Abstract
Purpose
This study compared the diagnostic accuracy of cone-beam computed tomography (CBCT) scans obtained with 2 CBCT systems with high- and low-resolution modes for the detection of root perforations in endodontically treated mandibular molars.
Materials and Methods
The root canals of 72 mandibular molars were cleaned and shaped. Perforations measuring 0.2, 0.3, and 0.4 mm in diameter were created at the furcation area of 48 roots, simulating strip perforations, or on the external surfaces of 48 roots, simulating root perforations. Forty-eight roots remained intact (control group). The roots were filled using gutta-percha (Gapadent, Tianjin, China) and AH26 sealer (Dentsply Maillefer, Ballaigues, Switzerland). The CBCT scans were obtained using the NewTom 3G (QR srl, Verona, Italy) and Cranex 3D (Soredex, Helsinki, Finland) CBCT systems in high- and low-resolution modes, and were evaluated by 2 observers. The chi-square test was used to assess the nominal variables.
Results
In strip perforations, the accuracies of low- and high-resolution modes were 75% and 83% for NewTom 3G and 67% and 69% for Cranex 3D. In root perforations, the accuracies of low- and high-resolution modes were 79% and 83% for NewTom 3G and was 56% and 73% for Cranex 3D.
Conclusion
The accuracy of the 2 CBCT systems was different for the detection of strip and root perforations. The Cranex 3D had non-significantly higher accuracy than the NewTom 3G. In both scanners, the high-resolution mode yielded significantly higher accuracy than the low-resolution mode. The diagnostic accuracy of CBCT scans was not affected by the perforation diameter.
Root perforation is defined as a pathological mechanical communication between the root canal and the periodontal tissue supporting the tooth.1 Root perforation most often occurs due to operator error, and can happen at any step during root canal treatment. When root perforation occurs, it compromises the periradicular tissue, and if it is not treated or if treatment is delayed, tooth extraction may be necessary. Root perforation occurs in 2%–12% of endodontically treated teeth.2 Evidence shows that the process of healing takes place 31% more slowly in teeth with root perforation than in teeth without root perforation.3
Several factors, such as the time of diagnosis and treatment, as well as the size and location of the perforation, affect the prognosis of treatment.13 The time interval between diagnosis and treatment and the site of perforation are the most important factors determining the prognosis. Prompt diagnosis and treatment decrease the risk of infection of the perforated site and often result in an optimal response by the periradicular tissue. Thus, immediate aseptic treatment techniques are associated with high rates of success.1
In addition to clinical signs and symptoms, several devices and methods have been suggested for the clinical detection of root perforations, such as electronic apex locators, surgical microscopes, endoscopes, and optical coherence tomography scans; however, none of these devices can detect perforations in endodontically treated teeth (filled roots).14
Radiographs provide beneficial information for the diagnosis, treatment, and follow-up of endodontically treated teeth.5 The main limitations of intraoral radiographs include 2-dimensional imaging of a 3-dimensional object and the superimposition of anatomical structures and cortical bone covering the area; these factors complicate the accurate visualization of the perforation site and make it difficult to estimate its extent. This limitation has been overcome by the use of 3-dimensional computed tomography and cone-beam computed tomography (CBCT).67
CBCT is a type of computed tomography, in which a cone-shaped beam is used. It provides several advantages for the diagnosis and treatment planning of endodontic problems.8 CBCT systems vary in terms of the detector type and resolution, which can affect the diagnostic accuracy and diagnostic value of these systems.9 New CBCT scanners vary in terms of some major exposure settings, such as amperage, voltage, exposure time, and field of view (FOV). These variations not only affect the patient's radiation dose, but also impact the diagnostic quality of the images.10 Moreover, some CBCT scanners allow the selection of a high- or low-resolution mode for scanning. The images obtained in each of these modes are captured with different voxel sizes, and switching from the high-resolution mode to the low-resolution mode and vice versa therefore necessitates changing the voxel size and amperage.1011 Spatial resolution, defined as the ability to detect small details on images, depends on voxel size in digital systems. A smaller voxel size yields higher spatial resolution.10 Voxel size is a critical factor affecting the quality and time of CBCT image reconstruction. Voxels in CBCT systems are isotropic and range from 0.8 mm×0.8 mm×0.8 mm to 4 mm×4 mm×4 mm.9 Theoretically, higher spatial resolution enables better visualization of details on images. However, higher resolution results in a higher radiation dose for the patient.10 The most effective dose significantly depends on the scanning protocol. Any protocol includes a combination of voltage, amperage, voxel size, and some other factors; thus, in reality, the effective dose closely depends on the selected exposure settings.12 FOV also plays a pivotal role in evaluating the effective dose in CBCT. If exposure settings such as voltage and amperage are kept constant, a larger FOV is associated with a higher effective dose.12 The considerations suggest that higher spatial resolution increases the effective dose, as has also been reported by Davies et al.13
Despite the existence of different tools and methods to detect root perforation, radiography is the only diagnostic modality for endodontically treated teeth, which have filled canals.
It is not known whether high resolution (resulting in a higher radiation dose for the patient) increases the diagnostic accuracy of CBCT for detecting root perforations. No definitive information is available on the effect of voxel size in CBCT on the detection of various sizes of root perforations in different areas in endodontically treated teeth. Thus, this study sought to assess the effect of the resolution mode of CBCT and the type of CBCT system on diagnostic accuracy in detecting root perforations.
A total of 72 first and second mandibular molars were selected and clinically evaluated under a magnifying glass to ensure the absence of root defects. The teeth were stored in distilled water until the experiment.
For the endodontic treatment of the teeth, an access cavity was prepared, the coronal pulp was excavated, and the root canals were cleaned and shaped using K-files #15-35 (Mani Inc., Utsunomiya, Japan) via the step-back technique. To accomplish cleaning and shaping, #35 and #40 ProTaper rotary files (Dentsply Maillefer, Ballaigues, Switzerland) were also used according to the manufacturer's instructions. Each root canal was rinsed with 2% sodium hypochlorite (Rafooneh, Arak, Iran) using a 27-gauge needle. Each canal was then rinsed with 2 mL of distilled water (Fig. 1).
For root perforation, the 144 roots were divided into 3 groups (n=48). In group 1, no perforations were made (control group). The remaining 96 roots were divided into 2 groups based on the site of perforation: strip perforations (cervical perforations) and root perforations (middle and apical perforations). Next, in each group, perforations with diameters of 0.2, 0.3, and 0.4 mm were created (to simulate clinical circumstances) in equal numbers in the mesiolingual canal of the mesial roots and the distal canal of the distal roots.
To create root perforations in the apical and middle thirds, the root canal wall was excessively filed at the curvature area using #15–40 K-files (Mani Inc., Utsunomiya, Japan). Next, depending on the diameter of the perforation, the perforated area was dilated by passing #20, #30, or #40 files through the perforation until easy passage of the files was achieved. Perforations at the cervical area (strip perforations) were made using #1–3 Gates Glidden drills (Mani Inc., Utsunomiya, Japan) down to 3 mm below the furcation area. Considering the possibility of presence of 2 perforations in each tooth and that the perforation sites had to be embedded in alveolar sockets in dry mandibles, the tooth crowns were color-coded based on the type of perforation (Fig. 2).
The root canals were dried with #30 and #35 paper points (Ariadent, Tehran, Iran). Next, the tip of the thickest guttapercha cone (Gapadent, Tianjin, China) that reached the working length was dipped in AH26 sealer (Dentsply Maillefer, Ballaigues, Switzerland) and inserted into the canal. Root canals were filled using #20 and #25 accessory gutta-percha cones and #25–#35 spreaders (Mani Inc., Utsunomiya, Japan) via the lateral compaction technique.
After cutting the cones at the orifice, the root filling was condensed to eliminate voids, and the gutta-percha and sealer residues were cleaned with a cotton pellet dipped in alcohol. The teeth were then mounted in a dry human mandible. Two layers of red wax were used to cover the bone surfaces to simulate soft tissue. The teeth were fixed in alveolar sockets using universal red wax (Associated Dental Products Ltd Kemdent, Swindon, UK) with 2-mm thickness and universal sticky wax (Associated Dental Products Ltd Kemdent, Swindon, UK).
To obtain CBCT scans using the NewTom 3G system (QR srl, Verona, Italy), the dry mandible was placed in a plastic container containing water and positioned in a manner similar to that used in clinical settings. CBCT scans were obtained with 110 kVp, 0.61 mA, 3.6 s, a 6-inch FOV, and a voxel size of 180 µm in the high-resolution mode and 110 kVp, 0.61 mA, 3.6 s, a 6-inch FOV, and a voxel size of 210 µm in the low-resolution mode. The initial image reconstruction was done using axial sections with 0.2-mm thickness, and the reconstruction image was stored (Fig. 3).
The imaging procedure using the CBCT Cranex 3D system (Soredex, Helsinki, Finland) was similar to that used with the NewTom 3G. However, since imaging had to be done in the standing position, the mandible was positioned similarly to how the chin is placed in a chin rest in an area compatible with the radiation field of the Cranex 3D system in high- and low-resolution modes with exposure settings of 90 kVp, 4 mA, 12.6 s, a voxel size of 0.2 mm, a FOV of 8×6 cm, and 0.2 mm slice thickness (Fig. 4). After data reconstruction at 0.2 mm intervals, the files were stored. Images were evaluated in the coronal, axial, and sagittal planes (Fig. 5). Images were interpreted by 2 oral and maxillofacial radiologists with 23 and 5 years of clinical experience, respectively, who were experts in the interpretation of CBCT scans. Any interruption in the continuity of the external root surface was diagnosed as a root perforation. Any interruption in the continuity of the external root surface at the furcation site was diagnosed as a strip perforation. Two observers (dentomaxillofacial radiologists) not involved in the study received instructions to separately and randomly observe the images and grade their observations as ‘presence of perforation,’ ‘absence of perforation,’ or ‘probable perforation’ (questionable cases where a perforation could not be clearly detected). The Cranex 3D and NewTom 3G CBCT images were observed in the axial, coronal and sagittal planes on a 15-inch liquid crystal display monitor (Satellite L55 TB5271; Toshiba, Tokyo, Japan) with a resolution of 1366×768 pixels in a dimly lit room. No time restriction was set. Observers could adjust the brightness, contrast, and magnification of images.
The sensitivity and specificity of each imaging modality were calculated and reported as percentages by dividing the number of correct diagnoses of perforations (definite perforations and questionable cases) by the total number of perforated roots, and the number of non-perforated roots correctly diagnosed by the total number of non-perforated cases, respectively. Knowledge of the presence/absence of perforations served as the gold standard. The chi-square test was used to compare quantitative values. Statistical analyses were carried out using STATA version 11.2 (STATA Corp. LLC, College Station, TX, USA) with 95% confidence intervals. To assess inter-observer agreement, the kappa coefficient was calculated for each imaging technique. Kappa coefficient values >0.75 were considered to show excellent agreement, values of 0.40–0.75 indicated moderate to good agreement, and values <0.40 corresponded to poor agreement.
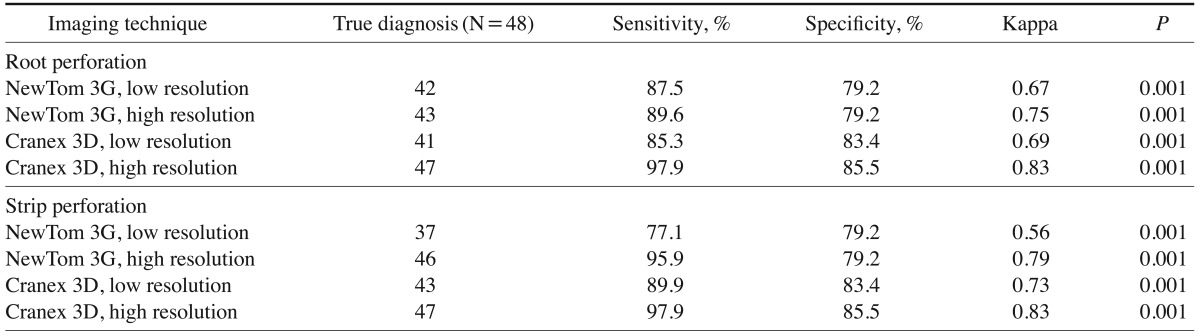
Table 1 shows the diagnostic accuracy, sensitivity, and specificity of the first and second observers for the detection of root perforations on CBCT scans taken in highand low-resolution modes with the Cranex 3D and NewTom 3G systems.
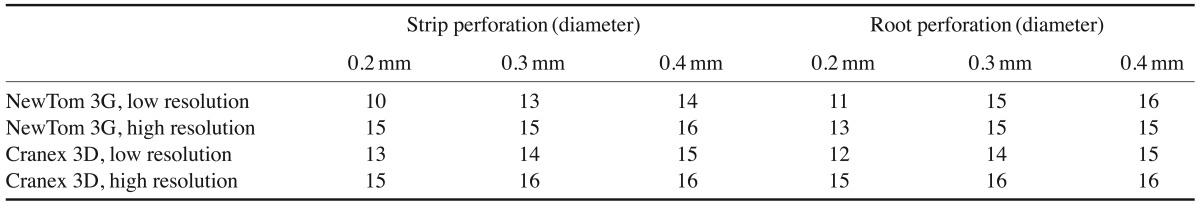
The comparison of the diagnostic accuracy of CBCT based on the resolution mode of the systems showed that the high-resolution mode had higher diagnostic accuracy than the low-resolution mode. This difference was significant for both the NewTom 3G and Cranex 3D systems (P<.05). No significant difference was noted between the NewTom 3G and Cranex 3D systems for the detection of root perforations (Table 2).
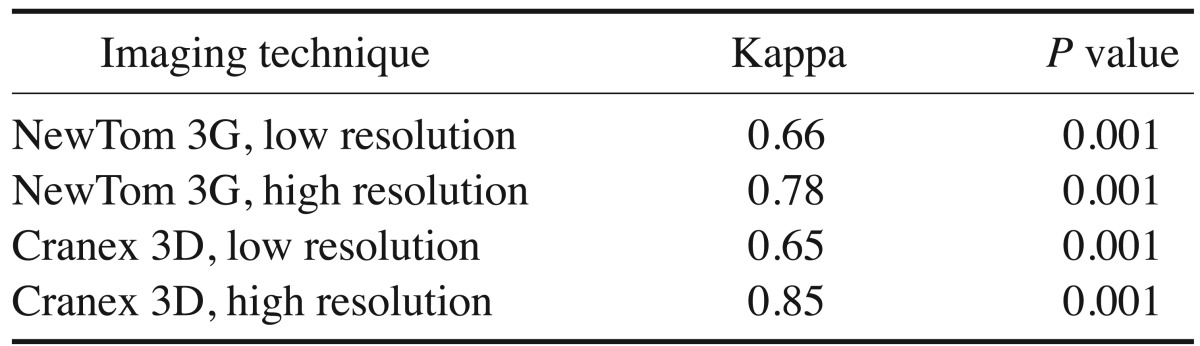
A comparison of the sensitivity and specificity of these 2 radiographic systems for the detection of root perforations in high- and low-resolution modes showed that despite the higher sensitivity of high-resolution CBCT scans, significant differences only existed between the Cranex high-resolution mode and the Cranex low-resolution mode (P=.027), while the difference between the NewTom high-resolution and NewTom low-resolution modes was not significant (P=.749). Additionally, despite the higher diagnostic accuracy of the NewTom high-resolution mode, the difference between the Cranex high-resolution and NewTom high-resolution modes was not significant (P=.094).
In the detection of strip perforations in high- and low-resolution modes, despite the higher sensitivity of the high-resolution modes, a significant difference in the detection of root perforations was only found between the NewTom high-resolution mode and the NewTom low-resolution mode (P=.007). No significant difference was noted between the Cranex high-resolution and Cranex low-resolution modes (P=.092). Additionally, despite the higher diagnostic accuracy of the NewTom high-resolution mode, the difference between the Cranex high-resolution and NewTom high-resolution modes was not significant (P=.557, Table 3).
This study aimed to assess the diagnostic accuracy of CBCT for the detection of root perforations in endodontically treated mandibular molars in high- and low-resolution modes. We also assessed the effects of the perforation site and diameter on the diagnostic accuracy of the imaging systems. We created perforations in 3 different diameters resembling the diameters of 3 endodontic file tips. Perforations were created on the mesial and distal root surfaces because perforations more commonly occur in these surfaces due to the morphology of mandibular molars.14
Due to its 3-dimensional nature and the fact that it eliminates superimpositions, CBCT has the potential to detect root perforations more accurately than other imaging modalities. However, various CBCT systems have major differences in terms of their ability to detect root perforations. CBCT systems also have differences in diagnostic values regarding the detection of root perforations. CBCT systems have different resolutions and contrasts based on the type of detector, the size of the FOV, the voxel size, the number and extent of artifacts, the number of basic images, and the image reconstruction algorithm.915 In this study, we compared the NewTom 3G and Cranex 3D CBCT systems.
A comparison of the diagnostic value of the NewTom 3G and Cranex 3D CBCT systems with different resolutions showed that the Cranex 3D high-resolution mode had higher sensitivity than the NewTom high-resolution mode, although this difference was not statistically significant. This non-significant difference in sensitivity may have been due to the type of the detector and the resolution of the images, or differences in the interpretation of images by the observers. CBCT systems are divided into 2 groups based on the type of detector: image intensifier tube/charge coupled devices (IIT/CCD) and flat-panel detectors (FPDs). FPDs have higher contrast and spatial resolution than IIT/CCDs. Moreover, artifacts and pixel noise are higher in IIT/CCDs. However, the main advantage of IIT/CCDs is that they involve a significantly lower radiation dose to the patient.1016 The NewTom 3G CBCT system has IIT/CCD detectors, while the Cranex 3D has FPDs; this may explain the higher diagnostic value of the Cranex 3D system than the NewTom 3G system for the detection of root perforations. However, based on our results, the high-resolution images of both the NewTom 3G and Cranex 3D systems were superior to the corresponding low-resolution images, and the differences between the NewTom high resolution and NewTom low resolution modes and between the Cranex high-resolution and Cranex low-resolution modes were statistically significant. Moreover, for the detection of strip perforations, the difference between the NewTom high-resolution and NewTom low-resolution modes was significant; but the difference between the 2 modes for root perforation was not significant, which may have been due to differences in the proficiency and experience of the observers. Dalili et al.17 evaluated the effect of the resolution of the CBCT system on the detection of small external root resorption defects (depth, 0.25 mm; diameter, 0.5 mm) and showed that the high-resolution mode was preferable for detecting small defects. Venskutonis et al.11 evaluated the effects of different voxel sizes on the detection of root perforations in non-endodontically treated teeth and showed that by decreasing the voxel size and increasing the resolution, the diagnostic value for the detection of root perforation increased, which agrees with our results. However, the utility of high-resolution images depends on the value of the diagnostic information obtained, which should be weighed against the high radiation dose administered to the patient. In clinical situations, other factors, such as the performance and expertise of the observer, the environment and conditions in which the images are viewed, patient-related factors, and CBCT software specifications, also affect the detection of perforations.11 In our study, artificial perforations were created and the teeth were inserted into alveolar sockets; soft tissue was also simulated with wax. However, clinical conditions cannot be perfectly simulated in such a setup. Artificially created defects are more easily detectable. Also, patient movements during scanning do not occur in in vitro settings. Moreover, there are some inherent differences between in vitro and in vivo studies, which increase the risk of bias and overestimation in the studies.918 In a previous study, the sensitivity and specificity of CBCT for detecting perforations in patients with internal root resorption were 81.3% and 84.4%, respectively.19
The site of a root perforation significantly affects the outcome of treatment. Perforations in the cervical area close to the alveolar crest have a poor prognosis due to high salivary contamination and the migration of epithelial attachments to the perforation site, with subsequent periodontal pocket formation, while apical perforations often have a good prognosis if they can be efficiently sealed.135 Moreover, it should be noted that we created perforations in the body of the roots of mandibular molars, so our results cannot be applied to perforations at the furcation area or perforations in maxillary molars due to their different anatomy.
Last but not least, it should be kept in mind that root canal filling materials, such as sealers or gutta-percha points, may create streak artifacts on CBCT scans that can mimic root fractures, resulting in false positive results and the misdiagnosis of root fracture.20
In conclusion, the 2 CBCT systems had different results in terms of the detection of strip and root perforations. The Cranex 3D had non-significantly higher accuracy than the NewTom 3G. The high-resolution mode yielded significantly higher accuracy than the low-resolution mode. The diagnostic accuracy of CBCT scans was not affected by the perforation diameter.
References
1. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006; 13:95–107.

2. Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961; 14:83–91. PMID: 13717698.

3. de Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S, et al. Treatment outcome in endodontics: the Toronto study-phase 4: initial treatment. J Endod. 2008; 34:258–263. PMID: 18291271.

4. Shemesh H, Cristescu RC, Wesselink PR, Wu MK. The use of cone-beam computed tomography and digital periapical radiographs to diagnose root perforations. J Endod. 2011; 37:513–516. PMID: 21419300.

5. Gröndahl HG, Huumonen S. Radiographic manifestations of periapical inflammatory lesions. Endod Topics. 2004; 8:55–67.
6. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007; 40:818–830. PMID: 17697108.

7. Patel S, Dawood A, Mannocci F, Wilson R, Pitt Ford T. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009; 42:507–515. PMID: 19298574.

8. Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013; 39:548–557. PMID: 23522555.

9. Eskandarloo A, Mirshekari A, Poorolajal J, Mohammadi Z, Shokri A. Comparison of cone-beam computed tomography with intraoral photostimulable phosphor imaging plate for diagnosis of endodontic complications: a simulation study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:e54–e61. PMID: 22981099.

10. Spin-Neto R, Gotfredsen E, Wenzel A. Impact of voxel size variation on CBCT-based diagnostic outcome in dentistry: a systematic review. J Digit Imaging. 2013; 26:813–820. PMID: 23254628.

11. Venskutonis T, Juodzbalys G, Nackaerts O, Mickevicienė L. Influence of voxel size on the diagnostic ability of cone-beam computed tomography to evaluate simulated root perforations. Oral Radiol. 2013; 29:151–159.

12. Li G. Patient radiation dose and protection from cone-beam computed tomography. Imaging Sci Dent. 2013; 43:63–69. PMID: 23807928.

13. Davies J, Johnson B, Drage N. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac Radiol. 2012; 41:30–36. PMID: 22184626.

14. Skidmore AE, Bjorndal AM. Root canal morphology of the human mandibular first molar. Oral Surg Oral Med Oral Pathol. 1971; 32:778–784. PMID: 5286234.

15. Naitoh M, Nakahara K, Suenaga Y, Gotoh K, Kondo S, Ariji E. Comparison between cone-beam and multislice computed tomography depicting mandibular neurovascular canal structures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e25–e31. PMID: 20123365.

16. Cheng JG, Zhang ZL, Wang XY, Zhang ZY, Ma XC, Li G. Detection accuracy of proximal caries by phosphor plate and cone-beam computerized tomography images scanned with different resolutions. Clin Oral Investig. 2012; 16:1015–1021.

17. Dalili Z, Taramsari M, Mousavi Mehr SZ, Salamat F. Diagnostic value of two modes of cone-beam computed tomography in evaluation of simulated external root resorption: an in vitro study. Imaging Sci Dent. 2012; 42:19–24. PMID: 22474644.

18. Liedke GS, da Silveira HE, da Silveira HL, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009; 35:233–235. PMID: 19166780.

19. Khojastepour L, Moazami F, Babaei M, Forghani M. Assessment of root perforation within simulated internal resorption cavities using cone-beam computed tomography. J Endod. 2015; 41:1520–1523. PMID: 26025347.

20. Menezes RF, Araújo NC, Santa Rosa JM, Carneiro VS, Santos Neto AP, Costa V, et al. Detection of vertical root fractures in endodontically treated teeth in the absence and in the presence of metal post by cone-beam computed tomography. BMC Oral Health. 2016; 16:48. PMID: 27075880.

Fig. 1
Cleaning and shaping of the canal. The access cavity is prepared, the coronal pulp is excavated, and the root canals are cleaned and shaped using K-files via the step-back technique. To accomplish cleaning and shaping, ProTaper rotary files are used.
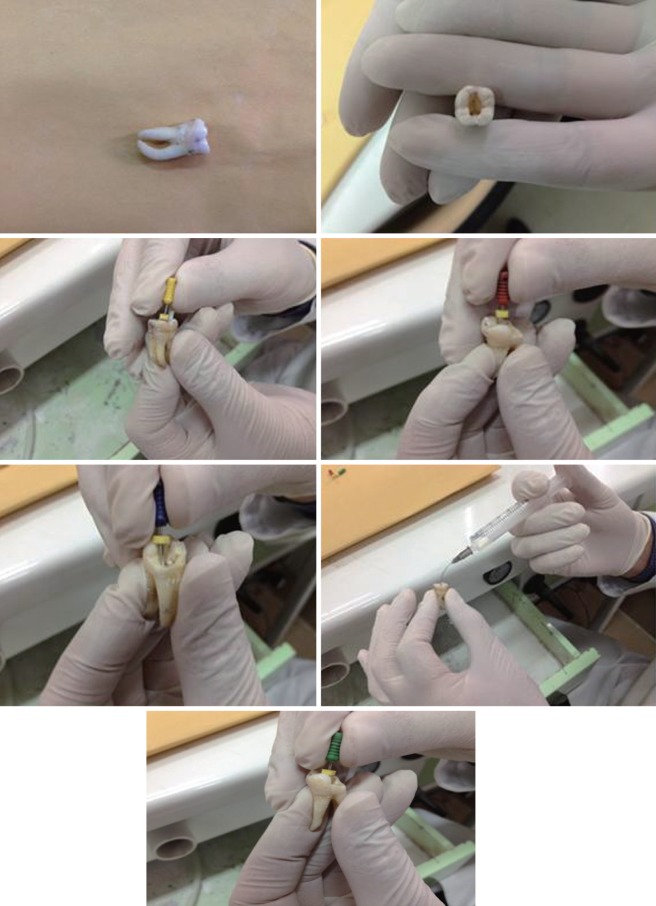
Fig. 2
Preparing root perforations. To create root perforations in the apical and middle thirds, the root canal wall is excessively filed at the curvature area using K-files. Perforations at the cervical area (strip perforation) are made using Gates Glidden drills.

Fig. 3
NewTom 3G cone-beam computed tomography (CBCT). To obtain NewTom 3G CBCT scans, a dry mandible was placed in a plastic container containing water and positioned in a position similar to those used in clinical settings.

Fig. 4
Cranex 3D CBCT system. The imaging procedure using the Cranex 3D is similar to that of the NewTom 3G. However, since imaging has to be done in the standing position, the mandible was positioned similarly to how the chin is placed in a chin rest in an area compatible with scanning.

Fig. 5
Scans obtained by the NewTom 3G and Cranex 3D systems. After data reconstruction at 0.2 mm intervals, the files were stored. Images were evaluated in the coronal, axial, and sagittal planes. A. NewTom 3G. B. Cranex 3D.
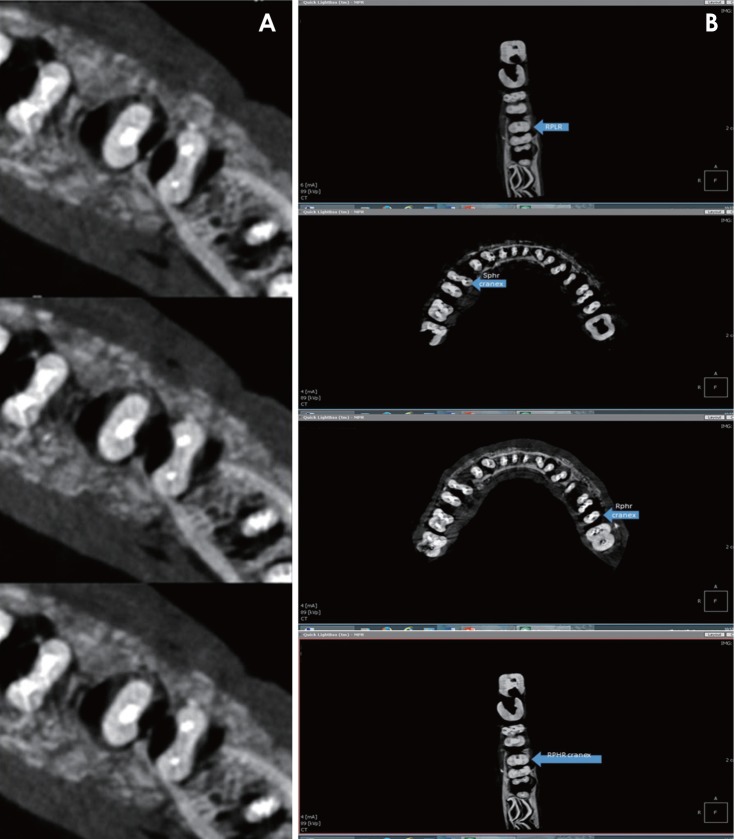
Table 1
Diagnostic accuracy of the first and second observers for detecting root perforations based on the imaging system
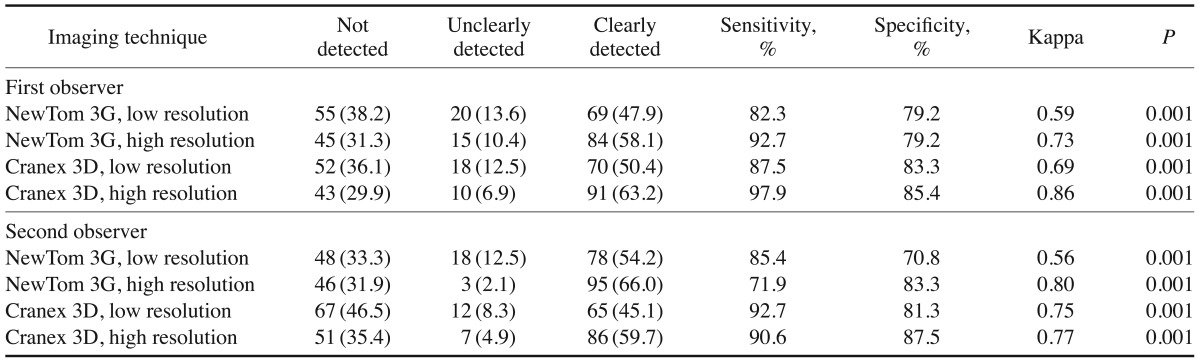
Table 2
Diagnostic accuracy of NewTom 3G and Cranex 3D cone-beam computed tomography (CBCT) scanners in high- and low-resolution modes
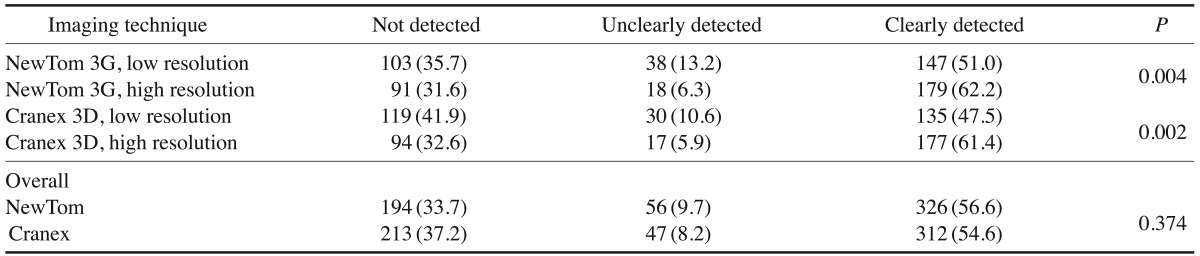
Table 3
Sensitivity, specificity, and kappa values of the different imaging systems according to the type of perforation




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download