Abstract
Purpose
This study was performed to identify correlations between keratocystic odontogenic tumor (KCOT) data from CT sections, and data on the KCOT clinical manifestation and resulting dental expenses.
Materials and Methods
Following local Institutional Review Board (IRB) approval, a seven-years of retrospective study was performed regarding patients with KCOTs treated at the Seoul National University Dental Hospital. A total of 180 KCOT were included in this study. The following information was collected: age, gender, location and size of the lesion, radiological features, surgical treatment provided and dental expenses.
Results
There was no significant association between the size of the KCOT and age, gender, and presenting preoperative symptoms. In both jaws, it was unusual to find KCOTs under 10 mm. The correlation between the number of teeth removed and the size of the KCOT in the tooth bearing area was statistically significant in the mandible, whereas in the maxilla, no significant relationship was found. Dental expenses compared with the size of the KCOT were found to be significant in both jaws.
Conclusion
The size of KCOT was associated with a significant increase in dental expenses for both jaws and the number of teeth removed from the mandible. These findings emphasize the importance of routine examinations and early detection of lesions, which in turn helps preserving anatomical structures and reducing dental expenses.
Keratocystic odontogenic tumor (KCOT), formerly regarded as odontogenic keratocyst, is a benign neoplasm of odontogenic origin. KCOTs comprise 12% of all odontogenic cysts of the jaws.1 Radiographically, the tumor presents as a unilocular or multilocular, sometimes expansile radiolucent lesion. Preoperative diagnosis of KCOT to distinguish it from other odontogenic cysts is important due to its high recurrence rate, which ranges from 13% to 58%.2-5 Since surgical treatment of KCOT is more invasive than that for other odontogenic cysts, early detection of KCOT is crucial to minimize surgical morbidity and preserve adjacent vital structures.
The clinical type, location, size of the lesion and the patient's age should be considered in choosing the most appropriate treatment for KCOTs. The radiographic features are an important factor for treatment planning. Advanced imaging modalities or frequent imaging examinations help in identifying small lesions while they remain relatively simple to remove. Presumably, symptomatic KCOTs might be larger, more destructive, and more difficult to treat.4 In severe cases, the mandible might be sacrificed.2
Most studies on KCOT thus far concern therapeutic approaches, evaluating different surgical treatment methods for KCOTs and reporting the outcome.6 Therefore, little is known about the radiographic characteristics of KCOT in association with clinical features. Due to the lack of adequate radiographic documentation in previous retrospective studies, it has been impossible to examine data regarding removal or maintenance of teeth in direct contact with the lesion. Computerized tomography (CT) is a very valuable tool in diagnosis and treatment planning, providing the present real dimension values.7 The relationship of a lesion to the teeth, cortical expansion and erosion, and the boundary of a lesion can be evaluated.8 Our study analyzed computed tomography (CT) section data of KCOTs in different phases of progression.
The purpose of this study was to present a series of keratocystic odontogenic tumors (KCOTs), analyzing data from CT sections and correlating the data to clinical manifestations and dental expenses.
The present study was approved by the Institutional Review Board at Seoul National University Dental Hospital and carried out according to institutional guidelines. We identified a total of 334 patients diagnosed histologically with keratocystic odontogenic tumor from 2004 to 2010 at Seoul National University Dental Hospital. Among them, the patients that had undergone surgical treatment for KCOT were initially eligible for this study. Inclusion criteria were patients with a definite histopathologic diagnosis of KCOT who had a CT scan (Somatom Sensation 10, Siemens, Erlangen, Germany) taken during the preoperative analysis. Exclusion criteria were 1) patients treated elsewhere with no surgical treatment provided at SNUDH and 2) patients undergoing surgery due to recurrence.
Based on these criteria, in the end, 180 patients were included in the present study. Using their dental records, the available information was reviewed, which was gender, age at diagnosis, clinical manifestations, site of involvement, radiographic measurement, and treatment modality. KCOTs were diagnosed in one of two different ways. First, the lesion was identified incidentally by routine examination or radiograph. Second, it was clinically identified with symptoms such as pain, swelling or drainage.
The location of the KCOTs in the maxilla or mandible was noted, and they were further subdivided into the following groups: 1) maxillary incisor and canine, 2) maxillary premolar, 3) maxillary molar and tuberosity, 4) maxillary sinus, 5) mandibular incisor and canine, 6) mandibular premolar, 7) mandibular molar, 8) mandibular angle and ramus, 9) mandibular coronoid process, and 10) mandibular condyle.
The treatment provided for each KCOT was also recorded as determined by a review of the surgical report. All of the KCOTs described in this report were treated by enucleation with peripheral ostectomy. Any adjunctive method such as marsupialization, bone graft, or en bloc resection was noted with each case.
The radiographs were saved as digital imaging and communications in medicine (DICOM) files. All of the radiographs were evaluated by one radiologist.
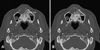
The size of each KCOT was measured on the CT slices using the axial plane in millimeters. The measurements were made by using a picture archiving and communication system (PACS) viewer (PiView STAR, Infinitt, Seoul, Korea). On the axial view, the longest mesio-distal and bucco-lingual dimensions were obtained. For the mandibular lesions, the mesio-distal dimension was measured parallel to the long axis of the mandibular body (Fig. 1A). The bucco-lingual dimension was measured perpendicular to the long axis of the mandibular body (Fig. 1B). On the maxillary axial view, the mesio-distal dimension was measured parallel to the coronal plane of the maxilla (Fig. 2A), and the bucco-lingual dimension was measured parallel to the sagittal plane of the maxilla (Fig. 2B). If the lesion involved both the tooth bearing area and non-tooth bearing area, the size of the tooth bearing area was measured separately. The tooth bearing area was defined as the area mesial to the distal surface of the secondary molar and superior to the apex of the roots in the maxilla. If the lesion fenestrated the buccal or lingual bone wall, it was recorded as having cortical discontinuity.
The number of teeth removed during surgery and teeth treated with a root canal associated with the lesion were also counted. In cases where tooth removal was conducted during surgery, it was assumed that rehabilitation by means of dental implants was needed. Dental expenses were estimated as a sum total of all the medical costs of adjunctive treatment, root canal treatment, and the prosthetic rehabilitation of the missing tooth. The values were adjusted by the SNUDH price index. In order to perform statistical analysis, estimated dental expenses were then classified into 4 groups according to the values. The dental expenses increased from group1 to group4.
All of the measurements were evaluated for the maxillary and mandibular lesions separately. In cases of multiple lesions occurring independently in a separate jawbone, the lesion largest in size was subject to measurement.
All of the statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) for Windows version 16.0. A paired t-test and Pearson's χ2 were used to assess the differences in patients with or without preoperative symptoms and cortical discontinuity in the study group. Analysis of variance (ANOVA) and Tukey's post hoc test were used for assessing the KCOT size by comparing several variables such as dental expenses, number of root canal treatments, and number of teeth removed. A 95% significance level was used for all of the statistical tests (P<0.05). Due to the homogeneity in the data within the study groups and a non-normal distribution of the data, all variables were transformed in order to reduce the variance and stabilize normality.
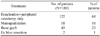
Our patient group was distributed in a wide age range from 9 to 80 years of age (mean, 36.8 years). There were 93 males (51.6%) and 87 females (48.3%) (ratio 1.1 : 1). The 117 patients (65%) presented with symptoms such as swelling, pain, drainage, and discomfort, whereas the remaining 63 (35%) were diagnosed incidentally at the time of routine examination (Table 1).
Cortical discontinuity was found in 119 of the 198 lesions (60.1%). Fifty-five lesions (27.7%) were maxillary and 143 were mandibular (ratio 1 : 2.6). The most frequently involved regions were the mandibular molar, angle, and ramus (57.2%). The maxillary molar and tuberosity region was the next most common location (11.0%). The majority (88.1%) of the KCOT's were located posterior to the canines (Table 2).
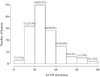
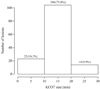
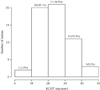
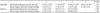
Radiographically, the size of the mandibular lesions ranged from 7.4 to 75.2mm(mean size of 29.9 mm) mesiodistally and from 4.9 to 27.5 mm (mean size of 14.0 mm) bucco-lingually. In the maxilla, the mean size of the lesions was 23.1 mm, with the smallest being 5.7 and the largest 44.1 mm mesio-distally, and the mean size of the lesion was 20.1 mm, with the smallest being 4.1 mm and the largest 49.2 mm. Most lesions measured over 10 mm (Figs. 3, 4, 5, 6). No statistically significant correlation with the KCOT size was found for age or for gender. Marsupialization was performed to treat 10% (18/180) of the cases. Bone graft was performed to treat 25% (45/180). Resection was performed to treat 1.1% (2/180) (Table 3).
All of the results are summarized in Tables 4, 5, 6. In the mandible, there were no statistically significant differences in bucco-lingual dimensions (P=0.218), number of teeth removed (P=0.335), number of root canal treatments (P=0.288), or dental expenses (P=0.239) between symptomatic patients and non-symptomatic patients. However, there were significantly smaller mesio-distal dimensions in non-symptomatic patients (P=0.016). In the maxilla, no statistically significant correlation was found between the initial symptoms and mesio-distal dimensions (P=0.182), bucco-lingual dimensions (P=0.689), number of teeth removed, number of root canal treatments, or dental expenses.
A statistically significant correlation was found for the presenting cortical discontinuity and the mesio-distal and bucco-lingual dimensions of the KCOTs (P<0.05, Table 6) in the mandible. In the maxilla, however, no statistically significant correlation was found between the cortical discontinuity and the mesio-distal (P=0.384) and bucco-lingual (P=0.682) dimensions of the KCOTs.
An ANOVA test for the dental expense data indicated that larger mandibular KCOT size was correlated with greater dental expenses (Table 7). Another ANOVA test indicated that the bucco-lingual dimension in tooth bearing area but not the mesio-distal dimension in the tooth bearing area increased with an increasing number of teeth removed (Table 8). In the maxillary KCOTs in the present study, there were no correlations between the size effects and the variables of interest. However, a statistically significant correlation was found between the bucco-lingual dimensions and dental expenses.
Finally, an ANOVA test indicated that the number of root canal treatments increased with the mesio-distal dimensions but did not differ by the bucco-lingual dimensions. In the maxilla, the number of root canal treatments increased with the mesio-distal and bucco-lingual dimensions of KCOTs (Table 9).
Among 180 patients with KCOTs, the slight male predominance and the male-to-female ratio of 1.1 was nearly identical to that of Japanese and British patients in previous studies.1,5 Our patients' mean age of 36.8 years was similar to the mean age of 37 years in a study by Brannon.9 The youngest patient in our study was a 9-year-old girl without symptoms.
Researchers have reported that 50% to 67% of KCOTs are symptomatic at the time of diagnosis,9-11 and which corresponds with our study. Some of our patients presented with swelling, pain and even pus discharge, while some others were asymptomatic.
The mandible was involved in 72.2% of cases, with a predilection for the posterior molar area, angle, and ascending ramus. These findings were in agreement with earlier studies, in which 70% of tumors were located in the mandible.1,5,12
Numerous studies have been carried out to evaluate relationship between the recurrence rate and surgical treatment performed. However, little is known about the relationship between radiographic imaging characteristics of KCOT and its clinical features. Most previous measurements of radiologic KCOT dimensions were performed on periapical and occlusal radiographs, and therefore they were difficult to standardize. Our report presented a series of KCOTs by analyzing data from CT sections and correlating the data to the clinical manifestation, (i.e., preoperative symptoms) and the dental expenses. Previous researchers have assumed that symptomatic KCOTs are larger, more destructive, and more difficult to treat.4,13 However, in this study, no statistically significant correlation with the size of KCOT was found for age or gender or for presenting preoperative symptoms.
The correlation between the number of teeth removed and the dimensions of the lesion in the tooth bearing area was statistically significant in the mandible, whereas in the maxilla, no significant relationship was found. This might be due to the fact that KCOT lesions in the maxilla developed in a complex fashion, involving the maxillary sinus instead of a simple bucco-lingual expansion.
The number of root canal treatments increased with the mesio-distal dimensions but did not differ by the bucco-lingual dimensions of the mandibular lesions. In the maxilla, the number of root canal treatments increased with both the mesio-distal and bucco-lingual dimensions of the lesions.
The dental expenses were found to be significantly related to the mandibular KCOT size. It was observed that lower cost was associated with a smaller KCOT size. In the maxilla, a statistically significant correlation was found between the bucco-lingual dimensions of the cysts and dental expenses.
In this study, the recurrence rate showed no significant association with the size of the lesion. However, the recurrence time after surgery showed a significant association with the KCOT size. Patients undergoing surgery due to recurrence were excluded from this study, thus decreasing the sample size. A larger sample size could better demonstrate the association between the size of the lesion and recurrence, if such an association exists.
Overall, this study found that the size of KCOT was significantly associated with increased dental expenses. In both jaws, it was unusual to find KCOTs less than 10 mm. This is because a KCOT might continue to grow if the lesions are asymptomatic and no radiographic evaluation has been performed. These findings strongly support the importance of routine examinations for recognizing initial lesions.14 Early detection of these lesions will reduce the risk of losing anatomical structures during surgical procedures and lower the total dental expenses as well.
Figures and Tables
Fig. 1
Measurements of keratocystic odontogenic tumor in the mandible using axial computed tomographic images. A. The longest mesiodistal dimension of the cystic lesion is measured parallel to the long axis of the mandibular body. B. The longest bucco-lingual dimension of the cystic lesion is measured perpendcular to the long axis of the mandibular body.
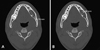
Fig. 2
Measurements of keratocystic odontogenic tumor in the maxilla using axial computed tomographic images. A. The longest mesiodistal dimension of the cystic lesion is measured parallel to the coronal plane of the maxilla. B. The longest bucco-lingual dimension of the cystic lesion is measured parallel to the sagittal plane of the maxilla.
References
1. Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006; 35:500–507.

2. Myoung H, Hong SP, Hong SD, Lee JI, Lim CY, Choung PH, et al. Odontogenic keratocyst: review of 256 cases for recurrence and clinicopathologic parameters. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:328–333.

3. Zhao YF, Wei JX, Wang SP. Treatment of odontogenic keratocysts: a follow-up of 255 Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:151–156.

4. Morgan TA, Burton CC, Qian F. A retrospective review of treatment of the odontogenic keratocyst. J Oral Maxillofac Surg. 2005; 63:635–639.

5. González-Alva P, Tanaka A, Oku Y, Yoshizawa D, Itoh S, Sakashita H, et al. Keratocystic odontogenic tumor: a retrospective study of 183 cases. J Oral Sci. 2008; 50:205–212.

6. Güler N, Sençift K, Demirkol O. Conservative management of keratocystic odontogenic tumors of jaws. ScientificWorldJournal. 2012; 2012:680397.

7. Crusoé-Rebello I, Oliveira C, Campos PS, Azevedo RA, dos Santos JN. Assessment of computerized tomography density patterns of ameloblastomas and keratocystic odontogenic tumors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:604–608.

8. Boeddinghaus R, Whyte A. Current concepts in maxillofacial imaging. Eur J Radiol. 2008; 66:396–418.

9. Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg Oral Med Oral Pathol. 1976; 42:54–72.
10. Crowley TE, Kaugars GE, Gunsolley JC. Odontogenic keratocysts: a clinical and histologic comparison of the parakeratin and orthokeratin variants. J Oral Maxillofac Surg. 1992; 50:22–26.

11. Dammer R, Niederdellmann H, Dammer P, Nuebler-Moritz M. Conservative or radical treatment of keratocysts: a retrospective review. Br J Oral Maxillofac Surg. 1997; 35:46–48.

12. Minami M, Kaneda T, Ozawa K, Yamamoto H, Itai Y, Ozawa M, et al. Cystic lesions of the maxillomandibular region: MR imaging distinction of odontogenic keratocysts and ameloblastomas from other cysts. AJR Am J Roentgenol. 1996; 166:943–949.





 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download