Abstract
Purpose
Insufficient knowledge of the anatomy of the maxillary sinuses prior to sinus graft surgery may lead to perioperative or postoperative complications. This study sought to characterize the position of the posterior superior alveolar artery (PSAA) within the maxillary sinuses using cone-beam computed tomography (CBCT).
Materials and Methods
A total of 300 patients with edentulous posterior maxillae, including 138 females and 162 males with an age range of 33-86 years, who presented to a radiology clinic between 2013 and 2015 were enrolled in this retrospective cross-sectional study. The distance from the inferior border of the PSAA to the alveolar crest according to the residual ridge classification by Lekholm and Zarb, the distance from the PSAA to the nasal septum and zygomatic arch, and the diameter and position of the PSAA were all assessed on patients' CBCT scans. The data were analyzed using the Mann-Whitney test and the t-test.
Results
The PSAA was detected on the CBCT scans of 87% of the patients; it was located beneath the sinus membrane in 47% of cases and was intraosseous in 47% of cases. The diameter of the artery was between 1 and 2 mm in most patients (72%). The mean diameter of the artery was 1.29±0.39 mm, and the mean distances from the PSAA to the zygomatic arch, nasal septum, and alveolar crest were 22.59±4.89 mm, 26.51±3.52 mm, and 16.7±3.96 mm, respectively.
Inadequate bone volume due to alveolar bone resorption is often associated with pneumatization of the maxillary sinus, causing clinical problems for implant placement in the posterior maxilla.1 Successful implant placement in the posterior maxilla in such cases requires the bone height to be increased via alveolar bone augmentation, which is often performed by maxillary sinus floor augmentation. Augmentation of the maxillary sinus floor using autogenous bone was first described by Boyne and James in 1980 for implant placement.2 It still remains a safe and predictable surgical procedure for augmentation of the alveolar ridge in atrophic posterior maxillae.3 However, sufficient knowledge about sinus anatomy and its vascular supply, as well as a thorough preoperative assessment, are key factors in the success of this treatment modality.
The infraorbital artery and the posterior superior alveolar artery (PSAA) are the branches of the maxillary artery that provide blood supply to the lateral sinus walls and the sinus floor membrane.4 To avoid traumatizing these arteries and subsequent perioperative bleeding, locating their exact position is imperative prior to sinus floor augmentation surgery.5 The use of a 3-dimensional imaging technique to visualize the anatomy of the maxillary sinus can be very helpful in this respect.6 Several factors can affect the selection of the radiographic technique for each patient. These factors include cost, availability, patient radiation dose, and case type.1
Cone-beam computed tomography (CBCT) was introduced to dentistry in the late 1990s. It is a digital imaging modality that provides accurate information about the morphology of bone and the location of anatomical landmarks such as the PSAA.78 A lower patient radiation dose is a major advantage of CBCT over computed tomography (CT).9
Several studies have assessed the anatomy of the maxillary sinuses using panoramic radiography and 3-dimensional radiographic modalities such as CT and CBCT. However, considering the clinical significance of this topic, the lack of adequate information in this regard, and the controversial results of previous studies on the exact position of the PSAA in the Iranian population, this study sought to assess the prevalence and location of the PSAA and its relation to the alveolar ridge, nasal septum, and zygomatic arch.
This retrospective cross-sectional study was conducted in the Periodontology Department of Shahed University during 2014 and 2015. The study protocol was approved by the Ethics Committee of Shahed University.
The CBCT scans used in this study were obtained using a NewTom VG apparatus (QR srl, Verona, Italy), set at a tube voltage of 110 kVp and a tube current of 13.11 to 20.18 mA. In our study group, we performed 2 types of scans: one a with 0.3-mm voxel size for a larger field of view (160×110 mm) and the other with a 0.24-mm voxel size for a smaller field of view (120×70 mm). The axial thickness was either 0.24 mm or 0.3 mm (isotropic voxel reconstruction). The slice thickness of the multiplanar reconstruction images was 1 mm.
A total of 300 CBCT scans of 138 females and 162 males between 33 and 86 years of age, who had presented to the radiology clinic of our institution between 2013 and 2015, were randomly selected. The inclusion criteria were: 1) the availability of CBCT scans of the posterior maxilla with maxillary molar and premolar teeth missing in at least one quadrant, 2) visibility on the CBCT scans of up to 2 cm above the maxillary sinus roof, and 3) the absence of motion or scattering artifacts.
Images showing changes in the morphology of the sinus walls due to trauma or pathological conditions were excluded from the study. The posterior superior alveolar canal along the posterolateral wall of the maxillary sinus was assessed on the coronal sections using NNT Workstation version 4.5 software (QR srl, Verona, Italy) and the data were recorded in charts for each patient.
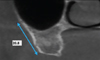
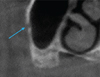
The PSAA was assessed in terms of the following factors: 1) Distance from the inferior border of PSAA to the alveolar crest: the closest distance to the edentulous ridge was measured (Fig. 1). 2) Diameter of the PSAA: since the artery was visible in more than one area and considering the importance of the diameter of the artery in the occurrence of perioperative bleeding, the greatest diameter of the PSAA was measured. According to the PSAA diameter, 3 groups were defined: <1 mm, 1-2 mm, and >2 mm. 3) Position of the PSAA: according to a study by Ilgüy et al. in 2013,6 the PSAA was divided into 3 categories in terms of its position: (1) intraosseous (Fig. 2), (2) beneath the membrane (Fig. 3), and (3) over the external cortex of the lateral sinus wall (Fig. 4). The software used in the current study had high accuracy and enabled the classification of PSAA into the abovementioned 3 groups. 4) Distance from the PSAA to the zygomatic arch (Fig. 5): considering the extent of the zygomatic arch, the most anterior and inferior point of the zygomatic arch was marked first, and then the closest distance from this point to the PSAA was measured using the 3-dimensional distance measurement feature of the CBCT software. 5) Distance from the PSAA to the nasal septum (Fig. 5): the closest distance from the PSAA to the nasal septum was measured. Considering the variable diameter of the nasal septum in different areas, its thickness at the center was used as a reference. 6) Determination of the type of residual alveolar ridge: the type of edentulous ridge was classified according to the classification by Lekholm and Zarb in 198510 based on the amount of resorption.
The CBCT scans were evaluated by a dentist trained by an oral and maxillofacial radiologist for this purpose. To determine the reliability and reproducibility of the findings (intrarater agreement), the CBCT scans were evaluated again by the same observer 2 weeks later.
The data were analyzed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics (mean, variance, standard deviation, and range) were calculated for the variables. The t-test was used to compare the mean values of quantitative variables between males and females and also for the comparison of relative measurements. The non-parametric Mann-Whitney test was applied to compare the mean values of qualitative variables between the 2 groups. The level of significance was set at P<.05.
The mean age of the patients was 62.4±10.6 years. The PSAA was detected in the CBCT scans of 87% of the patients; it was located beneath the membrane in 47% of patients, while it was intraosseous in 47% of patients. The PSAA was located on the external cortex of the lateral sinus wall in 6% of the patients.
The diameter of PSAA was 1-2 mm in most patients (74.8%), >2 mm in 4.5%, and <1 mm in 20.7%. The results of the parametric t-test revealed a significant difference in the diameter of the PSAA between males and females (P<.05). The mean diameter of the PSAA was 1.38±0.35 mm in males and 1.2±0.37 mm in females.
The results of the non-parametric Mann-Whitney test showed a significant difference in the position of the PSAA between males and females (P<.05). The position of the PSAA was intraosseous in 47.9% of males, while it was beneath the membrane in 48% of females (Table 1).
A significant difference was noted in the prevalence of the PSAA between patients with complete and partial edentulism, and the likelihood of not detecting the PSAA on the CBCT scans of patients with complete edentulism was higher (25.7%) than for patients with partial edentulism (6.1%); this difference was statistically significant (P<.05, Table 1).
The mean distance from the PSAA to the zygomatic arch was 25.59±4.89 mm, and the difference in this respect between males and females was not significant (P>.05). The mean distance from the inferior border of PSAA to the alveolar crest was 16.7±3.96 mm, and the difference in this respect between males and females was statistically significant (P<.05).
The mean distance from the PSAA to the nasal septum was 26.51±3.52 mm, and a significant difference existed in this respect between males and females (P<.05, Table 2).
According to Lekholm and Zarb's classification, most patients had type C ridges (53%), followed by type D (33.5%). Based on the type of residual ridge, the distance from the inferior border of the PSAA to the alveolar crest was measured, and it was found that smaller edentulous ridges were associated with lower values of this distance (Table 3).
Maxillary sinus floor augmentation is a highly predictable method for the successful placement of dental implants in atrophic posterior maxillae.3 Knowledge of the anatomy of the region is especially important for the success of this treatment modality. In the current study, we assessed the prevalence and position of PSAA using CBCT scans. The PSAA was detected on the CBCT scans of 87% of the patients, which is similar to the prevalence reported by Ilgüy et al. (89.3%).6 The prevalence of PSAA in the current study was higher than that reported by Elian et al. (52.9%)11 and Mardinger et al. (55%)12; this difference may be due to differences in the methodology of these studies and the sample size and definitions of the PSAA on images, because Solar et al.4 and Rosano et al.13 demonstrated that an endosseous anastomosis of the PSAA and infraorbital artery was present in 100% of cadaveric specimens. This finding indicates that not detecting the PSAA on CBCT or CT scans does not necessarily mean that it is absent. It may not be visible due to its small diameter.12
In the current study, the PSAA was present beneath the membrane as often as it had an intraosseous location (47%), but in a small percentage of patients, the PSAA was detected on the external cortex of the lateral sinus wall (6%). The frequency of the presence of the PSAA on the external cortex was 5.7% in a study by Güncü et al.,14 and 5.2% in a study by Ilgüy et al.6; these values are close to our obtained value.
No significant difference between males and females in the prevalence of PSAA was found in our study, which is in agreement with the results of Ilgüy et al.6 However, Kim et al.15 reported a higher prevalence in males (64%). The difference between their results and ours may be due to differences in the male-to-female ratio.
In the current study, the position of the PSAA significantly varied in males and females. The same finding was reported by Kim et al.16 However, this difference was not significant in the study by Ilgüy et al.6 This discrepancy may likewise be attributed to differences in the male-to-female ratio.
In our study, the PSAA had a moderate diameter (1-2 mm) in most patients (72%); this finding accords with the results of Güncü et al. (1.3 mm)14 and Ella et al. (1.2 mm).5 In the study by Ilgüy et al.,6 the diameter of the PSAA was <1 mm in most cases (68.9%). In the study by Mardinger et al.,12 the number of patients with a PSAA diameter <1 mm and between 1 and 2 mm was the same. This variability in the results may be attributed to racial differences in the study populations. In the current study, the diameter of the PSAA in males was greater than in females (P<.05), which is in accordance with the results of Güncü et al.14
Our study showed that the PSAA was not detected in a higher percentage of completely edentulous patients than partially edentulous subjects (25.7% versus 6.1%). Monje et al.17 concluded that the mean lateral wall thickness was smaller in fully edentulous patients than in partially edentulous subjects. Sinus pneumatization and a reduction in lateral sinus wall thickness often occur in patients with complete edentulism. Thus, it is assumed that the impression of the PSAA canal on the lateral sinus wall is less visible in these patients due to the reduced thickness of the sinus wall.
To determine the position of the PSAA and its distance from the zygomatic arch, the distance from the inferior border of the PSAA to the alveolar crest and the distance from the PSAA to the nasal septum were measured. The mean distance from the PSAA to the zygomatic arch was 25.59±4.89 mm; the difference in this respect between males and females was not significant. The mean distance from the PSAA to the nasal septum was 26.51±3.52 mm; the difference in this respect between males and females was statistically significant. To the best of our knowledge, no previous study has evaluated the distance from the PSAA to the zygomatic arch or to the nasal septum. By using these anatomical landmarks and measurements, the approximate location of the PSAA can be estimated prior to surgery when CBCT may not be available. Consequently, damage to the PSAA and subsequent complications can be prevented.
The mean distance from the inferior border of the PSAA to the alveolar crest was 16.7±3.96 mm, which is close to the values reported in other studies. This distance was reported to be 17 mm by Ilgüy et al.,6 18±4.9 mm by Güncü et al.,14 16.4 mm by Elian et al.,11 16.9 mm by Mardinger et al.,12 and 18.9 mm by Kim et al.16 The variability in the results may be explained by differences in the vertical height of the alveolar ridge among individuals.
During the preparation of the lateral window in the lateral sinus wall, there is a high risk of injury to the PSAA. The height of the residual alveolar ridge is an important factor determining the approximate position of the PSAA.
In groups A and B according to the classification proposed by Lekholm and Zarb, the distance from the PSAA to the alveolar crest is more than 16 mm. In groups C and D, the distance from the PSAA to the alveolar crest is more than 10 mm. In group E, the ridge is severely atrophic; thus, this distance is often less than 10 mm. The results of Mardinger et al.12 are similar to our findings in this respect. With the reduction in size of the residual alveolar ridge from class A to E, the distance from the PSAA to the alveolar crest decreased as well. Thus, it is recommended that the superior border of the osteotomy in classes A to C should be placed 15-16 mm above the alveolar bone crest to prevent trauma to the PSAA. In ridges with more severe resorption, as in classes D and E, care must be taken not to damage the PSAA.
In conclusion, the likelihood of detecting the PSAA on CBCT scans is high. Its location is intraosseous or beneath the sinus membrane in most patients, with a mean distance of 16.7±3.96 mm to the alveolar crest. Thus, in surgical procedures on severely resorbed ridges, determining the exact location of the PSAA on CBCT scans preoperatively can help prevent it from being damaged during surgery.
Figures and Tables
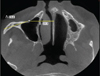
Fig. 3
Coronal view of the maxillary sinus, showing the artery (arrow), which is below the membrane.
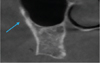
Fig. 4
Coronal view of the maxillary sinus, showing the artery (arrow), which runs over the external cortex of the lateral sinus wall.
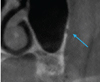
Table 3
Assessment of the type of residual ridge according to the classification of Lekholm and Zarb10

References
1. Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's clinical periodontology. 12th ed. St. Louis, MO: Saunders;2015.
2. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–616.
3. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008; 35:8 Suppl. 216–240.

4. Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999; 10:34–44.

5. Ella B, Sedarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, et al. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008; 23:1047–1052.
6. Ilgüy D, Ilgüy M, Dolekoglu S, Fisekcioglu E. Evaluation of the posterior superior alveolar artery and the maxillary sinus with CBCT. Braz Oral Res. 2013; 27:431–437.
7. Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999; 28:245–248.

8. Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998; 8:1558–1564.

9. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:106–114.

10. Lekholm U, Zarb GA. Patient selection and preparation. In : Brånemark PI, George AZ, Albrektsson T, editors. Tissue-integrated prostheses: osseointegration in clinical dentistry. Chicago, IL: Quintessence;1985. p. 199–209.
11. Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005; 20:784–787.
12. Mardinger O, Abba M, Hirshberg A, Schwartz-Arad D. Prevalence, diameter and course of the maxillary intraosseous vascular canal with relation to sinus augmentation procedure: a radiographic study. Int J Oral Maxillofac Surg. 2007; 36:735–738.

13. Rosano G, Taschieri S, Gaudy JF, Del Fabbro M. Maxillary sinus vascularization: a cadaveric study. J Craniofac Surg. 2009; 20:940–943.
14. Güncü GN, Yildirim YD, Wang HL, Tözüm TF. Location of posterior superior alveolar artery and evaluation of maxillary sinus anatomy with computerized tomography: a clinical study. Clin Oral Implants Res. 2011; 22:1164–1167.

15. Kim JH, Ryu JS, Kim KD, Hwang SH, Moon HS. A radiographic study of the posterior superior alveolar artery. Implant Dent. 2011; 20:306–310.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download