MATERIALS AND METHODS
Subjects
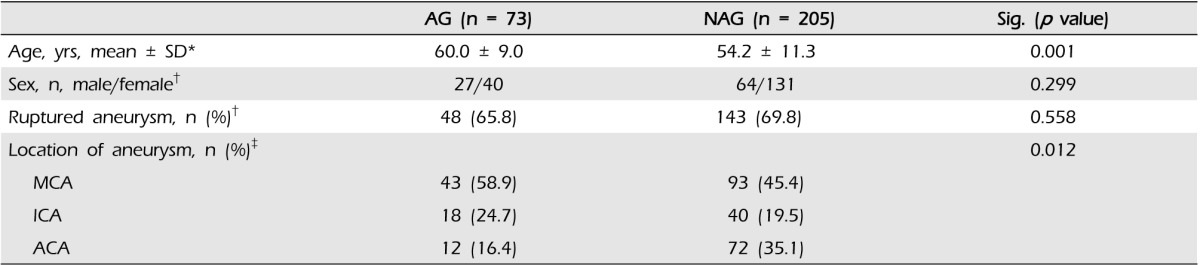
Cases of 262 patients who underwent aneurysmal neck clipping surgery at our center between June 2004 and November 2010 were analyzed retrospectively. We reviewed intraoperative videos; microscopic photographs; pre- and post-operative findings of computed tomography angiogram (CTA), magnetic resonance angiogram (MRA), and digital subtraction angiogram (DSA); and medical and surgical records. We divided the patients into two groups: the atherosclerotic group (AG) with atherosclerotic appearance of vessels, and the non-atherosclerotic group (NAG) without atherosclerosis.
Evaluation of atherosclerotic aneurysm
The criteria for atherosclerotic aneurysm were assessed according to the surgeons' intraoperative findings, either retrospectively or prospectively. Atherosclerotic changes in the vessel or aneurysm walls were identified as follows: (1) yellowish and/or whitish spotty appearance of the vessel and/or aneurysm; (2) surgical confirmation of a definite decrease in elasticity of the wall, with or without a color change of the vessel (
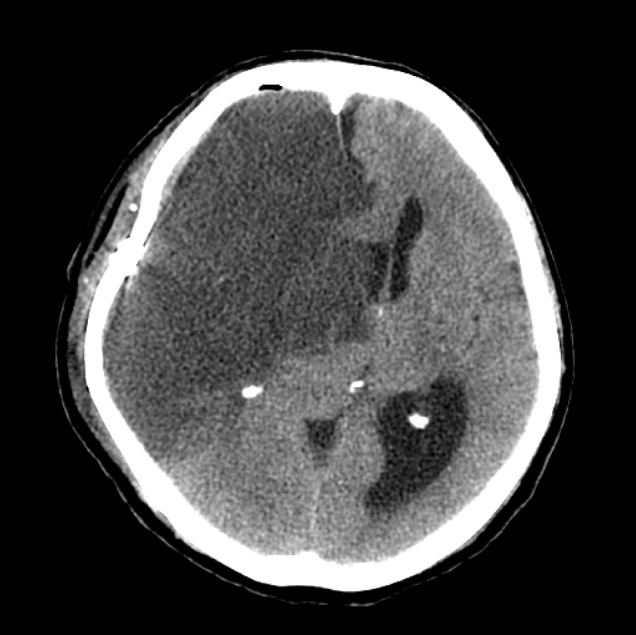
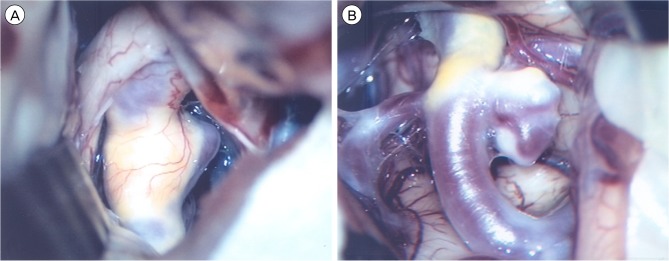
Fig. 1).
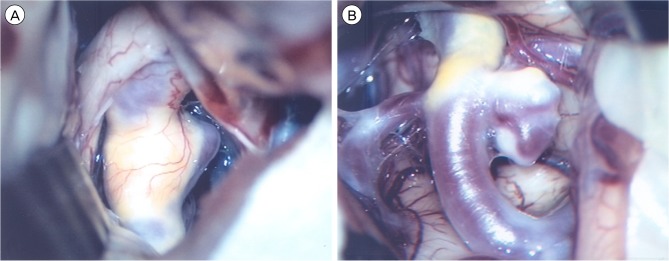 | Fig. 1Operative view of an aneurysm with atherosclerotic wall. (A) Atherosclerotic change in the parent artery and aneurysmal neck. (B) Atherosclerotic change in the parent artery and aneurysmal wall. 
|
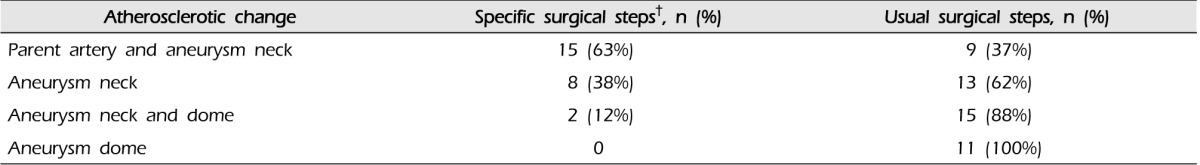
Atherosclerosis types were divided according to the following categories based on the position of the atherosclerotic changes: (1) parent artery and aneurysm neck; (2) aneurysm neck; (3) aneurysm neck and dome; (4) aneurysm dome. Location in the parent artery was defined as atherosclerotic change within 5 mm from the neck of the aneurysm.
Evaluation of surgical result
Clinical outcome was determined according to scoring and changes on the Glasgow outcome scale (GOS). The outcome was determined as favorable if the GOS score was either unchanged, regardless of the preoperative status, or improved to a GOS score of 4-5. An outcome was considered unfavorable if there was deterioration to a GOS score of 1-3. In addition, the occurrence of new postoperative ischemia was assessed with a head computed tomography (CT) scan. The postoperative CT was analyzed for territory infarction or perforator infarction in relation to the clip position.
Statistical analysis
To evaluate the difference between the AG and NAG, the variables of clinical characteristics, aneurysmal characteristics, and surgical procedures between the two groups were compared using univariate methods (the two-sample t-test, Fisher's exact test, and Pearson's Chi-square test). MedCalc® (version 13, MedCalc Software bvba, Ostend, Belgium) was used for analysis, and a p value less than 0.05 was considered statistically significant for all statistics.
Go to :

DISCUSSION
Recently, treatment of cerebral aneurysms has been developing at a rapid pace, and a number of studies have reported good clinical outcomes of aneurysm surgeries. However, Flamm et al. reported that the presence of plaque in an aneurysm can be a predictive factor for unexpected complications during aneurysm surgery.
3) Other researchers have also examined the importance of atherosclerotic aneurysms.
In 1999, Ohno et al. reported atherosclerotic changes in six patients (10%) among 30 patients with cerebral aneurysms.
8) Similarly, in 2003, Grigorian et al. reported atherosclerotic changes in 81 patients (26.7%) among 333 patients with aneurysms.
4) In our study, 67 (25.6%) of the 262 patients with aneurysms had atherosclerotic aneurysms. Therefore, when treating aneurysms, understanding the pathophysiology of atherosclerotic changes is important.
Atherosclerosis is a well-known pathological condition that generally affects the arterial blood vessels. As a degenerative process, atherosclerotic changes result from deposition of plasma lipids, connective tissues, and local or circulating cells over the intima of the blood vessels, which leads to narrowing of the vessel lumen.
7) The restorability of such atherosclerotic vessels is limited because of a resultant decrease in elasticity and increase in rigidity of the vessel.
10) During aneurysm surgery, if the aneurysmal neck has atherosclerotic changes, problems such as incomplete neck clipping and narrowing of the lumen of the parent artery may occur.
8) In particular, narrowing of the lumen of the parent artery may be an important cause of postoperative ischemic events.
Regarding aneurysm location, Szelenyi et al. reported that among patients with atherosclerotic aneurysms, ten had aneurysms in the ICA, five had aneurysms in the anterior communicating artery, and 19 had aneurysms in the MCA.
9) Ohno et al. reported that six patients among seven patients with atherosclerotic changes in the aneurysmal neck had MCA aneurysms.
8) In our study, 43 patients among the 73 patients with atherosclerotic aneurysms had aneurysms in the MCA.
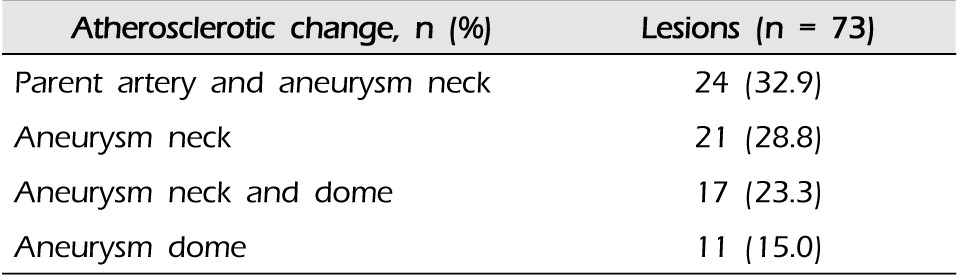
Szelenyi et al. reported that eight cases among 34 atherosclerotic aneurysm cases had atherosclerotic changes in the parent vessel, aneurysm dome, or aneurysm neck, respectively, and 11 cases had changes in both the aneurysm dome and neck.
9) In our study of 73 cases, the sites of atherosclerotic change were as follows: both parent artery and aneurysm neck in 24 (32.9%), aneurysm neck in 21 (28.8%), both aneurysm neck and dome in 17 (23.3%), and aneurysm dome in 11 (15.0%). These findings are not relevant to the findings reported in the papers mentioned earlier.
Regarding the postoperative prognosis of patients with atherosclerotic aneurysms, Szelenyi et al. reported that 27 of 34 atherosclerotic aneurysm patients had a good clinical outcome, increasing to 30 patients at six months. Postoperatively, four patients had an unfavorable outcome, and at the six-month follow-up, only three patients had an unfavorable outcome.
9) In our series, 47 patients had a favorable outcome, 20 patients had an unfavorable outcome, and, unfortunately, one patient expired. The most likely explanation for the higher rate of unfavorable clinical outcomes in our series as compared with that of Szelenyi et al. is that the latter study included only unruptured aneurysms, whereas we included 48 cases of ruptured aneurysms. Reviews of other studies have found that the frequency of morbidity in patients with atherosclerotic aneurysms is higher than in patients with non-atherosclerotic aneurysms, approximately 14% and 6.8%, respectively.
2)3)6)
In atherosclerotic aneurysms, the atherosclerotic wall might increase the occurrence of thromboembolic events, or its rigidity might lead to occlusion of perforators within the aneurysm vicinity during surgery.
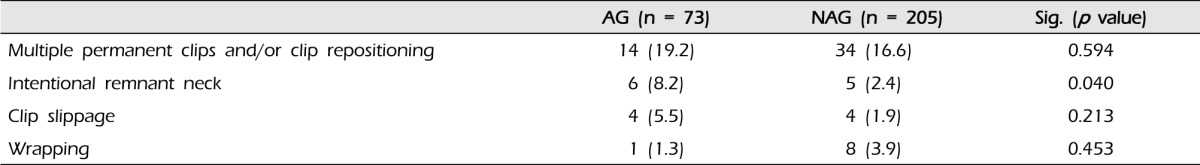
1)5) Szelenyi et al. reported that in six patients with atherosclerotic aneurysms, a small residuum of the aneurysm neck was intentionally left. This was done significantly more often than in patients with non-atherosclerotic aneurysms. In addition, in patients with atherosclerotic aneurysms, temporary vessel occlusion and multiple repositioning of the permanent clip were performed more often than in patients with non-athe rosclerotic aneurysms. Although the application of more than one permanent clip and wrapping occurred more often in patients with atherosclerotic aneurysms, this did not reach statistical significance in their study.
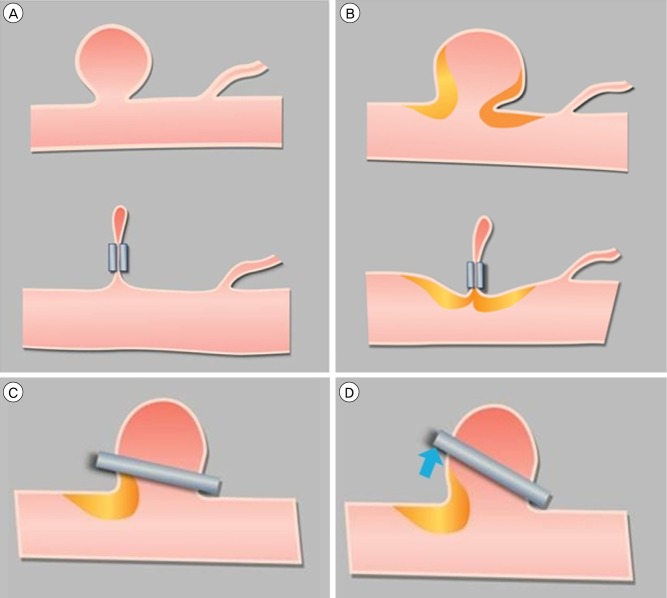
9) It is expected that clip placement in atherosclerotic aneurysms requires more surgical steps compared with non-atherosclerotic aneurysms. This is supported by our finding that the intraoperative observation of atherosclerosis showed significant correlation with a higher percentage of multiple positioning of a permanent clip. Clip placement might be hampered by a rigid atherosclerotic wall such that aneurysm obliteration due to sliding of the clip off the aneurysm dome is not complete or that the parent vessel or perforating branches are occluded (
Fig. 3). One solution to this problem is aneurysm obliteration with multiple clips.
8)9) Furthermore, as in our study, avoidance of the region of the atheroma could promote effective clip placement and prevent parent artery occlusion.
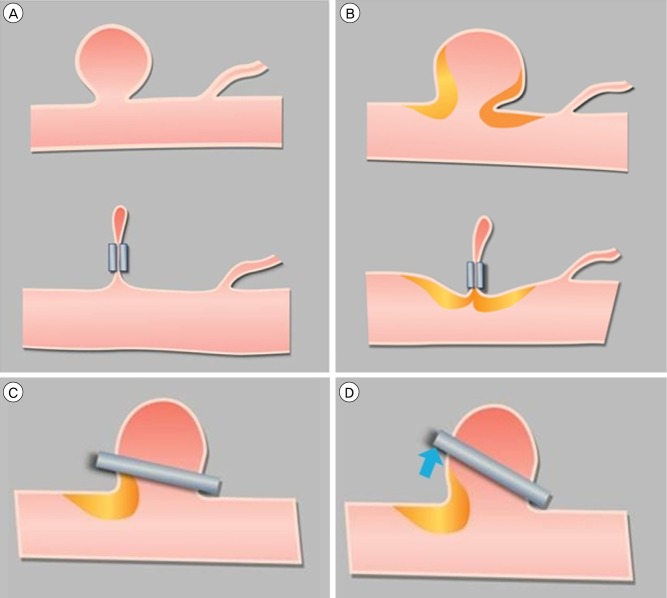 | Fig. 3Schematic illustrations of cerebral aneurysms. (A) Non-atherosclerotic aneurysm prior to neck clip placement (above) and with neck clip in place (below). (B) Parent artery narrowing due to atheroma, with and without neck clip in place. (C) and (D) Atherosclerotic change in the aneurysm neck leads to sliding of the clip and results in a remnant neck after clipping. 
|
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download