INTRODUCTION
AO type C pelvic ring injuries are complete disruption of anterior or posterior pelvic rings following a severe traumatic force. The most common cause of this type of injury is motor vehicle accident. Other mechanisms include falls and crush injuries. Management of pelvic ring injuries are either closed reduction and external fixation or open reduction and internal fixation. External fixation is used in early emergency care or when internal fixation is not feasible for an open fracture. The disadvantages of external fixation are difficulty of anatomical reduction, insufficient stability due to loss of reduction, pin loosening, secondary infection and scarring1,2). Open reduction and internal fixation allows excellent anatomical reduction and stable fixation with a favorable prognosis3,4). Many authors have underscored the significance of solid internal fixation in the posterior pelvic ring5,6,7), yet, Kim et al.2) and Kim et al.8) suggested that despite the importance of posterior fixation, acceptable anterior pelvic ring fixation is also indispensable. Open reduction and internal fixation may incur complications including surgical site infection and neuromuscular injury due to soft tissue injury that is caused by surgical incision9).
We conducted a retrospective study on patients who had undergone an initial treatment for the ligamentous injury and received additional fixation for unstable or displaced pelvic fractures to evaluate the radiologic and clinical outcomes of AO type C pelvic ring injury and identify the prognostic factors.
MATERIALS AND METHODS
We studied 53 patients who were admitted to our hospital due to unstable type C pelvic ring injuries (AO classification) and underwent open reduction and internal fixation from January 2002 to February 2010 with a minimum follow-up of one year. Our study encompassed 34 men and 19 women with a mean age of 42.4 years (range, 22-67 years) and a mean follow-up of 14 months (range, 12-25 months). There were 8 cases of AO type C1-1, 19 cases of C1-2, 11 cases of C1-3, 6 cases of C2 and 9 cases of C3 injury. The mechanism of injury was car-pedestrian accident in 17 cases, traffic collision in 14 cases, motorcycle accident in 9 cases, crush injury in 6 cases, fall in 4 cases and injury from a heavy falling object in 3 cases. The most common associated injury was lower extremity injury in 48 cases followed by upper extremity injury in 25 cases, spinal injury in 20 cases, abdominal injury in 20 cases, head injury in 11 cases and neurologic injury in 8 cases. The mean number of associated injuries was 2.5. Due to a relatively poor general condition stemming from associated injuries, the mean time from injury to operation was 7.8 days (range, 4-19 days).
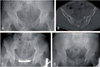
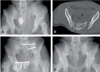
Pure ligamentous injuries were initially fixed that include separation of the symphysis pubis or sacroiliac joint dislocation. Additional fixation was performed in patients with unstable pelvic ring or severe displacement greater than 10 mm. Anterior fixation was achieved using a pelvic reconstruction plate through the Pfannenstiel incision or ilio-inguinal approach in the supine position. Posterior fixation was accomplished with open reduction using one or two 6.5 mm cancellous screws in the prone position. Fourteen patients received plate fixation of the symphysis pubis (Fig. 1) and fourteen patients received simultaneous plate fixation of the symphysis pubis and screw fixation of the sacroiliac joint (Fig. 2). Screw fixation of the sacroiliac joint was performed in 26 cases. No difference was found between the fixation methods according to the injury classification (Table 1). Joint exercise was performed, actively or passively, for hip and knee to prevent stiffness after 2-3 days postoperatively. Patients were recommended to attain a sitting position 2 weeks after the surgery and wheelchair ambulation was started at the 3rd week postoperatively. Partial weight bearing was started 6 weeks after the surgery.
For radiologic evaluation, antero-posterior, inlet and outlet views of pelvic bone were taken at final follow-up to measure the degree of displacement. According to Matta and Saucedo criteria10), displacements of less than 4 mm are excellent, 4-10 mm are good, 10-20 mm are fair and more than 20 mm displacements are poor.
For clinical evaluation, Majeed11) score system was used. Majeed score is made up of 7 sections: pain (30 points), work (20 points), sitting (10 points), walking aids (12 points), unaided gait (12 points), walking distance (12 points) and sexual intercourse (4 points). Out of a perfect Majeed score of 100 points, scores over 85 are excellent, 70-84 are good, 56-69 are fair and scores below 55 are poor.
Mann-Whitney test was used to compare the radiologic outcomes and Majeed scores according to injury classification, Majeed scores according to reduction degree and fixation method of fracture and Majeed scores according to AO classification. Majeed scores according to gender, age, mechanism of injury, AO classification, degree of reduction, fixation method and presence of neurologic injury were analyzed using logistic regression to identify prognostic factors.
RESULTS
At the final follow-up, the radiologic outcomes according to Matta and Saucedo criteria10) were excellent in 31 cases, good in 17 cases and fair in 5 cases with a mean displacement of 5.23 mm (range, 1.61-13.6 mm). No difference was found according to injury classification (Table 2). The mean Majeed score was 86.2 points (range, 57-100 points): excellent in 36 cases, good in 15 cases, fair in 2 cases and no poor cases. According to injury types, Majeed score was 87.1 points in AO type C1-1, 86.5 points in type C1-2, 82.7 points in type C1-3, 85.8 points in type C2, and 84.3 points in type C3 injury. Although the score was lowest in type C1-3, no statistically significant difference was observed (P=0.085, Table 3).
According to the degree of reduction, Majeed score was 86.8 points in excellent patients, 86.3 points in good patients and 83.4 points in fair patients, but no statistically significant difference was found (P=0.086, Table 4). According to fixation method, Majeed score was 86.4 points in the group with only anterior fixation, 87.3 points in the group with only posterior fixation and 85.9 points in the group with antero-posterior fixation. However, there was no statistically significant difference (P=0.975).
Lumbosacral plexus injury was seen in 7 out of 8 patients with neurologic injuries, and sciatic nerve injury was detected in one patient. There were 1 case of type C1-1, 2 cases of type C1-2, 2 cases of type C1-3, 1 case of type C2 and 2 cases of type C3 injury, showing no difference in frequency according to AO classification. Although injuries were improved at the final follow-up, Majeed score was 76.6 points due to incomplete recovery. This score was significantly lower than 88.2 points in 45 patients without neurologic injuries (P=0.025).
Logistic regression analysis on prognostic factors showed that gender (P=0.858), age (P=0.975), mechanism of injury (P=0.085), AO classification (P=0.098), degree of reduction (P=0.754) and fixation method (P=0.875) were not associated with prognosis, while neurologic deficit had a statistically significant association (P=0.042).
Postoperative complications were non-union and deep infection, each in one patient. The patient with non-union after plate fixation of the symphysis pubis and screw fixation of the sacroiliac joint in AO type C3 classification, gained union at 9th month postoperatively by conducting antero-posterior plate fixation at the 6th postoperative month to manage loosening of fixation plate and screw. The patient with deep infection after plate fixation of the symphysis pubis was treated with marginal excision after plate removal and administration of antibiotics.
DISCUSSION
In the past, skeletal traction or pelvic external fixation had been used to treat unstable pelvic ring injuries. Since fracture reduction and solid fixation are difficult to achieve only with external fixation, internal fixation is the preferred method of treatment in recent years. Tile5), Lindahl and Hirvensalo6), and Oh and Hwang7) suggested that solid fixation of the sacroiliac joint is required because sacroiliac joint fixation is important in maintaining the stability of the pelvic ring. Matta12) showed that internal fixation is essential for dislocations caused by pure ligamentous injuries, while union can be achieved relatively easier in pubic ramus fractures without internal fixation. Kim et al.2) and Kim et al.8) reported that although posterior fixation is important, adequate fixation is additionally required in the anterior pelvic ring to manage type C pelvic ring injuries. Dislocated sites with pure ligamentous injuries are initially fixed, and later, additional internal fixation of fractured sites is performed when a severe fracture displacement or an unstable pelvic ring is detected. Compared to the outcome of patients with simultaneous anterior and posterior fixations, satisfactory results were obtained in patients that received either anterior or posterior fixation.
Based on the clinical outcome according to the degree of postoperative reduction, Lindahl et al.13) and Oh et al.3) reported poor prognosis when a displacement of over 10 mm remains. Additionally, Matta and Saucedo10) also found favorable clinical outcomes when the displacement of the fracture is less than 10 mm. Majeed score had a tendency to be lower when a displacement of over 10 mm remained, but there was no statistically significant difference. The outcome is thought to be attributable to a small number of patients having a displacement over 10 mm and a small degree of displacement less than 13.6 mm, showing no statistically significant difference.
Neurologic injuries are commonly associated with unstable pelvic ring injuries and the clinically manifested symptoms are lower extremity motor dysfunction, pain from nerve injury, erectile dysfunction and hypesthesia that lead to unfavorable clinical prognosis due to restrictions of function and daily life activities14,15). Lee et al.16) found neurologic injuries in 2 out of 23 patients. Tornetta et al.17) showed that nerve injuries occur more frequently than fracture-dislocation of the sacroiliac joint in case of sacral fracture or pure dislocation of the sacroiliac joint. They also reported thy patients with nerve injuries had unfavorable outcomes. In a study by Lindahl and Hirvensalo6), lumbosacral plexus injuries were identified in 40 out of 101 patients who underwent surgical treatment for type C pelvic ring injuries with poor clinical prognosis in 18 patients with incomplete motor recovery. According to Kim et al.8), nerve injuries were observed in 12 out of 25 patients who underwent surgical treatment of type C pelvic ring injuries and the clinical prognosis was poorer in patients with nerve injuries compared to those without nerve injury. In our study, nerve injuries were identified in 8 (15%) out of 53 patients and Majeed scores were significantly lower in patient with nerve injuries.
Our study is limited by the relatively small sample size in each group. Since nerve injuries were evenly distributed in each group, other variables had no significant difference in clinical outcome. Further studies with larger sample sizes are warranted.
CONCLUSION
Satisfactory radiologic and clinical outcomes were obtained with dislocated sites with pure ligamentous injuries are initially fixed, and later, additional internal fixation of fractured sites is performed when a severe fracture displacement or an unstable pelvic ring is detected.
Majeed score was significantly lower in patients with nerve injury. Therefore, nerve injury is thought to be a crucial factor in clinical outcome.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download