0.006, P=0.033, respectively).
Multivariate analysis revealed that positive galactomannan tests before initiation of empirical antifungal therapy (P=0.026, hazard ratio [HR], 2.28; 95% CI, 1.10-4.69) and abnormal findings on chest X-rays or CT before initiation of empirical antifungal therapy (P=0.022, HR, 2.03; 95% CI, 1.11-3.71) were significantly associated with poor outcomes of empirical antifungal therapy with itraconazole.
The success rate of empirical antifungal therapy in the patients with positive baseline galactomannan tests was 38.5%. A total of 13 baseline fungal infections in 39 patients with positive baseline galactomannan tests developed due to Aspergillus and 5 (38.5%) out of 13 patients were successfully treated. Among the patients with positive baseline galactomannan tests, premature discontinuation of itraconazole therapy because of a lack of efficacy occurred in 46.2% (Table 5). The success rate of empirical antifungal therapy in the patients with abnormal findings on chest X-rays or CT was 46.3%. Meanwhile, 33.9% engaged in premature discontinuation of itraconazole therapy because of a lack of efficacy.
We demonstrated that empirical antifungal therapy with itraconazole is effective and safe in Korean patients with hematological malignancies. In this study, we analyzed the success rate using the 5 well-known criteria for success of empirical antifungal therapy (13, 15, 16) and reported a 56.5% overall success rate, which was comparable to previous trials with other antifungal agents (13, 15, 16). Moreover, we also reported that positive galactomannan tests and abnormal findings on the chest imaging tests were risk factors for failure of empirical antifungal therapy with itraconazole.
Although empirical antifungal therapy was usually recommended 3-to-7 days after the onset of neutropenic fever (5, 8, 9), early application of empirical antifungal therapy could be possible in patients with high risk factors for developing IFD. Therefore, there were no limitations for the time to initiation of empirical antifungal therapy in this study. The median time to start empirical antifungal therapy with IV itraconazole was 2 days after the onset of neutropenic fever. Because the rate of antifungal prophylaxis was lower in the "early administration" group, many doctors preferred the early use of empirical antifungal agent in spite of the short duration of neutropenia. In this study, 291 patients (74.4%) were considered as the high-risk patients for IFD because of residual underlying disease and only about 50% of patients received antifungal prophylaxis in spite of general recommendation of antifungal prophylaxis for high-risk patients (25). Furthermore, antifungal agents with weak anti-mold activity were used in about 60% of patients. Therefore, we could use these data for analyzing risk factors for failure of empirical antifungal therapy in spite of relatively early start of empirical antifungal therapy.
Because there was no significant difference in the success rate between the "early administration" group and the "routine administration" group in this study, we could not consider the time to initiation of empirical antifungal therapy as a risk factor for failure of empirical antifungal therapy. Although empirical antifungal therapy is still recommended because of a high rate of mortality and morbidity of IFD (6, 7), a pre-emptive approach in which a patient with suspected IFD is treated according to the radiologic studies or laboratory markers such as the galactomannan test has recently been emphasized to minimize toxicities and costs related to antifungal therapy (17, 26). Therefore, we should consider the early application of pre-emptive therapy only in the patients with some evidence of IFD.
The diagnosis of pulmonary IFD is typically difficult because invasive diagnostic approaches are not easily available and the findings of chest CT are very diverse according to the underlying disease and ANC (27). Therefore, a serum assay for galactomannan has been considered as the most important test for the diagnosis of invasive aspergillosis because of its noninvasive blood test with high sensitivity and specificity (28). The serum galactomannan test can be used for predicting the clinical outcome in patients with probable or proven invasive aspergillosis (29), but little is known about the role of the serum galactomannan test in the setting of empirical antifungal therapy. In this study, 39 patients with a positive galactomannan test prior to initiation of empirical antifungal therapy were associated with a low success rate (38.5%). There were more premature discontinuations of itraconazole therapy in the patients with positive baseline galactomannan tests (n=19, 48.7%) than in the patients with negative baseline galactomannan tests (23.6%, P=0.003). Because these patients had poor outcomes of empirical antifungal therapy even after receiving the empirical antifungal therapy for a sufficient duration (median 9 days), it seems reasonable to consider the positive baseline galactomannan test as a risk factor for failure of empirical antifungal therapy. Therefore, we may need to consider more potent or combination antifungal therapies in the patients with a positive galactomannan test prior to initiation of empirical itraconazole therapy. Because the early trend of serum galactomannan levels in the course of IFD might be useful in predicting eventual clinical outcomes (30, 31), we could consider the early trend of the galactomannan test during the empirical antifungal therapy when we suspected failure of empirical antifungal therapy.
In this study, the presence of abnormal findings on chest imaging tests was also considered an independent risk factor for predicting the failure of empirical antifungal therapy. There was a significantly higher incidence of abnormal findings on chest imaging tests in elderly (≥60 yr old) patients (54.5% vs 26.0%, P=0.036) and the patients with underlying lung disease (73.9% vs 28.3%, P<0.001). Because abnormal findings on chest imaging tests are usually associated with underlying bacterial infections, high-resolution CT before initiating empirical antifungal therapy is required to find out whether or not the lesions are related to IFD (4, 5, 11). Although the patients with abnormal findings on chest X-rays or CT also experienced a higher rate of premature discontinuations of itraconazole therapy (38.0% vs 25.5%, P<0.001), these results might be analyzed with caution because there were relatively few patients who performed CT (n=95, 24.3%) and few patients with definite evidence of fungal infection on CT (n=22, 5.6%). Among the 39 patients with positive baseline galactomannan tests, 36 patients had normal findings on chest X-rays. Therefore, we should perform a high-resolution CT regardless of the results of chest X-rays if we consider the empirical antifungal therapy.
There were several limitations of this study. Because this study was conducted in the form of an observation study at 22 different institutions, we did not standardize the initial antibiotic therapy for neutropenic fever and prophylactic antifungal therapy. Two distinct host factors for developing IFD are prolonged neutropenia (>10 days) and allogeneic hematopoietic stem cell transplantation (HSCT) (4). However, we had relatively few patients with prolonged baseline neutropenia (29.4%) and few patients who received an allogeneic HSCT (4.1%). Because this observational study was closer to actual clinical practice and a sufficient number of patients for evaluating the characteristics of empirical antifungal therapy were enrolled in this study, the results from this population could be useful for clinical application. Because we did not evaluate the effect of blood concentration of itraconazole on the success rate in this study, we try to make a protocol with therapeutic drug monitoring in a future trial.
In conclusion, this study demonstrated that itraconazole was effective and safe in Korean patients with hematological malignancies. Positive galactomannan tests and abnormal findings on chest imaging tests at the time of initiation of empirical antifungal therapy are risk factors for failure of empirical antifungal therapy with itraconazole. Therefore, we should confirm the results of serum galactomannan tests and high-resolution CT before initiation of empirical antifungal therapy to estimate the results of empirical antifungal therapy.
Figures and Tables
Notes
References
1. Baden LR, Bensinger W, Angarone M, Casper C, Dubberke ER, Freifeld AG, Garzon R, Greene JN, Greer JP, Ito JI, et al. Prevention and treatment of cancer-related infections. J Natl Compr Canc Netw. 2012; 10:1412–1445.
2. Pagano L, Caira M, Candoni A, Offidani M, Martino B, Specchia G, Pastore D, Stanzani M, Cattaneo C, Fanci R, et al. Invasive aspergillosis in patients with acute myeloid leukemia: a SEIFEM-2008 registry study. Haematologica. 2010; 95:644–650.
3. Pagano L, Caira M, Candoni A, Offidani M, Fianchi L, Martino B, Pastore D, Picardi M, Bonini A, Chierichini A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006; 91:1068–1075.
4. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008; 46:1813–1821.
5. Ruhnke M, Böhme A, Buchheidt D, Cornely O, Donhuijsen K, Einsele H, Enzensberger R, Hebart H, Heussel CP, Horger M, et al. Diagnosis of invasive fungal infections in hematology and oncology: guidelines from the Infectious Diseases Working Party in Haematology and Oncology of the German Society for Haematology and Oncology (AGIHO). Ann Oncol. 2012; 23:823–833.
6. Wingard JR. Empirical antifungal therapy in treating febrile neutropenic patients. Clin Infect Dis. 2004; 39:S38–S43.
7. Martino R, Viscoli C. Empirical antifungal therapy in patients with neutropenia and persistent or recurrent fever of unknown origin. Br J Haematol. 2006; 132:138–154.
8. Lee DG, Kim SH, Kim SY, Kim CJ, Park WB, Song YG, Choi JH. Evidence-based guidelines for empirical therapy of neutropenic fever in Korea. Korean J Intern Med. 2011; 26:220–252.
9. Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011; 52:427–431.
10. Wingard JR, Carter SL, Walsh TJ, Kurtzberg J, Small TN, Baden LR, Gersten ID, Mendizabal AM, Leather HL, Confer DL, et al. Randomized, double-blind trial of fluconazole versus voriconazole for prevention of invasive fungal infection after allogeneic hematopoietic cell transplantation. Blood. 2010; 116:5111–5118.
11. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008; 46:327–360.
12. Maertens J, Marchetti O, Herbrecht R, Cornely OA, Flückiger U, Frêre P, Gachot B, Heinz WJ, Lass-Flörl C, Ribaud P, et al. European guidelines for antifungal management in leukemia and hematopoietic stem cell transplant recipients: summary of the ECIL 3: 2009 update. Bone Marrow Transplant. 2011; 46:709–718.
13. Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz C, Bodensteiner D, Pappas P, Seibel N, Greenberg RN, Dummer S, et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia: National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med. 1999; 340:764–771.
14. Boogaerts M, Winston DJ, Bow EJ, Garber G, Reboli AC, Schwarer AP, Novitzky N, Boehme A, Chwetzoff E, De Beule K. Intravenous and oral itraconazole versus intravenous amphotericin B deoxycholate as empirical antifungal therapy for persistent fever in neutropenic patients with cancer who are receiving broad-spectrum antibacterial therapy: a randomized, controlled trial. Ann Intern Med. 2001; 135:412–422.
15. Walsh TJ, Pappas P, Winston DJ, Lazarus HM, Petersen F, Raffalli J, Yanovich S, Stiff P, Greenberg R, Donowitz G, et al. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med. 2002; 346:225–234.
16. Walsh TJ, Teppler H, Donowitz GR, Maertens JA, Baden LR, Dmoszynska A, Cornely OA, Bourque MR, Lupinacci RJ, Sable CA, et al. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med. 2004; 351:1391–1402.
17. Klastersky J. Antifungal therapy in patients with fever and neutropenia: more rational and less empirical? N Engl J Med. 2004; 351:1445–1447.
18. Schuler U, Bammer S, Aulitzky WE, Binder C, Böhme A, Egerer G, Sandherr M, Schwerdtfeger R, Silling G, Wandt H, et al. Safety and efficacy of itraconazole compared to amphotericin B as empirical antifungal therapy for neutropenic fever in patients with haematological malignancy. Onkologie. 2007; 30:185–191.
19. Ohta K, Nishiki Kosaka S, Nakao Y, Kumura T, Hagihara K, Sakamoto E, Okamoto S, Hirose A, Aoyama Y, Yamamura R, et al. Efficacy and safety of intravenous itraconazole as empirical antifungal therapy for persistent fever in neutropenic patients with hematological malignancies in Japan. Int J Hematol. 2009; 89:649–655.
20. Park SH, Choi SM, Lee DG, Choi JH, Yoo JH, Min WS, Shin WS. Intravenous itraconazole vs. amphotericin B deoxycholate for empirical antifungal therapy in patients with persistent neutropenic fever. Korean J Intern Med. 2006; 21:165–172.
21. KDOQI. KDOQI Clinical Practice Guideline and Clinical Practice Recommendations for anemia in chronic kidney disease: 2007 update of hemoglobin target. Am J Kidney Dis. 2007; 50:471–530.
22. National Cancer Institute. Common terminology criteria for adverse events (CTCAE) v3.0. accessed on 10 August 2013. Available at http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.
23. Maertens JA, Klont R, Masson C, Theunissen K, Meersseman W, Lagrou K, Heinen C, Crépin B, Van Eldere J, Tabouret M, et al. Optimization of the cutoff value for the Aspergillus double-sandwich enzyme immunoassay. Clin Infect Dis. 2007; 44:1329–1336.
24. Leeflang MM, Debets-Ossenkopp YJ, Visser CE, Scholten RJ, Hooft L, Bijlmer HA, Reitsma JB, Bossuyt PM, Vandenbroucke-Grauls CM. Galactomannan detection for invasive aspergillosis in immunocompromized patients. Cochrane Database Syst Rev. 2008; (4):CD007394.
25. Robenshtok E, Gafter-Gvili A, Goldberg E, Weinberger M, Yeshurun M, Leibovici L, Paul M. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2007; 25:5471–5489.
26. Cordonnier C, Pautas C, Maury S, Vekhoff A, Farhat H, Suarez F, Dhédin N, Isnard F, Ades L, Kuhnowski F, et al. Empirical versus preemptive antifungal therapy for high-risk, febrile, neutropenic patients: a randomized, controlled trial. Clin Infect Dis. 2009; 48:1042–1051.
27. Bergeron A, Porcher R, Sulahian A, de Bazelaire C, Chagnon K, Raffoux E, Vekhoff A, Cornet M, Isnard F, Brethon B, et al. The strategy for the diagnosis of invasive pulmonary aspergillosis should depend on both the underlying condition and the leukocyte count of patients with hematologic malignancies. Blood. 2012; 119:1831–1837.
28. Maertens J, Verhaegen J, Lagrou K, Van Eldere J, Boogaerts M. Screening for circulating galactomannan as a noninvasive diagnostic tool for invasive aspergillosis in prolonged neutropenic patients and stem cell transplantation recipients: a prospective validation. Blood. 2001; 97:1604–1610.
29. Miceli MH, Grazziutti ML, Woods G, Zhao W, Kocoglu MH, Barlogie B, Anaissie E. Strong correlation between serum aspergillus galactomannan index and outcome of aspergillosis in patients with hematological cancer: clinical and research implications. Clin Infect Dis. 2008; 46:1412–1422.
30. Nouér SA, Nucci M, Kumar NS, Grazziutti M, Barlogie B, Anaissie E. Earlier response assessment in invasive aspergillosis based on the kinetics of serum Aspergillus galactomannan: proposal for a new definition. Clin Infect Dis. 2011; 53:671–676.
31. Chai LY, Kullberg BJ, Johnson EM, Teerenstra S, Khin LW, Vonk AG, Maertens J, Lortholary O, Donnelly PJ, Schlamm HT, et al. Early serum galactomannan trend as a predictor of outcome of invasive aspergillosis. J Clin Microbiol. 2012; 50:2330–2336.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download