Abstract
Osteosarcoma is a classical malignant bone-forming neoplasm which usually presents with an aggressive clinical course. The current case is presented with the radiographic feature of widening of the periodontal ligament space of the involved teeth, which is considered to be the earliest radiographic manifestation of osteosarcoma involving the jaw bone. The main aim of this case report was to focus on the importance of early diagnosis of this tumor based on clinical and radiographic examinations, and confirmation by histopathology. Considering the rarity of the disease type and particularly taking into account the fast progression and aggressiveness of this neoplasm, it is clear that the presentation of a clinical case represents a major contribution to better understanding of osteosarcomas involving the jaw bone.
Osteosarcoma is a primary malignant bone neoplasm characterized by osteoid synthesis by malignant osteoblasts.1 Evidence of direct osteoid formation by neoplastic cells is considered to be an essential criterion for its diagnosis, and microscopic evidence of neoplastic bone, even if it is very minimal, confirms its diagnosis.1
The jaw bone is considered to be the most common site in the head and neck region.1 Osteosarcoma of the jaws is slightly more common in males and occurs at a later age compared to that occurring in long bones.1
Swelling of the jaw with associated pain and tooth mobility is the common clinical manifestation, and it presents radiographically as an osteolytic, osteoblastic, or mixed lesion. Also, symmetric widening of the periodontal ligament space of the involved teeth (positive Garrington's sign) might be seen.2
Biologically, osteosarcoma of the jaw is considered to be less aggressive with lower incidence of metastasis and hence associated with a better prognosis compared to that occurring in long bones.2
This report described a case of osteosarcoma of the right posterior mandible, which clinically presented as soft tissue growth from the gingiva, mimicking a common benign reactive lesion such as pyogenic granuloma. This report highlighted its early diagnosis based on simple, yet rare radiographic findings for osteosarcoma, that is, widening of the periodontal ligament space, despite its misleading clinical presentation as a more common reactive lesion.
A 40-year-old female reported with the chief complaint of swelling in the right side of the lower jaw for the previous 10 days. The patient's medical and dental history was unremarkable, and the patient did not seem to have any harmful habits.
On extraoral examination, there was a swelling in the right mandible with a normal color and texture of the overlying skin. Mouth opening was found to be normal. Paraesthesia was detected in the skin over the swelling. The right submandibular lymph node was of 2 cm in size, palpable, tender, and non-fixed.
Intraoral examination revealed a nodular swelling in the right mandible extending from the mandibular canine to the mandibular first molar. It measured approximately 3 cm×5 cm. The overlying mucosa was eyrthematous in appearance and the borders were well defined, with a consistency varying from firm to hard. Tenderness was present on palpation. The teeth near the swelling were not mobile (Fig. 1).
A panoramic radiograph revealed a periradicular widening of the periodontal ligament space and loss of lamina dura involving the right mandibular second premolar and the mesial and distal roots of the first molar with mild rarefaction of the inter-dental alveolar bone between the roots of the mandibular right first molar and second molar (Fig. 2).
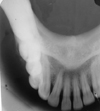
An intraoral periapical radiograph revealed a loss of the lamina dura and periradicular bone loss involving the interdental bone between the mandibular right second premolar and first molar (Fig. 3). A shadow of the soft tissue mass on the right side and mild peripheral cortical bone reactive bone formation in the molar and premolar region were visible in the right mandibular lateral occlusal radiograph (Fig. 4). Correlating the clinical and radiographic features, a provisional diagnosis of osteosarcoma involving the jaw bone was made.
Incisional biopsy of the lesion was performed, and the hematoxylin-eosin stained section showed highly cellular connective tissue stroma, predominantly composed of neoplastic spindle cells that exhibited pleomorphism and hyperchromatism. Abundant neoplastic osteoid formation with varying degrees of calcification was seen within the stroma. The neoplastic bone showed typical peripheral rim of malignant osteoblasts as well as entrapped pleomorphic, hyperchromatic cells. Mitotic figures were also seen in the stroma (Fig. 5). A histopathological diagnosis of osteosarcoma was made.
Based on the report, segmental resection of the right body of the mandible was performed with wide surgical resection margins. The resected tumor specimen also exhibited similar histopathological findings consistent with the incisional biopsy report of osteosarcoma.
Soft tissue growth involving the gingiva is a very common clinical presentation in the oral cavity and is the clinical presentation of more common benign reactive lesions such as pyogenic granuloma.3 These lesions often do grow rapidly like neoplasms and appear reddish, due to their inherently vascular nature and present with surface ulceration due to frictional trauma in the oral cavity.3
Subtle radiographic changes such as inter-dental bone loss associated may be seen in these lesions without any distinctive radiolucent or osteolytic areas involving the body of the jaw bone, since these benign reactive lesions practically never invade the bone, unlike aggressive malignant neoplasms.
This patient also presented with a rapidly growing soft tissue mass with an erythematous surface involving the gingiva of the right mandible like a more common benign reactive lesion. Panoramic and periapical radiographs did not reveal any significant osteolytic or mixed (osteolytic and osteoblastic) lesions involving the right body of the mandible, except for the following features: widening of the periodontal ligament (PDL) space, loss of the lamina dura, and periradicular interdental alveolar bone loss involving the mandibular right first molar and second premolar.
Considering the rarity of this lesion, clinically for the present case, though pyogenic granuloma could not be ruled out in the differential diagnosis, more importance was placed on specific radiographic changes, that is, the widening of the PDL space and mild peripheral reactive cortical bone formation, a first provisional diagnosis of osteosarcoma involving the jaw bone was made, which was later confirmed in both incisional biopsy and the final histopathology of the lesion.
The most common radiographic differential diagnosis for localized widening of the PDL space is trauma from occlusion or periapical infectious pathology. Some rare diseases such as scleroderma also can manifest as widening of the PDL space involving the posterior teeth. However, for the present case, the rapidly growing mass involving the gingiva along with the abovementioned radiographic features aided us in establishing with more certainty the provisional diagnosis of osteosarcoma.
The early lesion of osteosarcoma of the jaw usually occurs as a lobular mass involving the surface of the bone with sessile attachment of the lesion to the cortex and with very minimal or no trabecular involvement. The advanced lesion may show extensive trabecular infiltration.4,5
The more typical 'sun-burst' or 'sun-ray' reaction of osteosarcoma involving the peripheral bone is almost always absent in osteosarcoma involving the jaw bone.4,5
Due to the rapid progression of the lesion in soft tissue such as the PDL, osteosarcoma involving the alveolus may present with typical radiographic signs of symmetrical widening of the periodontal ligament space. This is very rare and not considered to be pathognomonic for osteosarcoma.5
Histopathologically, osteosarcoma involving the jaw bone is osteoblastic or chondroblastic in nature, with deposition of a variable amount of osteoid matrix and minimal cytological atypia, and is usually characterized by well-differentiated lesions.6 In the present case, histologically the tumor mass was mainly composed of cells with shapes varying between oval and spindle, which were responsible for the deposition of extensive osteoid areas, as was typical of the osteoblastic type.
Adequate surgical excision of the primary lesion with postoperative radiotherapy or chemotherapy in appropriate situations remains the mainstay of treatment for osteosarcoma of the jaw bone.7 Factors associated with good prognosis are a small tumor size, absence of nerve involvement, adequate surgical margin, histologically well differentiated lesion, and younger patients without associated retinoblastoma.7
Osteosarcoma of the jaws has a better prognosis than that of the long bones. The survival rate with jaw osteosarcoma is about 50%, compared to a 30% 5-year survival rate with long bone osteosarcoma. Therapeutic failure usually occurs due to local recurrence and also due to lung metastasis followed by metastasis to the brain and then to other bones. All of the distant metastasis occurs through tumor emboli in veins that either flow downstream to the right side of the heart where they are pumped into and lodged in the capillaries of the lungs or via retrograde flow to the brain or to other bones.8
In conclusion, though widening of the PDL space is considered rare and not a pathognomonic sign of an osteosarcoma, due attention should be paid to this simple, distinctive, and easily identifiable radiographic finding in relevant clinical situations for the early diagnosis of osteosarcoma involving the jaw bone.
Figures and Tables
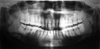 | Fig. 2A panoramic radiograph shows the loss of the lamina dura and widening of the periodontal ligament space involving the right permanent mandibular first molar and second premolar with mild rarefaction of the interdental alveolar bone between the right mandibular first molar and second molar. |
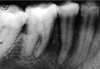 | Fig. 3A periapical radiograph shows the loss of the lamina dura and periradicular bone loss involving the interdental bone between the right permanent mandibular second premolar and first molar. |
References
1. Khorate MM, Goel S, Singh MP, Ahmed J. Osteosarcoma of mandible: a case report and review of literature. J Cancer Sci Ther. 2010; 2:122–125.
2. Ong ST, Shim CK, Ng KH, Siar CH. Osteosarcoma presenting as an aggressive nodular mass in the region of the mandible. J Oral Sci. 2004; 46:55–59.

3. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 3rd ed. St. Louis: Saunders/Elsevier;2009. p. 517–519.
4. Donaldson ME, Geist JR, Daley TD. Osteosarcoma of the jaws in children. Int J Paediatr Dent. 2004; 14:54–60.

5. Bras JM, Donner R, van der Kwast WA, Snow GB, van der Waal I. Juxtacortical osteogenic sarcoma of the jaws. Review of the literature and report of a case. Oral Surg Oral Med Oral Pathol. 1980; 50:535–544.
6. Anil S, Krishnan AP, Rajendran R. Osteosarcoma of the mandible masquerading as a dental abscess: report of a case. Case Rep Dent. 2012; 2012:635062.

7. Amaral MB, Buchholz I, Freire-Maia B, Reher P, de Souza PE, Marigo Hde A, et al. Advanced osteosarcoma of the maxilla: a case report. Med Oral Patol Oral Cir Bucal. 2008; 13:E492–E495.
8. Marx RE, Stern D. Oral and Maxillofacial Pathology: a rationale for diagnosis and treatment. Chicago: Quintessence Pub Co;2003. p. 805–806.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download