Abstract
Varicoceles are a major cause of impaired spermatogenesis and the most common correctable cause of male infertility. They are found in approximately 40% of men with primary infertility and 80% of men with secondary infertility, although they also occur in 12% of men with normal semen parameters. The presence of a varicocele does not always affect spermatogenesis, as it has been reported that only 20% of men with documented varicoceles suffer fertility problems. However, varicocele repair appears to have beneficial effects in men with impaired semen parameters and palpable varicoceles. Currently, the main procedures employed for varicocele repair are microsurgical subinguinal or inguinal varicocelectomy, laparoscopic varicocelectomy, and radiological percutaneous embolization. Microsurgical varicocelectomy appears to be the optimal treatment in most cases, whereas the other procedures are useful only in specific cases. After treatment, it typically takes 3 to 6 months for patients' semen parameters to improve; thus, other therapies, including assisted reproductive technology, should be considered if infertility persists after this interval, especially in older couples. Controversies still remain regarding how varicoceles in certain subgroups, such as adolescents or men with azoospermia, should be treated. Due to their relatively high prevalence rate among the general population, varicoceles can occur concomitantly with other conditions that cause impaired spermatogenesis. Further studies are necessary in order to identify the patients who are most likely to benefit from treatment. In this review, we sought to summarize the issues currently associated with varicocele treatment in infertile men.
Infertility affects approximately 15% of couples, and male factors are known to be responsible in almost half of cases [1]. Several etiological factors can contribute to male infertility, including impaired spermatogenesis, the obstruction of the passage of sperm, and sexual dysfunction. Varicoceles are a major cause of impaired spermatogenesis and are the most common correctable cause of male infertility [2]. Varicoceles are found in approximately 40% of men with primary infertility and 80% of men with secondary infertility, although they also occur in 12% of men with normal semen parameters [345]. The recognition that varicoceles are associated with male infertility dates back to the first century, when Celsius noted an association between varicoceles and ipsilateral testicular atrophy [6]. In the 19th century, further evidence that varicoceles are associated with impaired testicular function was obtained [78]. Subsequently, Macomber and Sanders [9] noted that surgical varicocelectomy was associated with improved sperm production and fertility. In 1955, Tulloch [10] demonstrated that high ligation of the spermatic vessels resulted in improved fertility, which led to varicoceles being recognized as a major surgically correctable cause of male infertility. Subsequently, numerous studies have reported that varicocele repair is an effective treatment for male infertility.
In 2003, Evers and Collins [11] published a shocking systematic review addressing the topic of varicocele repair for male-factor infertility, concluding that "varicocele repair does not seem to be an effective treatment for male or unexplained subfertility." However, their review included patients with non-palpable varicoceles and/or normal semen parameters, who are not generally offered varicocele repair as a treatment for male infertility [1213]. This is critical because including these men would have masked the beneficial effects of treatment for clinically apparent varicoceles in men with impaired semen parameters. Indeed, several meta-analyses that excluded men with subclinical varicoceles or normal semen parameters have confirmed the efficacy of varicocele treatment [1415]. For example, in a study involving men with palpable varicoceles and abnormal semen parameters conducted by Marmar et al [14], a meta-analysis indicated that the odds ratio of spontaneous pregnancy after surgical varicocelectomy was 2.87. In the updated Cochrane review conducted by Kroese et al [16], the authors concluded that in subfertile men with a clinically evident varicocele and poor semen quality, treatment might be beneficial, as it was found to result in an odds ratio for natural pregnancy of 1.47. Although the evidence is still inconclusive, many andrologists believe that varicocele treatment is effective in men with palpable varicoceles and impaired semen parameters. In this review, we sought to summarize the issues currently associated with varicocele treatment in infertile men.
A varicocele is a varicose vein in the scrotum that arises due to abnormal dilation of the internal spermatic vein and pampiniform venous plexus within the spermatic cord. Most varicoceles occur on the left side; a palpable left-sided varicocele is seen in 85% to 90% of cases, while isolated right-sided varicoceles are extremely rare [1718]. Accordingly, in cases involving an isolated right-sided varicocele, the physician should consider whether the varicocele may be caused by the effects of a retroperitoneal mass [19]. The predominance of left-sided varicoceles is related to the anatomy of the testicular venous drainage system [6]. The left internal spermatic vein is longer and enters the left renal vein at a right angle, whereas the right internal spermatic vein drains directly into the inferior vena cava. This anatomical structure contributes to the high hydrostatic pressure of the left testicular venous drainage system, which was confirmed by a study that detected higher venous pressure levels in the left internal spermatic vein in men with varicoceles [20]. Regurgitation can occur in the internal spermatic vein as a result of the absence of venous valves [21], compression of the left renal vein between the superior mesenteric artery and aorta, or obstruction of the left common iliac vein by the left common iliac artery [22]. Although the precise mechanism has yet to be established, varicoceles can affect spermatogenesis and Leydig cell function by inducing an elevated testicular temperature [23], increased venous pressure [24], hypoxia [25], oxidative stress [26], hormonal imbalances [27], and/or the reflux of toxic metabolites of adrenal or renal origin [28]. However, it is important to note that the presence of a varicocele does not always result in impaired spermatogenesis. Only 20% of men with documented varicoceles have been reported to suffer fertility problems [2930].
As described above, the presence of a varicocele does not always result in fertility problems. A number of men with varicoceles do not show any evidence of testicular dysfunction, although varicoceles do affect spermatogenesis in a subset of patients. Consequently, the indications for varicocele treatment should be determined carefully in order to avoid unnecessary invasive interventions. The American Society for Reproductive Medicine (ASRM) Practice Committee guidelines indicate that varicocele treatment should be considered when most or all of the following conditions are met: (1) the couple is attempting to conceive; (2) the varicocele is palpable on physical examination; (3) the couple has known fertility problems; (4) the female partner has normal fertility or a potentially treatable cause of infertility, and the time until conception is not a concern; and (5) the male partner has abnormal semen parameters [12]. However, it should be noted that varicoceles can have a progressively toxic effect on the testes, ultimately resulting in irreversible infertility if left untreated [2]. Even if no abnormalities in testicular function are detected during the evaluation of a patient with a varicocele, regular follow-up is recommended if the patient is concerned about his future fertility [2].
The goal of varicocele treatment is to eliminate venous reflux into the scrotum while preserving the internal spermatic artery, lymphatic vessels, and vas deferens. Two approaches can be used to accomplish this goal: surgical varicocelectomy and percutaneous embolization, the former of which is widely employed.
Several approaches have been used in the surgical treatment of varicoceles. In the early 20th century, Ivanissevich [31] proposed a suprainguinal approach to spermatic vein ligation, which involved only ligating the spermatic vein while preserving the artery. More than 4,000 cases in which this procedure was performed have been reported in the literature. Bernardi [32], a student of Ivanissevich, modified this procedure to include a transinguinal approach, which is an easier way of accessing the spermatic cord than the retroperitoneal approach. This transinguinal procedure is usually described as the "Ivanissevich method" in the literature [33]. In another surgical procedure developed by Palomo [34], a 3-cm skin incision is made above the internal ring, and then both the spermatic vein and artery are ligated at a more proximal level. This retroperitoneal approach is based on the finding that the deferential and cremasteric arteries provide sufficient blood supply to the testis. Several modified versions of these procedures have been developed. In the 1970s, surgical varicocelectomy gained worldwide interest as a treatment for male infertility [35]. More recently, innovative surgical procedures, including microsurgical and laparoscopic techniques, have been developed.
The most common complications of conventional varicocelectomy are postoperative hydrocele formation and varicocele recurrence [363738]. Furthermore, ligation of the spermatic artery can have a negative impact on testicular function [3940]. The introduction of microsurgical treatment for varicoceles has made it easier to identify and ligate the spermatic veins and to preserve the spermatic arteries and lymphatic vessels [3841]. It is reasonable to suppose that the accurate identification of fine anatomical structures during surgery leads to better treatment outcomes. In agreement with this, a meta-analysis has shown microsurgical varicocelectomy to result in higher pregnancy rates and fewer postoperative complications than conventional varicocelectomy in infertile men [42].
In 1985, Marmar et al [38] presented the first microsurgical varicocelectomy procedure, which was performed with an operating microscope and microsurgical instruments. The procedure was carried out on 71 infertile men with varicoceles and involved a combination of the microdissection of larger veins (>2 mm) and the controlled sclerosis of small veins. The spermatic cord was delivered at the subinguinal level. The microscope was used to ensure that the lymphatics of the spermatic cord were avoided in order to prevent postoperative hydrocele, and a Doppler ultrasound probe and papaverine hydrochloride were employed to identify the internal spermatic arteries when they were in spasm. All of the larger spermatic veins were identified and ligated microsurgically, while the small veins were subjected to sclerosis using sodium tetradecyl sulfate. The operations were completed within 30 minutes, and significant postoperative increases in sperm density and motility were observed. The postoperative pregnancy rate was almost 30% [38]. The same research group updated the outcomes of 606 subfertile men who underwent the abovementioned procedure and reported that the 1-year pregnancy rate was higher in the post-varicocelectomy group than in the medically treated group (35.6% versus 15.8%). In addition, minimal morbidity was observed, including only one case of permanent hydrocele, and the recurrence rate was 0.82% [43]. Numerous microsurgical procedures derived from this procedure have subsequently been developed, although sclerosing agents are rarely used during surgical varicocelectomy.
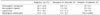
The subinguinal approach results in less morbidity because it preserves the muscle layers and the inguinal canal; however, it is also technically challenging due to the greater number of spermatic veins and arteries located below the external inguinal ring [44]. A study evaluating the microanatomy of the spermatic cord during microsurgical varicocele treatment reported that the primary branching point of the testicular artery was often located in the section that passed through the inguinal canal and that the internal spermatic arteries at the subinguinal level were more than 3 times as likely to be surrounded by a network of adherent veins than those located at the inguinal level (Fig. 1) [45]. Another concern about the subinguinal approach is that the identification of artery pulsation can be difficult due to arterial compression caused by the edge of the external ring pressing against the elevated cord [46].
For these reasons, microsurgical inguinal varicocelectomy has been widely performed for varicocele ligation. In the inguinal approach, an incision measuring 3~5 cm is made over the inguinal canal, and then the external oblique aponeurosis is opened to deliver the spermatic cord. Similarly to the subinguinal approach, all of the internal spermatic veins are identified and ligated under microscopy, and the testicular artery and lymphatics are preserved [41]. Several articles have argued that microsurgical inguinal varicocelectomy is the treatment of choice because this approach produces similar outcomes to the subinguinal approach via a simple surgical technique [474849]. One drawback of this approach is that it results in greater intraoperative pain when performed under local anesthesia. In particular, Gontero et al [49] reported that the inguinal approach resulted in significantly higher intraoperative visual analog scale pain scores.
Although the above techniques usually allow maximal ligation of the spermatic vessels, it should be noted that avenues of testicular venous drainage, such as the gubernacular veins, might persist. To eliminate such channels, the delivery of the testis via a subinguinal or inguinal incision during microsurgery was proposed [41]. Enlarged gubernacular veins were reported to be present in 48% of cases [50], and gubernacular collaterals were presumed to exist in 7% of cases recurrent varicoceles [51]. However, the latter study did not confirm the advantages of testicular delivery during varicocelectomy. Ramasamy and Schlegel [52] reported that delivery of the testis resulted in more trauma, a longer operating time, and inflammatory changes in the scrotum, and it did not have any beneficial effects on semen quality or pregnancy rates after microsurgical varicocelectomy.
Laparoscopic varicocelectomy is essentially the same as the above retroperitoneal procedure (the Palomo method). An early study showed that laparoscopic cameras can provide a microscopic view and that it is easy to identify arteries and to divide and clip the internal spermatic veins during laparoscopic varicocelectomy [53]. However, this procedure is less commonly used to treat varicocele in adults because it generally involves ligation of the testicular artery, which can lead to impaired testicular function [54]. Interestingly, pediatric urologists prefer laparoscopic varicocelectomy to microsurgery [55]. One of the reasons for this might simply be the individual preferences of the surgeons; for example, pediatric urologists may be more familiar with laparoscopic techniques, whereas andrologists are more comfortable with microsurgical techniques [5657]. Although some controversy remains, artery preservation is generally encouraged during laparoscopic procedures, although it may be associated with a higher recurrence rate. A study comparing 122 laparoscopic varicocelectomies with or without artery sparing showed that postoperative sperm density significantly improved when the artery was preserved [58]. Although they are rare, clinicians should be aware that laparoscopic varicocelectomy is associated with various inherent complications, such as air embolism, hypercapnia, injuries to the intra-abdominal organs, port-site hernias, and delayed bowel obstruction due to adhesion [56]. At the same time, this approach has advantages for the simultaneous repair of bilateral varicoceles [59].
Percutaneous embolization of the internal spermatic vein is a non-surgical approach that results in minimal pain and allows the patient to recover rapidly after the procedure. Spermatic venography was introduced as a diagnostic tool that can be used to select patients who would be good candidates for surgical varicocelectomy [60]. The first percutaneous embolization procedure was described by Lima et al [61] in 1978. The authors reported the feasibility of interrupting retrograde flow in the spermatic veins using by sclerosing agents, and this did not result in any significant prolongation of the diagnostic procedure. While this procedure was initially performed via a transfemoral approach, a transjugular approach can also be used to gain better access to spermatic veins that are technically difficult to identify, such as the right spermatic veins [6263]. In addition, several modifications to the procedure, including the use of balloon occlusion and coil embolization, have been made over the years [64]. This approach has the following advantages: it does not require surgical incisions; it makes it possible to identify all testicular veins, including the collateral veins; and virtually eliminates damage to the testicular artery. However, catheterization of the spermatic vein may be technically impossible in certain cases [6566]. In addition, although such complications are rare, embolization carries a risk of contrast reactions, extravasation, and migration of the embolization material [6768]. This procedure is less commonly used as a first-line treatment for varicoceles, but it has been found to exhibit an excellent success rate in the setting of recurrent varicoceles after surgical repair [69].
As described above, microsurgical varicocelectomy, laparoscopic varicocelectomy, and percutaneous embolization are the main treatment options for varicoceles in infertile men. The main goal of treatment is to eliminate venous backflow without causing postoperative complications, such as hydrocele. Although none of these methods has been proven to be superior to the others in terms of their ability to improve fertility [12], numerous studies have evaluated the clinical outcomes of these procedures, and microsurgical procedures seem to produce more favorable outcomes than other techniques. A meta-analysis by Cayan et al [42] evaluated the cases of 4,473 infertile men with palpable varicoceles and showed that microsurgical varicocelectomy techniques were associated with higher spontaneous pregnancy rates and lower complication rates. Another review by Diegidio et al [70] that included over 5,000 patients concluded that microsurgical subinguinal or inguinal techniques offer the best outcomes (Table 1). Similar results were also described in a recent review article [71]. Kovac et al [72] examined the cost-effectiveness of varicocele treatment and found that microsurgical varicocelectomy was the most cost-effective method of treatment based on pregnancy outcomes. Collectively, microsurgical subinguinal or inguinal varicocelectomy might be the optimal treatment in most cases. However, laparoscopic surgery might be preferred in some cases, such as those involving bilateral varicoceles. Percutaneous embolization is rarely employed as a first-line treatment for varicoceles, but it is an ideal choice for men in whom varicocele recurs after surgery.
From a practical viewpoint, assessing how soon improvements in semen parameters are seen after varicocele repair is important, especially in older couples. In humans, the entire spermatogenic process takes approximately 64 days [73]. Studies evaluating the time interval between varicocelectomy and improvements in semen parameters revealed that sperm parameters improved during the first 3 months after varicocele repair, but did not show further improvements thereafter [7475]. Correspondingly, the ASRM Practice Committee has stated that improvements in semen parameters are typically seen after 3 to 6 months [12]. These findings are useful for designing therapeutic strategies for candidates for varicocelectomy and underscore the necessity of not delaying other approaches for managing infertility.
Although they are rarely seen in pre-pubertal boys, most varicoceles are present by the time puberty is completed [76]. The management of varicoceles in adolescents is more complicated. Since many men with varicoceles do not suffer from fertility problems, it is obvious that repairing all varicoceles would represent overtreatment. However, in a proportion of adolescents, the presence of a varicocele has detrimental effects on testicular growth and can lead to irreversible testicular damage [77]. Thus, it is important to identify appropriate candidates for treatment. The most widely accepted indication for varicocele treatment in adolescents is a marked discrepancy in testicular volume (a >20% discrepancy in testicular volume is usually considered to be significant). However, no consensus currently exists regarding who should be treated, when they should be treated, or how they should be treated [17].
In the first report of a varicocele in a man with azoospermia, Tulloch [78] described the case of an azoospermic male with a varicocele in whom sperm returned to the ejaculate after varicocelectomy. Subsequently, several articles have indicated that surgical varicocelectomy is effective in men with non-obstructive azoospermia (NOA) [7980]. However, whether men with NOA should be offered treatment for clinically apparent varicoceles remains controversial. Schlegel and Kaufmann [81] reported that even if return of sperm to the ejaculate was achieved after varicocelectomy in men with NOA, <10% of the patients had adequately motile sperm for assisted reproductive technology. In addition, although their study included men with NOA and subclinical varicoceles, a history of prior varicocele repair did not increase the likelihood of sperm retrieval when testicular sperm retrieval (testicular sperm extraction, TESE) was performed. In contrast, subsequent studies have shown varicocele treatment to be effective in men with NOA [8283]. Recently, Esteves et al [84] conducted a systematic review evaluating the outcomes of varicocele repair in men with NOA. Their study included 468 men with NOA and palpable varicoceles and reported that the sperm retrieval rate was significantly higher in men who had previously undergone varicocele repair (odds ratio=2.65). In addition, sufficient return of sperm to the ejaculate to avoid TESE was observed in approximately 44% of the treated men. Furthermore, of the men whose postoperative ejaculate contained sperm, 14% subsequently achieved natural pregnancies. Taken together, although in men with NOA, varicocelectomy may be an unnecessary treatment that delays the performance of a definitive intracytoplasmic sperm injection procedure, a subset of men might benefit from such treatment. Thus, clinicians should counsel couples with care. Since varicoceles can occur coincidentally in men with NOA, it is essential to rule out other factors that can contribute to spermatogenic disruption, such as abnormalities of the sex chromosomes or Y chromosome microdeletions, before considering varicocele repair in these patients.
Varicoceles are a common and correctable cause of male infertility. Although varicocele repair has been shown to be an effective treatment for male infertility, some men who undergo this procedure fail to exhibit any postoperative improvement in spermatogenesis. One possible reason for this is that it is difficult to identify the patients who would benefit most from varicocele repair. According to the current guidelines, varicocele repair is only recommended for men who want to improve their fertility, have a palpable varicocele, and exhibit abnormal semen parameters. Considering their relatively high prevalence among the general population, varicoceles can occur concomitantly with other idiopathic conditions. Further studies are needed to identify the patients who are most likely to benefit from varicocele repair.
The varicocele repair procedures used to treat infertility include microscopic subinguinal or inguinal varicocelectomy, laparoscopic varicocelectomy, and radiological percutaneous embolization. Of these, microsurgical varicocelectomy is the most commonly employed and achieves favorable outcomes. However, controversies still remain regarding the optimal treatment for certain cases, such as adolescents or men with azoospermia.
Figures and Tables
Fig. 1
Schematic diagram of the microanatomy of the spermatic cord. The numbers denote the mean quantity of arteries (red) and veins (blue) at the indicated level. The primary branching point of the testicular artery is often located along the section that passes through the inguinal canal. Internal spermatic veins become substantially less numerous moving from the subinguinal region through the inguinal canal to the internal inguinal ring. Data from the article of Hopps et al (J Urol 2003;170:2366-70) [45] with original copyright holder's permission.

References
1. Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod. 1991; 6:811–816.
2. Cozzolino DJ, Lipshultz LI. Varicocele as a progressive lesion: positive effect of varicocele repair. Hum Reprod Update. 2001; 7:55–58.

3. Dubin L, Amelar RD. Etiologic factors in 1294 consecutive cases of male infertility. Fertil Steril. 1971; 22:469–474.

4. Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993; 59:613–616.
5. World Health Organization. The influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinics. Fertil Steril. 1992; 57:1289–1293.
6. Kaufman DG, Nagler HM. The varicocele: concepts of pathophysiology: present and future. World J Urol. 1986; 4:88–91.
7. Bennet WH. Varicocele, particularly with reference to its radical cure. Lancet. 1889; 1:261.
8. Curling TB. A practical treatise on the disease of the testis and of the spermatic cord and scrotum. Philadelphia: Blanchard & Lea;1856.
9. Macomber D, Sanders MB. The spermatozoa count: its value in the diagnosis, prognosis and treatment of sterility. New Engl J Med. 1929; 200:981–984.
11. Evers JL, Collins JA. Assessment of efficacy of varicocele repair for male subfertility: a systematic review. Lancet. 2003; 361:1849–1852.

12. Practice Committee of the American Society for Reproductive Medicine. Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014; 102:1556–1560.
13. Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, et al. European association of urology guidelines on male infertility: the 2012 update. Eur Urol. 2012; 62:324–332.

14. Marmar JL, Agarwal A, Prabakaran S, Agarwal R, Short RA, Benoff S, et al. Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysis. Fertil Steril. 2007; 88:639–648.

15. Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, Salonia A, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011; 60:796–808.

16. Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012; 10:CD000479.

17. Chiba K, Ramasamy R, Lamb DJ, Lipshultz LI. The varicocele: diagnostic dilemmas, therapeutic challenges and future perspectives. Asian J Androl. 2016; 18:276–281.

18. Skoog SJ, Roberts KP, Goldstein M, Pryor JL. The adolescent varicocele: what's new with an old problem in young patients? Pediatrics. 1997; 100:112–121.

19. Masson P, Brannigan RE. The varicocele. Urol Clin North Am. 2014; 41:129–144.
20. Shafik A, Bedeir GA. Venous tension patterns in cord veins I In normal and varicocele individuals. J Urol. 1980; 123:383–385.

21. Ahlberg NE, Bartley O, Chidekel N. Right and left gonadal veins An anatomical and statistical study. Acta Radiol Diagn (Stockh). 1966; 4:593–601.
22. Coolsaet BL. The varicocele syndrome: venography determining the optimal level for surgical management. J Urol. 1980; 124:833–839.

23. Garolla A, Torino M, Miola P, Caretta N, Pizzol D, Menegazzo M, et al. Twenty-four-hour monitoring of scrotal temperature in obese men and men with a varicocele as a mirror of spermatogenic function. Hum Reprod. 2015; 30:1006–1013.

24. Eisenberg ML, Lipshultz LI. Varicocele-induced infertility: Newer insights into its pathophysiology. Indian J Urol. 2011; 27:58–64.

25. Hu W, Zhou PH, Zhang XB, Xu CG, Wang W. Roles of adrenomedullin and hypoxia-inducible factor 1 alpha in patients with varicocele. Andrologia. 2015; 47:951–957.

26. Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol. 2008; 59:2–11.
27. Rajfer J, Turner TT, Rivera F, Howards SS, Sikka SC. Inhibition of testicular testosterone biosynthesis following experimental varicocele in rats. Biol Reprod. 1987; 36:933–937.

28. Fujisawa M, Yoshida S, Kojima K, Kamidono S. Biochemical changes in testicular varicocele. Arch Androl. 1989; 22:149–159.

29. Diamond DA, Gargollo PC, Caldamone AA. Current management principles for adolescent varicocele. Fertil Steril. 2011; 96:1294–1298.

30. Robinson SP, Hampton LJ, Koo HP. Treatment strategy for the adolescent varicocele. Urol Clin North Am. 2010; 37:269–278.

31. Ivanissevich O. Left varicocele due to reflux; experience with 4,470 operative cases in forty-two years. J Int Coll Surg. 1960; 34:742–755.
32. Bernardi R. Ivanissevich's anatomical concept of the cure of varicocele: some modifications in its technique. Bol Inst Clin Quir. 1941; 13:521.
33. González R. Proposal for describing procedures to correct varicocele. A new terminology. Front Pediatr. 2014; 2:47.

34. Palomo A. Radical cure of varicocele by a new technique; preliminary report. J Urol. 1949; 61:604–607.

35. Marmar JL. The evolution and refinements of varicocele surgery. Asian J Androl. 2016; 18:171–178.

36. Dubin L, Amelar RD. Varicocelectomy: 986 cases in a twelve-year study. Urology. 1977; 10:446–449.

37. Szabo R, Kessler R. Hydrocele following internal spermatic vein ligation: a retrospective study and review of the literature. J Urol. 1984; 132:924–925.

38. Marmar JL, DeBenedictis TJ, Praiss D. The management of varicoceles by microdissection of the spermatic cord at the external inguinal ring. Fertil Steril. 1985; 43:583–588.

39. Steinberger E, Tjioe DY. Spermatogenesis in rat testes after experimental ischemia. Fertil Steril. 1969; 20:639–649.

41. Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992; 148:1808–1811.

42. Cayan S, Shavakhabov S, Kadioğlu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009; 30:33–40.

43. Marmar JL, Kim Y. Subinguinal microsurgical varicocelectomy: a technical critique and statistical analysis of semen and pregnancy data. J Urol. 1994; 152:1127–1132.

44. Kupis Ł, Dobroński PA, Radziszewski P. Varicocele as a source of male infertility: current treatment techniques. Cent European J Urol. 2015; 68:365–370.

45. Hopps CV, Lemer ML, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approach. J Urol. 2003; 170:2366–2370.

46. Goldstein M. Surgical management of male infertility and other scrotal disorders. In : Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Campbell's urology. 8th ed. Philadelphia: W.B. Saunders;2002. p. 1573–1574.
47. Orhan I, Onur R, Semerciöz A, Firdolas F, Ardicoglu A, Köksal IT. Comparison of two different microsurgical methods in the treatment of varicocele. Arch Androl. 2005; 51:213–220.

48. Binsaleh S, Lo KC. Varicocelectomy: microsurgical inguinal varicocelectomy is the treatment of choice. Can Urol Assoc J. 2007; 1:277–278.
49. Gontero P, Pretti G, Fontana F, Zitella A, Marchioro G, Frea B. Inguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia: which technique is preferable in clinical practice? Urology. 2005; 66:1075–1079.

50. Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992; 148:1190–1194.

51. Murray RR Jr, Mitchell SE, Kadir S, Kaufman SL, Chang R, Kinnison ML, et al. Comparison of recurrent varicocele anatomy following surgery and percutaneous balloon occlusion. J Urol. 1986; 135:286–289.

52. Ramasamy R, Schlegel PN. Microsurgical inguinal varicocelectomy with and without testicular delivery. Urology. 2006; 68:1323–1326.

53. Hagood PG, Mehan DJ, Worischeck JH, Andrus CH, Parra RO. Laparoscopic varicocelectomy: preliminary report of a new technique. J Urol. 1992; 147:73–76.

54. Lipshultz LI, Thomas AJ Jr, Khera M. Surgical management of male infertility. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: WB Saunders;2007. p. 654–717.
55. Pastuszak AW, Kumar V, Shah A, Roth DR. Diagnostic and management approaches to pediatric and adolescent varicocele: a survey of pediatric urologists. Urology. 2014; 84:450–455.

56. Fine RG, Franco I. Laparoscopic orchiopexy and varicocelectomy: is there really an advantage? Urol Clin North Am. 2015; 42:19–29.
57. Diamond D. Adolescent versus adult varicoceles: how do evaluation and management differ? J Urol. 2009; 181:2418–2419.
58. Zampieri N, Zuin V, Corroppolo M, Chironi C, Cervellione RM, Camoglio FS. Varicocele and adolescents: semen quality after 2 different laparoscopic procedures. J Androl. 2007; 28:727–733.

59. Borruto FA, Impellizzeri P, Antonuccio P, Finocchiaro A, Scalfari G, Arena F, et al. Laparoscopic vs open varicocelectomy in children and adolescents: review of the recent literature and meta-analysis. J Pediatr Surg. 2010; 45:2464–2469.

60. Sabatier JC, Bruneton JN, Drouillard J, Tavernier J, Ducos M, Fleury B, et al. Spermatic phlebography: techniques and indications. A study on 37 cases (author's transl). Ann Radiol (Paris). 1977; 20:539–544.
61. Lima SS, Castro MP, Costa OF. A new method for the treatment of varicocele. Andrologia. 1978; 10:103–106.

62. Gonzalez R, Narayan P, Formanek A, Amplatz K. Transvenous embolization of internal spermatic veins: nonoperative approach to treatment of varicocele. Urology. 1981; 17:246–248.

63. Formanek A, Rusnak B, Zollikofer C, Castaneda-Zuniga WR, Narayan P, Gonzalez R, et al. Embolization of the spermatic vein for treatment of infertility: a new approach. Radiology. 1981; 139:315–321.

64. Halpern J, Mittal S, Pereira K, Bhatia S, Ramasamy R. Percutaneous embolization of varicocele: technique, indications, relative contraindications, and complications. Asian J Androl. 2016; 18:234–238.

65. Fayad F, Sellier N, Chabaud M, Kazandjian V, Larroquet M, Raquillet C, et al. Percutaneous retrograde endovascular occlusion for pediatric varicocele. J Pediatr Surg. 2011; 46:525–529.

66. Storm DW, Hogan MJ, Jayanthi VR. Initial experience with percutaneous selective embolization: a truly minimally invasive treatment of the adolescent varicocele with no risk of hydrocele development. J Pediatr Urol. 2010; 6:567–571.

67. Chomyn JJ, Craven WM, Groves BM, Durham JD. Percutaneous removal of a Gianturco coil from the pulmonary artery with use of flexible intravascular forceps. J Vasc Interv Radiol. 1991; 2:105–106.

68. Vicini P, Di Pierro GB, Grande P, Voria G, Antonini G, De Marco F, et al. Large bowel infarct following antegrade scrotal sclerotherapy for varicocele: a case report. Can Urol Assoc J. 2014; 8:E641–E643.

69. Jargiello T, Drelich-Zbroja A, Falkowski A, Sojka M, Pyra K, Szczerbo-Trojanowska M. Endovascular transcatheter embolization of recurrent postsurgical varicocele: anatomic reasons for surgical failure. Acta Radiol. 2015; 56:63–69.

70. Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011; 108:1157–1172.

71. Wang J, Xia SJ, Liu ZH, Tao L, Ge JF, Xu CM, et al. Inguinal and subinguinal micro-varicocelectomy, the optimal surgical management of varicocele: a meta-analysis. Asian J Androl. 2015; 17:74–80.

72. Kovac JR, Fantus J, Lipshultz LI, Fischer MA, Klinghoffer Z. Cost-effectiveness analysis reveals microsurgical varicocele repair is superior to percutaneous embolization in the treatment of male infertility. Can Urol Assoc J. 2014; 8:E619–E625.

73. Schlegel PN, Hardy MP, Goldstein M. Male reproductive physiology. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders;2007. p. 577–608.
74. Al Bakri A, Lo K, Grober E, Cassidy D, Cardoso JP, Jarvi K. Time for improvement in semen parameters after varicocelectomy. J Urol. 2012; 187:227–231.

75. Fukuda T, Miyake H, Enatsu N, Matsushita K, Fujisawa M. Assessment of time-dependent changes in semen parameters in infertile men after microsurgical varicocelectomy. Urology. 2015; 86:48–51.

76. Steeno O, Knops J, Declerck L, Adimoelja A, van de Voorde H. Prevention of fertility disorders by detection and treatment of varicocele at school and college age. Andrologia. 1976; 8:47–53.

78. Tulloch WS. A consideration of sterility factors in the light of subsequent pregnancies. II. Sub fertility in the male (Tr. Edinburgh Obst. Soc. Session 104). Edinb Med J. 1951; 59:29–34.
79. Czaplicki M, Bablok L, Janczewski Z. Varicocelectomy in patients with azoospermia. Arch Androl. 1979; 3:51–55.

80. Matthews GJ, Matthews ED, Goldstein M. Induction of spermatogenesis and achievement of pregnancy after microsurgical varicocelectomy in men with azoospermia and severe oligoasthenospermia. Fertil Steril. 1998; 70:71–75.

81. Schlegel PN, Kaufmann J. Role of varicocelectomy in men with nonobstructive azoospermia. Fertil Steril. 2004; 81:1585–1588.

82. Inci K, Hascicek M, Kara O, Dikmen AV, Gürgan T, Ergen A. Sperm retrieval and intracytoplasmic sperm injection in men with nonobstructive azoospermia, and treated and untreated varicocele. J Urol. 2009; 182:1500–1505.

83. Haydardedeoglu B, Turunc T, Kilicdag EB, Gul U, Bagis T. The effect of prior varicocelectomy in patients with nonobstructive azoospermia on intracytoplasmic sperm injection outcomes: a retrospective pilot study. Urology. 2010; 75:83–86.

84. Esteves SC, Miyaoka R, Roque M, Agarwal A. Outcome of varicocele repair in men with nonobstructive azoospermia: systematic review and meta-analysis. Asian J Androl. 2016; 18:246–253.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download