1. Munjack DJ, Kanno PH. Retarded ejaculation: a review. Arch Sex Behav. 1979; 8:139–150. PMID:
112949.

2. Shull GR, Sprenkle DH. Retarded ejaculation reconceptualization and implications for treatment. J Sex Marital Ther. 1980; 6:234–246. PMID:
6152867.

3. Segraves RT. Considerations for a better definition of male orgasmic disorder in DSM V. J Sex Med. 2010; 7:690–695. PMID:
20492418.

4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association;2013.
5. Rowland D, McMahon CG, Abdo C, Chen J, Jannini E, Waldinger MD, et al. Disorders of orgasm and ejaculation in men. J Sex Med. 2010; 7:1668–1686. PMID:
20388164.

6. Perelman MA. Psychosexual therapy for delayed ejaculation based on the sexual tipping point model. Transl Androl Urol. 2016; 5:563–575. PMID:
27652228.

7. Perelman MA. Reexamining the definitions of PE and DE. J Sex Marital Ther. 2017; 43:633–644. PMID:
27594579.

8. Waldinger MD, Quinn P, Dilleen M, Mundayat R, Schweitzer DH, Boolell M. A multinational population survey of intravaginal ejaculation latency time. J Sex Med. 2005; 2:492–497. PMID:
16422843.
9. Patrick DL, Althof SE, Pryor JL, Rosen R, Rowland DL, Ho KF, et al. Premature ejaculation: an observational study of men and their partners. J Sex Med. 2005; 2:358–367. PMID:
16422867.
10. Waldinger MD, McIntosh J, Schweitzer DH. A five-nation survey to assess the distribution of the intravaginal ejaculatory latency time among the general male population. J Sex Med. 2009; 6:2888–2895. PMID:
19627471.

11. Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999; 281:537–544. PMID:
10022110.
12. Fugl-Meyer AR, Sjögren Fugl-Meyer K. Sexual disabilities, problems, and satisfaction in 18–74 year old Swedes. Scand J Sexol. 1999; 3:79–105.
13. Simons JS, Carey MP. Prevalence of sexual dysfunctions: results from a decade of research. Arch Sex Behav. 2001; 30:177–219. PMID:
11329727.
14. Perelman MA, Rowland DL. Retarded ejaculation. World J Urol. 2006; 24:645–652. PMID:
17082938.

15. Paduch DA, Polzer P, Morgentaler A, Althof S, Donatucci C, Ni X, et al. Clinical and demographic correlates of ejaculatory dysfunctions other than premature ejaculation: a prospective, observational study. J Sex Med. 2015; 12:2276–2286. PMID:
26511106.

16. Nathan SG. The epidemiology of the DSM-III psychosexual dysfunctions. J Sex Marital Ther. 1986; 12:267–281. PMID:
3493350.

17. Nazareth I, Boynton P, King M. Problems with sexual function in people attending London general practitioners: cross sectional study. BMJ. 2003; 327:423. PMID:
12933729.

18. Blanker MH, Bosch JL, Groeneveld FP, Bohnen AM, Prins A, Thomas S, et al. Erectile and ejaculatory dysfunction in a community-based sample of men 50 to 78 years old: prevalence, concern, and relation to sexual activity. Urology. 2001; 57:763–768. PMID:
11306400.

19. Corona G, Lee DM, Forti G, O'Connor DB, Maggi M, O'Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European male ageing study (EMAS). J Sex Med. 2010; 7:1362–1380. PMID:
19929914.

20. Rosen RC, Heiman JR, Long JS, Fisher WA, Sand MS. Men with sexual problems and their partners: findings from the international survey of relationships. Arch Sex Behav. 2016; 45:159–173. PMID:
26228991.

21. Perelman MA. Patient highlights. Delayed ejaculation. J Sex Med. 2013; 10:1189–1190. PMID:
23551543.
22. Butcher MJ, Welliver RC Jr, Sadowski D, Botchway A, Köhler TS. How is delayed ejaculation defined and treated in North America? Andrology. 2015; 3:626–631. PMID:
26013106.

23. Althof SE. Psychological interventions for delayed ejaculation/orgasm. Int J Impot Res. 2012; 24:131–136. PMID:
22378496.

24. Masters WH, Johnson VE. Human sexual inadequacy. Boston: Little, Brown;1970.
25. Bancroft J. Human sexuality and its problem. London: Churchill Livingstone;2008.
26. Rowland DL, Keeney C, Slob AK. Sexual response in men with inhibited or retarded ejaculation. Int J Impot Res. 2004; 16:270–274. PMID:
14961061.

27. Teloken P, Nelson C, Mulhall J. Secondary delayed orgasm: patterns, correlates and predictors. J Urol. 2012; 187:e562.
28. Xia JD, Han YF, Pan F, Zhou LH, Chen Y, Dai YT. Clinical characteristics and penile afferent neuronal function in patients with primary delayed ejaculation. Andrology. 2013; 1:787–792. PMID:
23970455.

29. Nelson CJ, Ahmed A, Valenzuela R, Parker M, Mulhall JP. Assessment of penile vibratory stimulation as a management strategy in men with secondary retarded orgasm. Urology. 2007; 69:552–555. discussion 555-6. PMID:
17382163.

30. Perelman MA. Idiosyncratic masturbation patterns: a key unexplored variable in the treatment of retarded ejaculation by the practicing urologist. J Urol. 2005; 173:340. PMID:
15643170.
31. Apfelbaum B. Retarded ejaculation: a much-misunderstood syndrome. In : Lieblum SR, Rosen RC, editors. Principles and practice of sex therapy. 2nd ed. New York: Guilford Press;1989. p. 168–202.
32. Apfelbaum B. Retarded ejaculation: a much-misunderstood syndrome. In : Leiblum SR, Rosen RC, editors. Principles and practice of sex therapy. 3rd ed. New York: Guilford Press;2000. p. 205–241.
33. Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts male aging study. J Urol. 1994; 151:54–61. PMID:
8254833.

34. O'Leary MP, Rhodes T, Girman CJ, Jacobson DJ, Roberts RO, Lieber MM, et al. Distribution of the brief male sexual inventory in community men. Int J Impot Res. 2003; 15:185–191. PMID:
12904804.
35. Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011; 34:41–48. PMID:
20345874.

36. Edwards AE, Husted JR. Penile sensitivity, age, and sexual behavior. J Clin Psychol. 1976; 32:697–700. PMID:
956441.

37. Halata Z, Munger BL. The neuroanatomical basis for the protopathic sensibility of the human glans penis. Brain Res. 1986; 371:205–230. PMID:
3697758.

38. Tammaro A, Parisella FR, Cavallotti C, Persechino S, Cavallotti C. Ultrastructural age-related changes in the sensory corpuscles of the human genital skin. J Biol Regul Homeost Agents. 2013; 27:241–245. PMID:
23489703.
39. Rowland DL, Greenleaf W, Mas M, Myers L, Davidson JM. Penile and finger sensory thresholds in young, aging, and diabetic males. Arch Sex Behav. 1989; 18:1–12. PMID:
2712681.

40. Rowland DL. Penile sensitivity in men: a composite of recent findings. Urology. 1998; 52:1101–1105. PMID:
9836563.

41. Montejo AL, Montejo L, Navarro-Cremades F. Sexual side-effects of antidepressant and antipsychotic drugs. Curr Opin Psychiatry. 2015; 28:418–423. PMID:
26382168.

42. Hendren SK, O'Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ, et al. Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg. 2005; 242:212–223. PMID:
16041212.

43. Brindley GS, Gillan P. Men and women who do not have orgasms. Br J Psychiatry. 1982; 140:351–356. PMID:
7093610.

44. Richardson D, Nalabanda A, Goldmeier D. Retarded ejaculation: a review. Int J STD AIDS. 2006; 17:143–150. PMID:
16509998.
45. Foley S. The complex etiology of delayed ejaculation: assessment and treatment implications. J Fam Psychother. 2009; 20:261–282.

46. Jern P, Santtila P, Witting K, Alanko K, Harlaar N, Johansson A, et al. Premature and delayed ejaculation: genetic and environmental effects in a population-based sample of Finnish twins. J Sex Med. 2007; 4:1739–1749. PMID:
17888070.

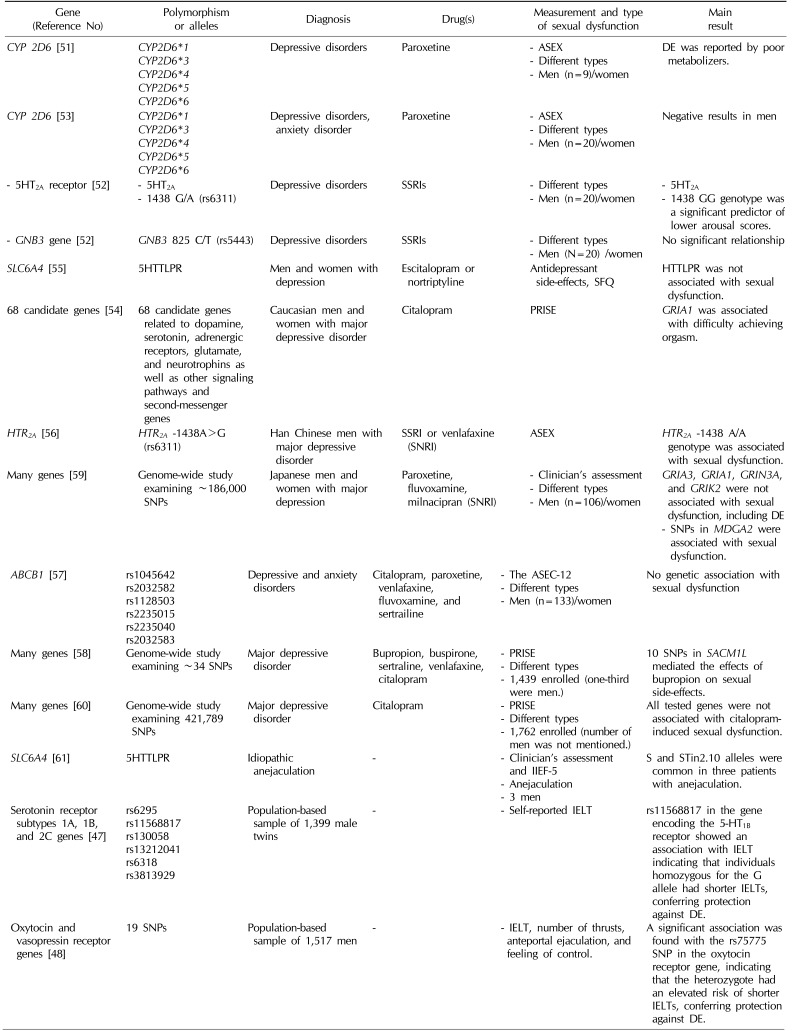
47. Jern P, Westberg L, Johansson A, Gunst A, Eriksson E, Sandnabba K, et al. A study of possible associations between single nucleotide polymorphisms in the serotonin receptor 1A, 1B, and 2C genes and self-reported ejaculation latency time. J Sex Med. 2012; 9:866–872. PMID:
22240001.

48. Jern P, Westberg L, Johansson A, Jonsson L, Corander J, Sandnabba NK, et al. Are single nucleotide polymorphisms in the oxytocin and vasopressin 1A/1B receptor genes likely candidates for variation in ejaculatory function? BJU Int. 2012; 110:E1173–E1180. PMID:
22882465.

49. Corona G, Ricca V, Bandini E, Mannucci E, Lotti F, Boddi V, et al. Selective serotonin reuptake inhibitor-induced sexual dysfunction. J Sex Med. 2009; 6:1259–1269. PMID:
19473282.
50. Stevenson JM, Bishop JR. Genetic determinants of selective serotonin reuptake inhibitor related sexual dysfunction. Pharmacogenomics. 2014; 15:1791–1806. PMID:
25493571.

51. Zourková A, Hadasová E. Relationship between CYP 2D6 metabolic status and sexual dysfunction in paroxetine treatment. J Sex Marital Ther. 2002; 28:451–461. PMID:
12378847.
52. Bishop JR, Moline J, Ellingrod VL, Schultz SK, Clayton AH. Serotonin 2A -1438 G/A and G-protein Beta3 subunit C825T polymorphisms in patients with depression and SSRI-associated sexual side-effects. Neuropsychopharmacology. 2006; 31:2281–2288. PMID:
16710319.

53. Zourková A, Cesková E, Hadasová E, Ravcuková B. Links among paroxetine-induced sexual dysfunctions, gender, and CYP2D6 activity. J Sex Marital Ther. 2007; 33:343–355. PMID:
17541852.
54. Perlis RH, Laje G, Smoller JW, Fava M, Rush AJ, McMahon FJ. Genetic and clinical predictors of sexual dysfunction in citalopram-treated depressed patients. Neuropsychopharmacology. 2009; 34:1819–1828. PMID:
19295509.

55. Strohmaier J, Wüst S, Uher R, Henigsberg N, Mors O, Hauser J, et al. Sexual dysfunction during treatment with serotonergic and noradrenergic antidepressants: clinical description and the role of the 5-HTTLPR. World J Biol Psychiatry. 2011; 12:528–538. PMID:
21388237.
56. Liang CS, Ho PS, Chiang KT, Su HC. 5-HT2A receptor -1438 G/A polymorphism and serotonergic antidepressant-induced sexual dysfunction in male patients with major depressive disorder: a prospective exploratory study. J Sex Med. 2012; 9:2009–2016. PMID:
22612784.

57. de Klerk OL, Nolte IM, Bet PM, Bosker FJ, Snieder H, den Boer JA, et al. ABCB1 gene variants influence tolerance to selective serotonin reuptake inhibitors in a large sample of Dutch cases with major depressive disorder. Pharmacogenomics J. 2013; 13:349–353. PMID:
22641028.

58. Clark SL, Adkins DE, Aberg K, Hettema JM, McClay JL, Souza RP, et al. Pharmacogenomic study of side-effects for antidepressant treatment options in STAR*D. Psychol Med. 2012; 42:1151–1162. PMID:
22041458.

59. Kurose K, Hiratsuka K, Ishiwata K, Nishikawa J, Nonen S, Azuma J, et al. Genome-wide association study of SSRI/SNRI-induced sexual dysfunction in a Japanese cohort with major depression. Psychiatry Res. 2012; 198:424–429. PMID:
22445761.

60. Adkins DE, Clark SL, Åberg K, Hettema JM, Bukszár J, McClay JL, et al. Genome-wide pharmacogenomic study of citalopram-induced side effects in STAR*D. Transl Psychiatry. 2012; 2:e129. PMID:
22760553.

61. Huang YY, Zhang XS, Gao JJ, Gao P, Liang CZ. Association between serotonin transporter 5-HTTLPR and STin2 VNTR polymorphisms and anejaculation: a preliminary report. Asian J Androl. 2017; 19:719–720. PMID:
27586024.

62. Waldinger MD, Berendsen HH, Blok BF, Olivier B, Holstege G. Premature ejaculation and serotonergic antidepressants-induced delayed ejaculation: the involvement of the serotonergic system. Behav Brain Res. 1998; 92:111–118. PMID:
9638953.

63. Waldinger MD, Schweitzer DH. Retarded ejaculation in men: an overview of psychological and neurobiological insights. World J Urol. 2005; 23:76–81. PMID:
15937707.

64. McMahon CG. Premature ejaculation. Indian J Urol. 2007; 23:97–108. PMID:
19675782.

65. Moretti M, Facchini F, Grande M, Larosa M, Leone M, Ziglioli F, et al. Ejaculatory system cysts: a case report. Urologia. 2014; 81(Suppl 23):S32–S37. PMID:
24665031.

66. Taskinen S, Heikkilä J, Santtila P, Rintala R. Posterior urethral valves and adult sexual function. BJU Int. 2012; 110:E392–E396. PMID:
22448709.

67. Reddy SS, Inouye BM, Anele UA, Abdelwahab M, Le B, Gearhart JP, et al. Sexual health outcomes in adults with complete male epispadias. J Urol. 2015; 194:1091–1095. PMID:
25916676.

68. Park W, Zwink N, Rösch WH, Schmiedeke E, Stein R, Schmidt D, et al. Sexual function in adult patients with classic bladder exstrophy: a multicenter study. J Pediatr Urol. 2015; 11:125.e1–125.e6. PMID:
25986209.

69. Frey A, Pedersen C, Lindberg H, Bisbjerg R, Sønksen J, Fode M. Prevalence and predicting factors for commonly neglected sexual side effects to external-beam radiation therapy for prostate cancer. J Sex Med. 2017; 14:558–565. PMID:
28258954.

70. Sullivan JF, Stember DS, Deveci S, Akin-Olugbade Y, Mulhall JP. Ejaculation profiles of men following radiation therapy for prostate cancer. J Sex Med. 2013; 10:1410–1416. PMID:
23433425.

71. Lew-Starowicz M, Rola R. Sexual dysfunctions and sexual quality of life in men with multiple sclerosis. J Sex Med. 2014; 11:1294–1301. PMID:
24612517.
72. Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliott SL. Long-term effects of spinal cord injury on sexual function in men: implications for neuroplasticity. Spinal Cord. 2007; 45:338–348. PMID:
17016492.

73. Lindau ST, Tang H, Gomero A, Vable A, Huang ES, Drum ML, et al. Sexuality among middle-aged and older adults with diagnosed and undiagnosed diabetes: a national, population-based study. Diabetes Care. 2010; 33:2202–2210. PMID:
20802158.
74. Ohl DA, Quallich SA, Sønksen J, Brackett NL, Lynne CM. Anejaculation and retrograde ejaculation. Urol Clin North Am. 2008; 35:211–220. PMID:
18423241.

75. Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol. 2016; 5:549–562. PMID:
27652227.

76. Corona G, Jannini EA, Mannucci E, Fisher AD, Lotti F, Petrone L, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008; 5:1991–1998. PMID:
18399946.

77. Morgentaler A, Polzer P, Althof S, Bolyakov A, Donatucci C, Ni X, et al. Delayed ejaculation and associated complaints: relationship to ejaculation times and serum testosterone levels. J Sex Med. 2017; 14:1116–1124. PMID:
28807505.

78. Nair S, Milsom S. Anejaculation as the presenting feature of pituitary microadenoma. Fertil Steril. 2008; 90:2012.e21–2012.e23.

79. Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005; 90:6472–6479. PMID:
16204360.

80. La Torre A, Giupponi G, Duffy D, Conca A, Cai T, Scardigli A. Sexual dysfunction related to drugs: a critical review. part V: α-blocker and 5-ARI drugs. Pharmacopsychiatry. 2016; 49:3–13. PMID:
26569417.

81. Abdel-Hamid IA, Saleh el-S. Primary lifelong delayed ejaculation: characteristics and response to bupropion. J Sex Med. 2011; 8:1772–1779. PMID:
21114770.

82. Tsimtsiou Z, Hatzimouratidis K, Nakopoulou E, Kyrana E, Salpigidis G, Hatzichristou D. Predictors of physicians' involvement in addressing sexual health issues. J Sex Med. 2006; 3:583–588. PMID:
16839313.
83. Courtois F, Charvier K, Leriche A, Vézina JG, Côté I, Raymond D, et al. Perceived physiological and orgasmic sensations at ejaculation in spinal cord injured men. J Sex Med. 2008; 5:2419–2430. PMID:
18466272.

84. Paduch DA, Polzer PK, Ni X, Basaria S. Testosterone replacement in androgen-deficient men with ejaculatory dysfunction: a randomized controlled trial. J Clin Endocrinol Metab. 2015; 100:2956–2962. PMID:
26158605.

85. Maggi M, Heiselman D, Knorr J, Iyengar S, Paduch DA, Donatucci CF. Impact of testosterone solution 2% on ejaculatory dysfunction in hypogonadal men. J Sex Med. 2016; 13:1220–1226. PMID:
27436077.

86. Masui H, Ike H, Yamaguchi S, Oki S, Shimada H. Male sexual function after autonomic nerve-preserving operation for rectal cancer. Dis Colon Rectum. 1996; 39:1140–1145. PMID:
8831531.

87. Pettus JA, Carver BS, Masterson T, Stasi J, Sheinfeld J. Preservation of ejaculation in patients undergoing nerve-sparing postchemotherapy retroperitoneal lymph node dissection for metastatic testicular cancer. Urology. 2009; 73:328–331. discussion 331-2. PMID:
19022490.

88. Meng X, Fan L, Liu J, Wang T, Yang J, Wang J, et al. Fresh semen quality in ejaculates produced by nocturnal emission in men with idiopathic anejaculation. Fertil Steril. 2013; 100:1248–1252. PMID:
23987518.

89. Soeterik TF, Veenboer PW, Lock TM. Electroejaculation in psychogenic anejaculation. Fertil Steril. 2014; 101:1604–1608. PMID:
24726223.

90. Perelman MA. Sex coaching for physicians: combination treatment for patient and partner. Int J Impot Res. 2003; 15(Suppl 5):S67–S74. PMID:
14551580.

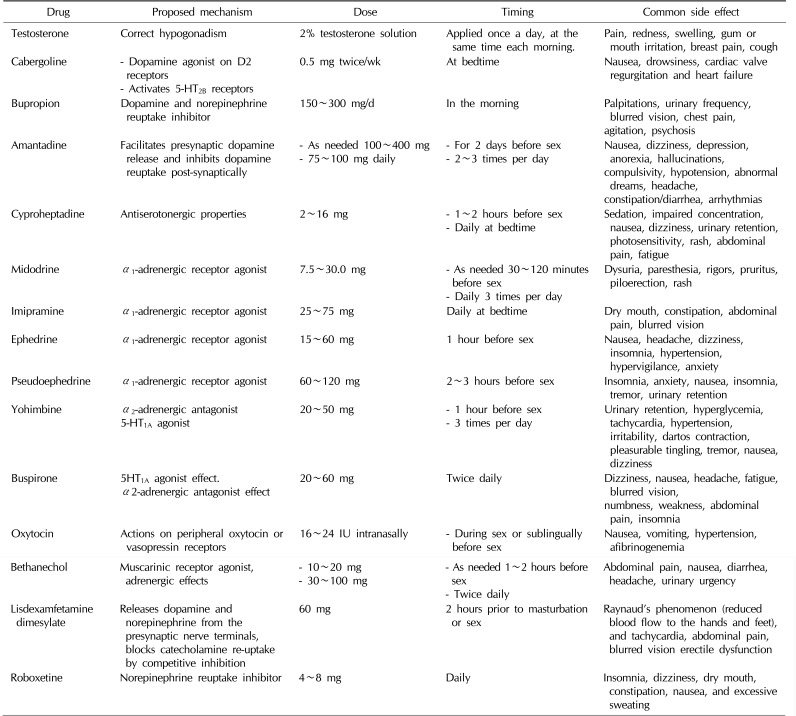
91. Abdel-Hamid IA, Elsaied MA, Mostafa T. The drug treatment of delayed ejaculation. Transl Androl Urol. 2016; 5:576–591. PMID:
27652229.

92. Lyons MD, Lentz AC, Coward RM. Lisdexamfetamine dimesylate (Vyvanse) for the treatment of neurogenic anejaculation. Am J Mens Health. 2017; 11:618–619. PMID:
27402622.

93. Pryor JP. Erectile and ejaculatory problems in infertility. In : Hargreave TB, editor. Male infertility. London: Springer;1997. p. 319–336.
94. Leduc BE, Fournier C, Jacquemin G, Lepage Y, Vinet B, Hétu PO, et al. Midodrine in patients with spinal cord injury and anejaculation: a double-blind randomized placebo-controlled pilot study. J Spinal Cord Med. 2015; 38:57–62. PMID:
24969635.

95. Fahmy I, Kamal A, Metwali M, Rhodes C, Mansour R, Serour G, et al. Vigorous prostatic massage: a simple method to retrieve spermatozoa for intracytoplasmic sperm injection in psychogenic anejaculation: case report. Hum Reprod. 1999; 14:2050–2053. PMID:
10438425.
96. Soler JM, Previnaire JG, Mieusset R. Evidence of a new pattern of ejaculation in men with spinal cord injury: ejaculation dyssynergia and implications for fertility. Spinal Cord. 2016; 54:1210–1214. PMID:
27324318.

97. Castle SM, Jenkins LC, Ibrahim E, Aballa TC, Lynne CM, Brackett NL. Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord. 2014; 52(Suppl 2):S27–S29. PMID:
25082380.

98. Fode M, Ohl DA, Sønksen J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol. 2015; 12:607–616. PMID:
26481575.

99. Raviv G, Madgar I, Elizur S, Zeilig G, Levron J. Testicular sperm retrieval and intra cytoplasmic sperm injection provide favorable outcome in spinal cord injury patients, failing conservative reproductive treatment. Spinal Cord. 2013; 51:642–644. PMID:
23689394.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download