Abstract
Background
Human rhinoviruses are the major cause of asthma exacerbation in both children and adults. Recently, impaired antiviral interferon (IFN) response in asthmatics has been indicated as a primary reason of the susceptibility to respiratory virus, but the mechanism of defective IFN production is little understood to date. The expression of IFN regulatory factor 7 (IRF7), a transcriptional factor for virus-induced type I IFN production is known to be regulated epigenetically by DNA methylation.
Objective
We aimed to investigate the expression of IFN-α, IFN-β, and IRF7 in response to rhinovirus infection in the adult asthmatics and evaluate DNA methylation status of IRF7 gene promotor.
Methods
Twenty symptomatic adult asthmatics and 10 healthy subjects were enrolled and peripheral blood was collected from each subject. Peripheral blood mononuclear cells (PBMCs) were isolated, cultured, and ex vivo stimulated with rhinovirus-16. The mRNA expressions of IFN-α, IFN-β, and IRF7 were analyzed using real time quantitative polymerase chain reaction. Genomic DNA was isolated from untreated PBMCs and the methylation status of IRF7 gene promotor was investigated using bisulfite pyrosequencing.
Results
The mean age of asthmatics was 45.4 ± 15.7 years and 40% was male, which were not different with those of control group. Asthmatics showed significantly decreased mRNA expressions (relative expression to beta-actin) of IFN-α and IFN-β compared with normal control. The mRNA expression of IRF7 in the asthmatics was also significantly lower than those in the normal control. No significant difference of DNA methylation was observed between asthmatics and controls in all analyzed positions of IRF7 promotor CpG loci.
Asthma is a chronic inflammatory disease with great socioeconomic burden [1]. Despite the advance of asthma management, many patients with asthma still experience episodic worsening of their symptoms. Exacerbation imposes considerable morbidity on patients with asthma and accounts for a major burden on health care resources [2]. In the real world survey of asthma control, 70% of patients with uncontrolled asthma had an unscheduled physician's office visit, 36% had an emergency department visit, and 14% had a hospitalization in a year. Even patients with controlled asthma, 43% had an unscheduled physician's office visit, 10% had an emergency department visit, and 3% had a hospitalization in a year [3]. Direct cost of health care use and indirect cost associated with loss of productivity are considerable due to asthma exacerbation [2].
Asthma exacerbation occurs not only due to inadequate asthma control but also in response to external triggering factors [2, 4]. Viruses are identified as a common external causative agent found in 50% to 90% of asthma exacerbations in children and adults [4]. Of the respiratory tract viruses, human rhinoviruses were most commonly detected approximately 65% of the time [2, 4, 5]. Respiratory tract virus infections cause a great degree of morbidity in the patients with asthma than in the healthy subjects [4, 5]. Increase in the airway hyperresponsiveness and decrease in the lung function were demonstrated in the asthmatics without any change in the healthy subjects after respiratory tract virus infection [6]. Defective innate immune response to the virus in asthmatics has been pointed out as a primary reason of the susceptibility to virus [4]. Impaired types I and III interferon (IFN) production have been reported in airway epithelial cells, bronchoalveolar lavage cells, and peripheral blood cells in asthmatics [7, 8, 9, 10]. However, the mechanism of deficient production of IFN in asthmatic is little known to date. Genetic polymorphism in IFN genes or genes encoding transcriptional factor or signaling molecules might be a mechanistic reason, but has been rarely identified as a genetic factor of asthma in the previous genetic association studies [11]. Recent studies suggested that epigenetic regulation which changes gene expression in the absence of alteration in DNA sequence may in part mediate a complex gene-environment interaction that can lead to asthma [12]. Among the genes regulating type I IFN production, interferon regulatory factor 7 (IRF7) was identified as a direct transducer of virus mediated signaling and shown to play a critical role in the induction of type I IFN genes [13]. Hypermethylation of CpG island on IRF7 promotor gene was related to gene silencing [14, 15]. Furthermore reduced expression of IRF7 in nasal epithelial cell was recently reported as a cause of susceptibility to influenza virus in smoker, which was mediated by hypermethylation of IRF7 gene [16]. In this study, we investigated the expression of IFN-α, IFN-β, and IRF7 in response to rhinovirus in the adults asthmatics and evaluate DNA methylation status of IRF7 gene promotor.
A total of 20 asthmatic patients were enrolled to the study. The criteria of eligibility for the enrollment were as followings; (1) presence of persistent characteristic asthma symptoms and physician's diagnosis of asthma; (2) airway reversibility documented by an increase of forced expiratory volume in one second (FEV1) of 12% and 200 mL after inhalation of 200 µg of salbutamol, or airway hyperresponsiveness documented by a methacholine provocation concentration causing a 20% fall in FEV1 (PC20) of ≤16 mg/mL, in the past or at the time of enrollment; (3) absence of acute asthma exacerbation and respiratory infection within the last 4 weeks prior to enrollment. Ten age/gender-matched healthy subjects were also recruited for the control. All subjects were provided written informed consent, and the study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1205-155-002).
Total 16 mL of peripheral blood was collected from each subject using Vacutainer CPT (Cell Preparation Tube; BD, Franklin Lakes, NJ USA) containing Sodium Citrate as the anticoagulant. The collected bloods were processed according to the manufacturer's instructions, by centrifugation at 1,600 RCF (relative centrifugal force) for 20 minutes at room temperature within two hours of blood collection. PBMC were washed twice with phosphate buffered saline and counted for recovery and viability using 0.4% Trypan Blue (Sigma-Aldrich Co., St. Louis, MO, USA). Aliquots of PBMC collected were cryopreserved using a consensus cryopreservation protocol for the subsequent experiments [17].
PBMCs were cultured in 24-well plates at a cell density of 1×106/mL in RPMI (Roswell Park Memorial Institute)-1640 medium (Gibco, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (Sigma-Aldrich Co.) and infected with a major group rhinovirus, rhinovirus-16 (multiplicity of infection, 1). Rhinovirus-16 was grown in Ohio Hela cells (European Collection of Cell Cultures) and stocks were generated and titrated [10]. As a negative control, cells were treated with medium alone. Cells and supernatants were harvested at 12 hours after rhinovirus stimulation.
RNA was extracted from the control and rhinovirus-treated PBMCs using TRIzol Reagent (Ambion, Carlsbad, CA, USA) for the measurement of mRNA expressions. RNA 1 µg was converted into cDNA using oligo (dT) and revere transcription enzyme (M-MLV, Promega Co., Madison, WI, USA). Expression of mRNA was measured using ABI 7,500 real-time polymerase chain reaction system (Applied Biosystems, Foster, CA, USA) with cDNA, primer solution, and SYBR Green master mix (Applied Biosystems). Primer sequences of each gene used in the experiment were as follows: IFN-α, forward-5'CTGGCACAAATGGGAAGAAT, reverse-5'CTTGAGCCTTCTGGAACTGG; IFN-β, forward-5'CGCCGCATTGACCATCTA, reverse-5'GACATTAGCCAGGAGGTTCT; IRF7, forward-5'TCCCCACGCTATACCATCTACCT, reverse-5'-ACAGCCAGGGT TCCAGCT T. Beta-actin, forward-5'CAAGAGATGGCCACCGCTGCT, reverse-5'TCCTTCTGCATCCTGTCGGCA.
Both IFN-α and IFN-β were assayed using commercial enzyme-linked immunosorbent assay (ELISA) kit (PBL Assay Science, Piscataway, NJ, USA) according to the manufacturer's instructions. The limits of detection were 12.5 pg/mL for IFN-α and 50 pg/mL for IFN-β.
Genomic DNA was isolated from rhinovirus-untreated baseline PBMCs using QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA, USA) according to manufacturer's instruction. Bisulfite modification was carried out with 500 ng DNA using EZ-DNA methylation Kit (Zymo research, Orange, CA, USA). Methylation status of IRF7 gene was investigated using bisulfite pyrosequencing, highly quantitative and reproducible method. We consulted National Center for Biotechnology Information gene browser to get RefSeq summary of human IRF7 gene (NM_004029.2). Detailed annotation was obtained and we examined methylation status of IRF7 gene promotor CpG sites. Bisulfite pyrosequencing was carried out using PSQ 96 MA system and pyrogram was generated for each sample. The percent of methylation were calculated from the peak heights of sequential C and T incorporations. Primers used for amplication and pyrosequencing are listed in Table 1.
Mann-Whitney test was used to compare the expression of IFN-α, IFN-β, and IRF7 and the methylation status of IRF7 between asthmatics and control. Wilcoxon signed rank test was used for the analyses of control and rhinovirus-treated paired samples. Statistical analyses were performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA); a p value of <0.05 was deemed to indicate statistical significance.
The mean age of asthmatics was 45.4 ± 15.7 years and 40% was a male, which were not different with those of control group. All of asthmatics had showed episodic asthmatic symptoms in the past 4 weeks of the enrollment and their asthmatic symptoms were not controlled adequately, although they were not in the exacerbation. The average score of asthma control test (ACT) was 16.3 ± 5.3 and mean predicted % of FEV1 was 82.8% ± 19.7% at the time of enrollment. Seventy five percent of patients showed atopy on their skin test or blood test for allergy for common inhalant allergens. The mean total IgE level was 373.6 ± 467.5 IU/mL (Table 2).
We evaluated the mRNA expressions of IFN-α, IFN-β, and IRF7 in PBMCs of each subject after ex vivo rhinovirus stimulation. All mRNA expressions of IFN-α, IFN-β, and IRF7 were significantly increased at 12 hours after rhinovirus stimulation compared to media only-treated controls. The relative expressions to beta-actin of IFN-α in the asthmatics group was significantly lower than those in the normal control group (p=0.005) (Fig. 1A). Asthmatics also showed significantly lower relative expressions to beta-actin of IFN-β compared with normal control (p=0.003) (Fig. 1B). When we checked the mRNA expression of IRF7 which is one of crucial transcriptional factor for gene expression of type I IFN after rhinovirus infection, the relative mRNA expression to beta-actin was significantly reduced in the asthmatics compared with normal control (p=0.048) (Fig. 1C). The protein levels of IFN-α and IFN-β were significantly increased at 12 hours after rhinovirus stimulation compared to media only-treated controls, but there was no significance difference between normal control and asthmatics (Fig. 2A, B).
To investigate the mechanism of reduced IRF7 response to rhinovirus in the asthmatics, we evaluated the baseline DNA methylation status of IRF7 gene promotor region using bisulfite pyrosequencing. A total of 16 CpG sites were evaluated with three sets of amplification and sequencing primers and 5 positions were passed quality criteria (Fig. 3A). However, no significant difference of methylation percentage was observed between asthmatics and controls in all the 5 positions of CpG loci (Fig. 3B).
In the present study, we found the reduced mRNA expression of IFN-α and IFN-β after rhinovirus stimulation in the PBMCs of asthmatics. Furthermore, we found the reduced mRNA expression of IRF7 in the response to rhinovirus in the asthmatic PBMCs. IRF7 is the important transcriptional factor for type I IFN production and this is the first study to suggest the role of IRF7 for possible mechanism of impaired antiviral type I IFN in the asthmatics. For the mechanism of down-regulated IRF7 expression, epigenetic changes in the IRF7 gene were investigated, but altered DNA methylation was not detected in the promotor of IRF7 gene.
Rhinovirus infection is the most commonly implicated cause of asthma exacerbation in both adults and children [4, 5]. In a longitudinal cohort study, patients with asthma did not have more rhinovirus infection than healthy individuals. However, more prolonged and severe lower respiratory tract symptoms were noticed in the asthmatics compared with healthy individuals [18]. A longitudinal observation study by Olenec et al. [19] revealed viral-associated illness was associated with a greater duration and severity of cold and asthma symptoms in children with asthma. Moreover, rhinovirus infection caused more extended and severe illness and more frequent loss of asthma control in children with allergic asthma compared with in those with nonallergic asthma [19]. These studies suggest that there might be an inherent difference in the response to respiratory virus infection in asthmatic subjects, especially in allergic asthma.
A variety of possible mechanisms have been suggested for the susceptibility to respiratory viral infection in asthmatics [4, 5, 20]. Rhinovirus infection induces a wide range of proinflammatory cytokines and chemokines in the airway epithelial cells and innate immune cells like macrophages and innate lymphoid cells [4, 20, 21]. Rhinovirus triggers the recruitment and activation of neutrophil and eosinophil in the airway [4, 20, 21]. A study with experimental rhinovirus infection showed impaired T-helper type 1 and interleukin (IL) 10 response and augmented T-helper type 2 (Th2) response in asthmatic subjects [6]. A chain of these process induced by rhinovirus may contribute to exacerbation of asthmatic symptoms by potentiating the pre-existing airway inflammation.
On the other hands, several studies have indicated impaired antiviral response as a causative factor of susceptibility to the virus in the asthmatics [4, 5]. Rhinovirus replication in vitro was greater in the damaged airway epithelium compared to undamaged epithelium [22]. Thus, airway epithelial damage induced by allergic inflammation may provide a better environment for viral replication. Chronic asthma is characterized by goblet cell metaplasia and increased mucus production [23, 24]. IL-13-induced mucous metaplasia increased the susceptibility to rhinovirus in the human epithelial cells [24]. Furthermore, FOXA3 which is highly expressed in airway goblet cells of patients with asthma induced goblet cell metaplasia, but paradoxically inhibit antiviral innate immune response like IFN production and antiviral defense gene expressions [23]. Recently, defective antiviral type I IFN production came into a spotlight for the susceptibility to respiratory viral infection in asthmatics. Wark et al. [7] first found the deficient IFN-β, impaired apoptosis, and increased viral replication in the primary airway epithelial cells of asthmatics compared with those of normal healthy subjects. Afterwards, defective induction of IFN-λ, type III IFN by rhinovirus was found in the primary epithelial cells and alveolar macrophages of asthmatics and it was highly correlated with the severity of rhinovirus-induced asthma exacerbation [10]. Although some studies performed with primary human airway epithelial cells showed discrepant results [25, 26], these series of studies suggest that defective innate antiviral response in the airway epithelium is implicated in the clinical characteristic of asthma prone to exacerbate after respiratory viral infection.
Type I IFNs such IFN-α and IFN-β are principal IFNs produced in human PBMCs, and blood immune cells including plasmacytoid dendritic cells have a major function of innate antiviral response [27, 28]. Since early 2000s, altered response to rhinovirus in type 1 immune response (lower IFN-γ/IL-4, lower IL-12, and higher IL-10) and expression of costimulatory molecules have been reported in the PBMCs of atopic asthmatic patients [29, 30]. Decreased virus-induced IFN-α has been reported in the blood samples from atopic children and adults with allergic asthma [31, 32]. The impaired IFN response was also demonstrated in the in vitro rhinovirus stimulation by Iikura et al. [8] using PBMCs from asthmatics. However, the impaired IFN response to rhinovirus was not observed at 8, 24, and 48 hours in the PBMCs in a recent study by Sykes et al. [9] which demonstrated the defective antiviral IFN-α and IFN-β responses in the bronchoalveolar lavage cells in patients with asthma. Our study demonstrated the reduced type I IFN mRNA expression at the 12 hours after rhinovirus-16 stimulation, although no difference was found in the type I IFN protein analysis of the PBMC supernatants like the result of study by Sykes et al. [9]. It is uncertain the reduced mRNA expression can affect the type I IFN production and innate immune defense in the PBMCs. However, the previouse report by Iikura et al. [8] showed deficient response of IFN-α in the PBMCs of asthmatics when they evaluated at the 72 hours after rhinovirus infection. Time kinetics might be involved in the altered expression of type I IFN production and secretion. It is one of our limitation that longer time point (>48 hours) was not evaluated in this study. Further study is needed to elucidate the meaning of alter mRNA expression at 12 hours and the discrepancy between studies.
The discrepancy among studies can be also related with characteristics of study subjects. Impaired IFN response to rhinovirus appears to be associated with severity of asthma and atopy status. In the severe therapy resistant atopic subjects, defective IFN response was detected, but it was not observed in the well-controlled asthma [33, 34, 35]. Recent studies demonstrated that an important role of FceRI pathway and IgE cross-linking in the impairment of antiviral response, which suggest that atopy is a crucial factor determining antiviral IFN response [36, 37]. The suppressed IFN secretion and dysfunction of plasmacytoid dendritic cell eventually can affect the following adaptive immune response and lead to exaggeration of Th2 cytokine synthesis [38]. Our study was carried out for uncontrolled symptomatic adult asthmatics with average ACT score of 16.3, and most of them had atopic diathesis. These features of subjects might contribute to the impaired IFN mRNA expression to rhinovirus in our study.
The precise mechanism of impaired IFN response to respiratory virus is not understood well to date, but several studies have been reported about this issue. Transforming growth factor-beat (TGF-β) contributes to suppressed IFN response to rhinovirus possibly via suppressor of cytokine signaling (SOCS)-1 and SOCS-3 [39]. TGF-β which is up-regulated in the rhinovirus-stimulated PBMCs under atopic environment is also related with lower production of IL-6, IL-8, and RANTES (regulated on activation, normal T cell expressed and secreted) in the epithelial cells and results in increased viral proliferation [40]. The signaling of pattern recognition receptors after rhinovirus infection such as toll-like receptor (TLR) 3 and MDA5 (melanoma differentiation-associated protein 5) was impaired in the epithelial cells of asthmatics, although the expressions of receptors were not down-regulated [41]. A recent study which compared the PBMCs from asthmatics and healthy donors showed multiple alterations of innate antiviral signaling pathways including reduced expressions of IRF1, IRF7, NF-κB (nuclear factor kappalight-chain-enhancer of activated B cells) family members and STAT1 (signial transducer and activator of transcription 1) and reduced responsiveness to TLR7/TLR8 activation [42]. As this study report, reduced mRNA expression of IRF7 was found in the asthmatic subjects compared to healthy subject in our study. IRF7 is a key transcriptional factor for type I IFN expression in epithelial cells and plasmacytoid dendritic cells [13]. However, impaired expression of IRF7 has not been well recognized as a mechanism for impaired IFN response in asthmatics to date. Our study focused on the altered IRF7 expression as a potential mechanism for impaired IFN response.
Previous reports have shown that the expression of IRF7 is regulated epigenetically by DNA methylation [14, 15]. Asthma is a complex multifactorial disease, in which various environmental factors including allergen, microbiome, air pollution, and diet affect gene expression. Epigenetic regulation can provide mechanistic explanations for the unsolved questions about asthma such as variable disease onset and remission, gene-environment interaction, and multigenerational transmission of trait [12]. We hypothesized that the reduced expression of IRF7 is caused by hypermethylation of IRF7 gene and investigated DNA methylation status of IRF7 gene promotor region to elucidate the mechanism of reduced IRF7 expression in asthmatics. Recent study by Jaspers et al. [16] which revealed the epigenetic modulation of IRF7 gene in nasal epithelial cell as a potential mechanism of the susceptibility to influenza virus in smoker supported our hypothesis. However, we could not find any difference of DNA methylation between asthmatics and healthy subjects in the promotor region of IRF7 gene. Another mechanism might be involved in the impaired IRF7 and type I IFN gene expression such as other epigenetic regulations (histone modification, microRNA etc.), alteration of other transcriptional factor regulation, and genetic polymorphisms of transcriptional factors. Further studies are warranted to clarify more the mechanism of impaired IFN and IRF7 response in asthmatics.
Our study has several limitations. First, we analyzed mRNA expression of type I IFN gene at only one time point and did not evaluate the protein level at longer time points. Second, we did not evaluate the other gene expressions of transcriptional factors and signaling pathways, because we focused on the gene expression and DNA methylation status of IRF7 as a potential candidate mechanism for the impaired IFN response. Third, only DNA methylation status of IRF7 promotor region was evaluated for the analysis and we could not identify the precise mechanism of reduced IRF7 expression. Nevertheless, our study provides meaningful information about the susceptibility to exacerbation after rhinovirus infection in asthma. Our data revealed impaired type I IFN mRNA expression in response to rhinovirus in the PBMC of asthmatics, which was controversial in the previous reports. Furthermore, our data suggest the defective expression of IRF7 might be a cause of the impaired IFN response to rhinovirus.
In conclusion, the mRNA expression of type I IFN, IFN-α, and IFN-β in response to rhinovirus was impaired in the PBMCs of asthmatics. The mRNA expression of IRF7, transcriptional factor inducing type I IFN was also reduced, but not caused by altered DNA methylation in the IRF7 gene promotor.
Figures and Tables
Fig. 1
Expressions of type I interferon (IFN) and interferon regulatory factor 7 (IRF7) mRNA in response to rhinovirus stimulation in the peripheral blood mononuclear cells of asthmatics and healthy subjects. IFN-α (A), IFN-β (B), and IRF7 (C) values in panels A, B and C are mean ± standard error of the mean. RV 16, rhinovirus 16. *p < 0.05. **p < 0.01.

Fig. 2
Protein levels of type I interferon (IFN) in the supernatant from rhinovirus-stimulated peripheral blood mononuclear cells of asthmatics and healthy subjects. IFN-α (A) and IFN-β (B) values in panels A and B are mean ± standard error of the mean. RV 16, rhinovirus 16. *p < 0.05.

Fig. 3
DNA methylation analysis in the IRF7 gene promotor. (A) Analyzed CpG loci in the IRF7 gene promotor: underlined, analyzed region; black bold, CpG loci; red bold, positions evaluated finally. (B) Comparison of DNA methylation status of IRF7 gene promotor between asthmatics and healthy subjects.

Table 1
Sequences of primers used for amplication, pyrosequencing reactions for IRF7 gene methylation analysis
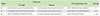
Table 2
Characteristic of study subjects
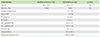
Values are presented as mean ± standard deviation unless otherwise indicated.
NS, nonsignificant; PC20, methacholine provocation concentration causing a 20% fall in FEV1; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; ACT, asthma control test.
*ACT score at the time of enrollment.
ACKNOWLEDGEMENTS
This work was supported by grant No. 04-2008-0040 from Seoul National University Hospital (SNUH) Research Fund.
References
1. Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59:469–478.
2. Jackson DJ, Sykes A, Mallia P, Johnston SL. Asthma exacerbations: origin, effect, and prevention. J Allergy Clin Immunol. 2011; 128:1165–1174.

3. Peters SP, Jones CA, Haselkorn T, Mink DR, Valacer DJ, Weiss ST. Real-world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based survey. J Allergy Clin Immunol. 2007; 119:1454–1461.

4. Jackson DJ, Johnston SL. The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol. 2010; 125:1178–1187.

5. Busse WW, Lemanske RF Jr, Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010; 376:826–834.

6. Message SD, Laza-Stanca V, Mallia P, Parker HL, Zhu J, Kebadze T, Contoli M, Sanderson G, Kon OM, Papi A, Jeffery PK, Stanciu LA, Johnston SL. Rhinovirus-induced lower respiratory illness is increased in asthma and related to virus load and Th1/2 cytokine and IL-10 production. Proc Natl Acad Sci U S A. 2008; 105:13562–13567.

7. Wark PA, Johnston SL, Bucchieri F, Powell R, Puddicombe S, Laza-Stanca V, Holgate ST, Davies DE. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med. 2005; 201:937–947.

8. Iikura K, Katsunuma T, Saika S, Saito S, Ichinohe S, Ida H, Saito H, Matsumoto K. Peripheral blood mononuclear cells from patients with bronchial asthma show impaired innate immune responses to rhinovirus in vitro. Int Arch Allergy Immunol. 2011; 155:Suppl 1. 27–33.

9. Sykes A, Edwards MR, Macintyre J, del Rosario A, Bakhsoliani E, Trujillo-Torralbo MB, Kon OM, Mallia P, McHale M, Johnston SL. Rhinovirus 16-induced IFN-α and IFN-β are deficient in bronchoalveolar lavage cells in asthmatic patients. J Allergy Clin Immunol. 2012; 129:1506–1514.e6.

10. Contoli M, Message SD, Laza-Stanca V, Edwards MR, Wark PA, Bartlett NW, Kebadze T, Mallia P, Stanciu LA, Parker HL, Slater L, Lewis-Antes A, Kon OM, Holgate ST, Davies DE, Kotenko SV, Papi A, Johnston SL. Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med. 2006; 12:1023–1026.
12. Miller RL, Ho SM. Environmental epigenetics and asthma: current concepts and call for studies. Am J Respir Crit Care Med. 2008; 177:567–573.
13. Ning S, Pagano JS, Barber GN. IRF7: activation, regulation, modification and function. Genes Immun. 2011; 12:399–414.

14. Li Q, Tainsky MA. Epigenetic silencing of IRF7 and/or IRF5 in lung cancer cells leads to increased sensitivity to oncolytic viruses. PLoS One. 2011; 6:e28683.

15. Lu R, Au WC, Yeow WS, Hageman N, Pitha PM. Regulation of the promoter activity of interferon regulatory factor-7 gene. Activation by interferon snd silencing by hypermethylation. J Biol Chem. 2000; 275:31805–31812.
16. Jaspers I, Horvath KM, Zhang W, Brighton LE, Carson JL, Noah TL. Reduced expression of IRF7 in nasal epithelial cells from smokers after infection with influenza. Am J Respir Cell Mol Biol. 2010; 43:368–375.

17. Disis ML, dela Rosa C, Goodell V, Kuan LY, Chang JC, Kuus-Reichel K, Clay TM, Kim Lyerly H, Bhatia S, Ghanekar SA, Maino VC, Maecker HT. Maximizing the retention of antigen specific lymphocyte function after cryopreservation. J Immunol Methods. 2006; 308:13–18.

18. Corne JM, Marshall C, Smith S, Schreiber J, Sanderson G, Holgate ST, Johnston SL. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet. 2002; 359:831–834.

19. Olenec JP, Kim WK, Lee WM, Vang F, Pappas TE, Salazar LE, Evans MD, Bork J, Roberg K, Lemanske RF Jr, Gern JE. Weekly monitoring of children with asthma for infections and illness during common cold seasons. J Allergy Clin Immunol. 2010; 125:1001–1006.e1.

20. Hershenson MB. Rhinovirus-Induced Exacerbations of Asthma and COPD. Scientifica (Cairo). 2013; 2013:405876.

21. Kumar RK, Foster PS, Rosenberg HF. Respiratory viral infection, epithelial cytokines, and innate lymphoid cells in asthma exacerbations. J Leukoc Biol. 2014; 96:391–396.

22. Lopez-Souza N, Dolganov G, Dubin R, Sachs LA, Sassina L, Sporer H, Yagi S, Schnurr D, Boushey HA, Widdicombe JH. Resistance of differentiated human airway epithelium to infection by rhinovirus. Am J Physiol Lung Cell Mol Physiol. 2004; 286:L373–L381.

23. Chen G, Korfhagen TR, Karp CL, Impey S, Xu Y, Randell SH, Kitzmiller J, Maeda Y, Haitchi HM, Sridharan A, Senft AP, Whitsett JA. Foxa3 induces goblet cell metaplasia and inhibits innate antiviral immunity. Am J Respir Crit Care Med. 2014; 189:301–313.

24. Lachowicz-Scroggins ME, Boushey HA, Finkbeiner WE, Widdicombe JH. Interleukin-13-induced mucous metaplasia increases susceptibility of human airway epithelium to rhinovirus infection. Am J Respir Cell Mol Biol. 2010; 43:652–661.

25. Lopez-Souza N, Favoreto S, Wong H, Ward T, Yagi S, Schnurr D, Finkbeiner WE, Dolganov GM, Widdicombe JH, Boushey HA, Avila PC. In vitro susceptibility to rhinovirus infection is greater for bronchial than for nasal airway epithelial cells in human subjects. J Allergy Clin Immunol. 2009; 123:1384–1390.e2.

26. Patel DA, You Y, Huang G, Byers DE, Kim HJ, Agapov E, Moore ML, Peebles RS Jr, Castro M, Sumino K, Shifren A, Brody SL, Holtzman MJ. Interferon response and respiratory virus control are preserved in bronchial epithelial cells in asthma. J Allergy Clin Immunol. 2014; 134:1402–1412.e7.

27. Khaitov MR, Laza-Stanca V, Edwards MR, Walton RP, Rohde G, Contoli M, Papi A, Stanciu LA, Kotenko SV, Johnston SL. Respiratory virus induction of alpha-, beta- and lambda-interferons in bronchial epithelial cells and peripheral blood mononuclear cells. Allergy. 2009; 64:375–386.

29. Papadopoulos NG, Stanciu LA, Papi A, Holgate ST, Johnston SL. A defective type 1 response to rhinovirus in atopic asthma. Thorax. 2002; 57:328–332.

30. Papadopoulos NG, Stanciu LA, Papi A, Holgate ST, Johnston SL. Rhinovirus-induced alterations on peripheral blood mononuclear cell phenotype and costimulatory molecule expression in normal and atopic asthmatic subjects. Clin Exp Allergy. 2002; 32:537–542.

31. Bufe A, Gehlhar K, Grage-Griebenow E, Ernst M. Atopic phenotype in children is associated with decreased virus-induced interferon-alpha release. Int Arch Allergy Immunol. 2002; 127:82–88.
32. Gehlhar K, Bilitewski C, Reinitz-Rademacher K, Rohde G, Bufe A. Impaired virus-induced interferon-alpha2 release in adult asthmatic patients. Clin Exp Allergy. 2006; 36:331–337.

33. Edwards MR, Regamey N, Vareille M, Kieninger E, Gupta A, Shoemark A, Saglani S, Sykes A, Macintyre J, Davies J, Bossley C, Bush A, Johnston SL. Impaired innate interferon induction in severe therapy resistant atopic asthmatic children. Mucosal Immunol. 2013; 6:797–806.

34. Sykes A, Macintyre J, Edwards MR, Del Rosario A, Haas J, Gielen V, Kon OM, McHale M, Johnston SL. Rhinovirus-induced interferon production is not deficient in well controlled asthma. Thorax. 2014; 69:240–246.

35. Sykes A, Edwards MR, Macintyre J, Del Rosario A, Gielen V, Haas J, Kon OM, McHale M, Johnston SL. TLR3, TLR4 and TLRs7-9 Induced Interferons Are Not Impaired in Airway and Blood Cells in Well Controlled Asthma. PLoS One. 2013; 8:e65921.

36. Gill MA, Bajwa G, George TA, Dong CC, Dougherty II, Jiang N, Gan VN, Gruchalla RS. Counterregulation between the FcepsilonRI pathway and antiviral responses in human plasmacytoid dendritic cells. J Immunol. 2010; 184:5999–6006.
37. Durrani SR, Montville DJ, Pratt AS, Sahu S, DeVries MK, Rajamanickam V, Gangnon RE, Gill MA, Gern JE, Lemanske RF Jr, Jackson DJ. Innate immune responses to rhinovirus are reduced by the high-affinity IgE receptor in allergic asthmatic children. J Allergy Clin Immunol. 2012; 130:489–495.

38. Pritchard AL, Carroll ML, Burel JG, White OJ, Phipps S, Upham JW. Innate IFNs and plasmacytoid dendritic cells constrain Th2 cytokine responses to rhinovirus: a regulatory mechanism with relevance to asthma. J Immunol. 2012; 188:5898–5905.

39. Bedke N, Sammut D, Green B, Kehagia V, Dennison P, Jenkins G, Tatler A, Howarth PH, Holgate ST, Davies DE. Transforming growth factor-beta promotes rhinovirus replication in bronchial epithelial cells by suppressing the innate immune response. PLoS One. 2012; 7:e44580.

40. Xatzipsalti M, Psarros F, Konstantinou G, Gaga M, Gourgiotis D, Saxoni-Papageorgiou P, Papadopoulos NG. Modulation of the epithelial inflammatory response to rhinovirus in an atopic environment. Clin Exp Allergy. 2008; 38:466–472.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download