Abstract
Primary diffuse large B-cell lymphoma of the seminal vesicle is an extremely rare disorder, with only two cases reported in the English literature. Here, we present imaging findings of a case of primary diffuse large B-cell lymphoma of the seminal vesicle. On transrectal ultrasonography, the mass presented as a 3.0-cm-sized heterogeneous, hypoechoic lesion in the right seminal vesicle. Computed tomography (CT) revealed a mass with rim-like enhancement in the right seminal vesicle. On magnetic resonance imaging (MRI), the tumor showed iso-signal intensity on T1-weighted images and heterogeneously intermediate-high signal intensity on T2-weighted images. The tumor showed rim-like and progressive enhancement with non-enhancing portion on dynamic scanning. Diffusion restriction was observed in the mass. On fluorodeoxyglucose positron emission tomography-computed tomography (FDG PET/CT) imaging, a high standardized uptake value (maxSUV, 23.5) by the tumor was noted exclusively in the right seminal vesicle.
Tumors of the seminal vesicles may be either primary or secondary tumor spread from adjacent organs, such as the prostate, bladder, rectum, or lymphoma (1). Primary neoplasms of the seminal vesicles are a rare and poorly understood entity. The criteria for the diagnosis of primary seminal vesicle tumor are as follows: No other demonstrable tumor present in the body; the tumor should be verified as localized in the seminal vesicle; and tumor invading from surrounding organs should be excluded (23).
Primary diffuse large B-cell lymphoma of the seminal vesicle is an extremely rare disorder, with only two cases reported in English literature (45).
We record here an extremely rare case of primary diffuse large B-cell lymphoma of the seminal vesicle. To our knowledge, the radiologic findings of this entity have seldom been described, due to its rarity. We present here the ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and [18F]-fluorodeoxyglucose positron emission tomography-computed tomography (FDG PET/CT) findings in this case of primary diffuse large B-cell lymphoma.
A 58-year-old man was presented with dysuria and erectile dysfunction for 1 year. The patient had a medical history of diabetes mellitus. On admission, physical examination showed no abnormal findings. Laboratory tests revealed an elevated level of prostate-specific antigen (PSA, 7.35 ng/ml). Urinalysis results and creatinine levels were normal.
On transrectal ultrasonography (TRUS), no evidence of prostate cancer was found. Rather, we found a 3.0-cm-sized heterogeneous, hypoechoic mass lesion in the right seminal vesicle (Fig. 1).
Abdominopelvic computed tomography (APCT) was performed, revealing a 4.1 × 3.0 cm sized well-defined mass with rim-like enhancement in the right seminal vesicle on portal venous phase. No significantly enlarged regional lymphadenopathy was found, and no other abnormal finding was seen on APCT.
Subsequently, we performed gadolinium-enhanced MRI. The tumor was shown to be of iso-signal intensity on T1-weighted images (T1WI), and heterogeneously intermediate-high signal intensity on T2-weighted images (T2WI) compared to signal intensity of adjacent muscle. Similar to CT finding, rim-like enhancement was shown on 3-min delayed phase images. On 5-min delayed phase enhancement scanning, the tumor showed progressive enhancement with a non-enhancing portion. On diffusion-weighted imaging (DWI), the mass had high signal intensity on high b-value (1000 s/mm2) and reduced apparent diffusion coefficient (ADC) values (Fig. 2).
On FDG PET/CT imaging, we found a high standardized uptake value (maxSUV, 23.5) exclusively in the tumor of the right seminal vesicle.
The differential diagnosis of malignant tumor of the seminal vesicle includes adenocarcinoma, squamous cell carcinoma, sarcoma, neuroendocrine tumor, and lymphoma. Since such lesions may appear as either a mass or an infiltrating lesion with enhancement in the seminal vesicle, they cannot be differentiated based on imaging findings (16).
To confirm histopathological diagnosis, ultrasound-guided needle biopsy was performed. Hematoxylin-eosin (HE) staining showed diffuse proliferation of a large neoplastic lymphoid area, suggestive of large cell lymphoma. The lymphoma cells showed positive immunohistochemical staining for CD20, a specific marker of B-cell lymphoma; partially positive staining for CD3, CD5, CD79α, LCA, and Ki-67; and negative staining for CD21, CD30, C-kit, and AFP. Thus, the overall histopathological and immunohistochemical findings were suggestive of diffuse large B-cell lymphoma. Bone marrow biopsy did not reveal lymphomatous involvement (Fig. 3).
The patient was treated with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone). After 3 months, on follow-up CT the primary diffuse large B-cell lymphoma in the seminal vesicle had disappeared. There was no significant uptake of FDG in the seminal vesicle on follow-up FDG PET/CT.
The genitourinary (GU) system is commonly affected by disseminated lymphoma, also known as secondary extranodal disease. Rarely, lymphoma can originate from and remain localized to one of the GU organs and thus presents as primary extranodal disease. Although lymphoma more commonly manifests as nodal disease affecting lymph nodes and lymphoid organs (such as the spleen, thymus, tonsils, and pharyngeal lymphatic ring), up to 40% of lymphoma cases present as extranodal disease with only 3% having the GU system as the primary site of involvement (7).
Only two cases of primary diffuse large B-cell lymphoma in the seminal vesicle are reported in the English literature (Table 1). The first of these, a primary diffuse large B-cell lymphoma of the seminal vesicle, showed a heterogeneous, echogenic mass on ultrasound and a homogenously enhancing mass on CT (4). But, in our case the tumor showed rim-like enhancement on portal venous phase images of CT and 3-min delayed phase images of MRI with a non-enhancing portion on 5-min delayed phase image of MRI. This finding may be necrotic portion rarely seen on lymphoma (89). But, we could not prove it due to lack of radiologic-pathologic correlation. In another case of primary diffuse large B-cell lymphoma of the seminal vesicle, hypermetabolism was noted on FDG PET/CT (5). This finding was consistent with our case.
Two cases of secondary seminal vesicle involvement of diffuse large B-cell lymphoma were reported, in India and Japan (610). The case reported in Japan revealed a homogenous enhancing mass on CT. The mass was of low signal intensity on T1WI and high signal intensity on T2WI, with heterogeneous enhancement (10) - MR findings similar to our case. The case reported in India showed a heterogeneously enhancing mass on CT, and hypermetabolism on FDG PET/CT (6) - findings similar to our case.
As with previously reported cases, our case showed a heterogeneous, hypoechoic mass on TRUS, while CT and MRI demonstrated rim and progressive enhancement with non-enhancing portion with diffusion restriction. FDG PET/CT showed marked hypermetabolism. These findings are suggestive of a nonspecific malignant tumor.
To the best of our knowledge, MR imaging findings in primary diffuse large B-cell lymphoma of the seminal vesicle have not previously been reported. Although there are no specific imaging findings for primary lymphoma, including diffuse large B-cell lymphoma, in the seminal vesicle, we consider lymphoma in the differential diagnosis when confronted with a patient with seminal vesicle tumor.
Figures and Tables
Fig. 1
Primary diffuse large B-cell lymphoma in the seminal vesicle in a 58-year-old man. Transrectal ultrasonography (TRUS) demonstrating a heterogeneous, hypoechoic mass (arrow) in the right seminal vesicle (a). CT images showing a mass with rim-like enhancement (arrows) in the right seminal vesicle on portal venous phase (b, c).

Fig. 2
Primary diffuse large B-cell lymphoma of the seminal vesicle in a 58-year-old man. T2-weighted axial MR image demonstrating a mass with subtle high signal intensity (arrow) in the right seminal vesicle (a); T1-weighted axial image demonstrating a mass of low signal intensity (b, arrow) ; diffusion-weighted imaging showing high intensity (arrow) with a high b-value (1000 s/mm2) (c). The tumor showed rim-like enhancement on 3-min delayed phase image (d, arrow) and progressive with a non-enhancing portion on 5-min delayed phase image (e, arrow). FDG PET/CT revealed a high standardized uptake value (maxSUV, 23.5) in the right seminal vesicle, suggesting a hypermetabolic mass (f, arrow).

Fig. 3
Primary diffuse large B-cell lymphoma of the seminal vesicle in a 58-year-old man. Staining of the biopsy from the seminal vesicle mass showing diffuse proliferation of large neoplastic lymphoid cells (a: × 200, H&E staining). Immunohistochemical staining showing neoplastic cells expressing CD79a, confirming their B-cell lineage (b: × 400).
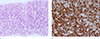
Table 1
Imaging Finding of Primary Diffuse Large B-cell Lymphoma of the Seminal Vesicles in the Previous Reports and Our Case

| Case No. | Authors (Ref. No.) | Year | Sex/Age | TRUS | CT | MR* | PET/CT |
|---|---|---|---|---|---|---|---|
| 1 | Zhu J, et al. (4) | 2011 | M/35 | Heterogeneous echogenic mass | Homogeneous enhancing mass | ||
| 2 | Zhu B, et al. (5) | 2012 | M/63 | Avid FDG uptake | |||
| 3 | Our case | 2016 | M/58 | Heterogeneous hypoechoic mass | Rim-like enhancement |
T1WI: iso SI T2W: intermediate-high SI Rim-like enhancement on 3-min delayed image Progressive enhancement on 5-min delayed image Diffusion restriction |
Avid FDG uptake |
Acknowledgments
No necessary for acknowledgement to colleagues other than co-authors. No related supports or other published materials. No commercial interests to this article.
References
1. Kim B, Kawashima A, Ryu JA, Takahashi N, Hartman RP, King BF Jr. Imaging of the seminal vesicle and vas deferens. Radiographics. 2009; 29:1105–1121.
2. Dalgaard JB, Giertsen JC. Primary carcinoma of the seminal vesicle; case and survey. Acta Pathol Microbiol Scand. 1956; 39:255–267.
3. Benson RC Jr, Clark WR, Farrow GM. Carcinoma of the seminal vesicle. J Urol. 1984; 132:483–485.
4. Zhu J, Chen LR, Zhang X, Gong Y, Xu JH, Zheng S. Primary diffuse large B-cell lymphoma of the seminal vesicles: ultrasonography and computed tomography findings. Urology. 2011; 78:1073–1074.
5. Zhu B, Cai Y, Chen R, Ye C, Tao Y, Wen X. Primary lymphoma of the seminal vesicles presented with acute renal failure: PET-CT findings. Open J Urol. 2012; 2:137.
6. Handa N, Rathinam D, Singh A, Jana M. Seminal vesicle involvement: a rare extranodal manifestation of non-Hodgkin's lymphoma. BMJ Case Rep. 2016; 2016.
7. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972; 29:252–260.
8. Sheth S, Ali S, Fishman E. Imaging of renal lymphoma: patterns of disease with pathologic correlation. Radiographics. 2006; 26:1151–1168.
9. Rajiah P, Sinha R, Cuevas C, Dubinsky TJ, Bush WH Jr, Kolokythas O. Imaging of uncommon retroperitoneal masses. Radiographics. 2011; 31:949–976.
10. Hamada S, Ito K, Kanbara T, et al. A case of malignant lymphoma mimicking a seminal vesicle tumor. Hinyokika Kiyo. 2010; 56:393–396.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download