Abstract
Background
Current statistics show that approximately 10% of patients claim to be allergic to penicillin yet only 10% of these have demonstrable allergy. The most appropriate and cost-effective antibiotics are sometimes withheld on the basis of patient history of drug allergy.
Objective
Investigation of IgE hypersensitivity and delayed hypersensitivity in patients with a history of penicillin allergy to a teaching hospital allergy clinic.
Methods
Patients underwent skin prick and intradermal testing (IDT) with major and minor penicillin determinants. Those with negative skin tests were administered a three-day oral challenge. Demographic and clinical details about the reactions were noted.
Results
One hundred twenty eight patients underwent testing, of these, one hundred and ten had self-reported histories of penicillin allergy and eighteen were referred because of other antibiotic allergies. Seventeen patients with self-reported penicillin allergy had either positive skin tests or oral challenge results, corresponding to 15% of patients having proven allergy. None reacted on skin prick testing, four reacted to IDT, thirteen reacted to oral challenge (five immediate and eight delayed). Analysis of clinical histories showed that patients with a well-defined history of allergy and a history of anaphylaxis were more likely to have a positive test compared to patients with vague histories. Skin testing proved to be less sensitive than oral challenge.
Conclusion
A minority of patients presenting with a history of penicillin allergy have evidence of immune-mediated hypersensitivity (17/110, 15%) in this study. Of these, eight out of seventeen (47%) had delayed reactions, demonstrating the usefulness and discriminating power of objective testing, which must include three-day oral challenge. Discriminating factors for immune-mediated allergy from patient history were a clear description of the original reaction and a history of anaphylaxis. Negative allergy testing enables the use of penicillin as first-line treatment when necessary and this can significantly reduce costs of antibiotics.
The most appropriate and cost-effective antibiotics are sometimes withheld from patients because of self-reported clinical histories of penicillin allergy [1, 3]. This affects not only the prescription of penicillins, but also the prescription of certain cephalosporin antibiotics, because of the risk of cross-reactivity [4]. Current statistics show that about 10% of patients claim to have a penicillin allergy, but it is likely that immunological testing will prove that a much smaller number of these patients have a true allergy to penicillin [1, 5].
The aim of this study was to determine the number of patients with evidence of penicillin allergy after testing amongst those with a self-reported penicillin allergy that have been referred to a tertiary allergy/immunology clinic. Secondary aims included correlation of allergy test results with main presenting symptoms and age of onset of reactions, and investigating the utility of skin testing and oral challenge testing.
The patient population used for this study consisted of patients from Campbelltown Hospital Allergy & Immunology Clinic who had been referred for investigation of penicillin allergy. Patients ages ranged from 9 years old to 93 years old.
Clinical histories were taken and included age at onset of reaction, drug implicated and details of the adverse events, noting the characteristics of the reaction, where they were known. The following features were tabulated.
Patients attended the outpatient clinic where they underwent skin prick and intradermal tests using protocols previously described [1]. If the skin tests were negative, an oral challenge was performed. Patients with positive skin tests were not challenged orally.
Skin prick testing (SPT) and intradermal testing (IDT) were performed using neat solutions of major and minor determinants of penicillin (Diater S.A. Avda. Gregorio Peces Barba, 2 - Parque Technológico de Leganés; 28918 Leganés. [Madrid] Spain) for SPT and dilutions of 1:10 for ID tests, solutions of ampicillin 1:1000 (for ID tests) and neat (for SPT), histamine 10 mg/mL as positive control (Hollister Stier) and normal saline as negative control.
Some patients were also tested for cephalosporin allergy, using neat solutions of cephalothin and ceftriaxone for SPT and 1:1000 dilutions for IDT.
SPT results were read after 15 minutes and IDT results were read after 30 minutes. For both tests, a wheal of diameter of > 3 mm was considered positive.
Testing followed Australasian Society of Clinical Immunology and Allergy guidelines for SPT [6].
If SPT and IDT were negative, patients were given an oral challenge. Oral challenges were performed with 250 mg/5 mL Amoxil syrup in all patients except for 12 patients, in whom phenoxypenicillin was used. Phenoxypenicillin 150 mg was used only in instances where the patient had named it as causing the original reaction. If the initial challenge caused no reaction, patients were given the drug to take home with instructions to take it for three days and report any reactions.
One hundred and ten patients with self-reported histories of penicillin allergy underwent testing. Of these, seventeen had a positive result with four patients reacting to IDT and thirteen reacting to oral challenge. Thus, only 15.5% of all patients reporting allergy had a confirmed allergic reaction to penicillin.
Most patients had little or no knowledge of the clinical characteristics of previous penicillin reactions. Of one hundred and ten patients, ninety one provided some details of their clinical histories. There were differences in the clinical histories between patients with positive and negative test results regarding the type of reaction. Other features of the clinical histories did not show substantial differences.
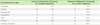
Table 1 compares the various reactions between challenge/skin test positive and negative groups. There was a significant difference in reports of urticaria and anaphylaxis, with these reactions being more common in the positive test group. There were no significant differences in other categories.
Seventy four patients described an age of onset of reaction to penicillin, most commonly below the age of 10 years, described by twenty nine patients (39%). The range of age of presentation was below 10 years and over 60 years.
Based on clinical histories, seventy seven patients had no other adverse drug reactions or allergies to drugs other than penicillin. There was no significant difference between the positive and negative test groups. In fifty one patients other drug reactions were described, the most common being to cephalosporins. In this group, only two patients (29%) had reacted positively to penicillin allergy testing.
In total, one hundred and twenty eight patients underwent tests and of these, eighteen patients had no history of a reaction to penicillin but were referred for testing because of a history of multiple drug allergies, and they had a requirement for penicillin as part of their treatment. Ten of these 18 (56%) had a history of adverse drug reactions to cephalosporin antibiotics.
36 patients within the entire study population were tested with cephalosporin reagents as well as penicillin reagents. The same testing protocol was used for both drugs. One patient had a positive intradermal test, and one patient had positive oral challenge test to a cephalosporin. There were no patients found to be positive to both penicillin and cephalosporins.
Six of 110 patients reported a family history allergy to penicillin. Two of these six tested positive to oral challenge.
Seventeen patients in total reacted positively to either oral or skin testing with penicillin reagents. Four patients demonstrated positive IDTs. Thirteen patients who were negative on skin testing had a positive oral challenge, five of whom developed immediate reactions to the drug. These five patients, along with the four patients who tested positively on IDT had confirmed immediate IgE-mediated reactions to penicillin. Eight patients experienced delayed reactions over the three day challenge, and these included both widespread and localised rashes with no patient experiencing any other more serious delayed reaction. The patients that reacted positively on oral challenge and IDT, had negative SPTs. Thus, SPT with penicillin reagents had a sensitivity of 0% and IDT with penicillin reagents a sensitivity of 44%. Of those patients with negative skin prick results, one hundred and eleven had negative oral challenges. Thus, the SPT had a specificity of 93% and the IDT a specificity of 96%.
Only 17/110 (15.5%) of patients with a history of penicillin allergy were found to have a reaction to penicillin on allergy testing which is in agreement with the published literature on this. Clinically, this indicates that patient reporting of a history of penicillin allergy has a poor predictive value in determining allergic (both IgE mediated and non-IgE mediated) reactions to penicillin and demonstrates the usefulness of an allergy consultation with appropriate testing to determine which patients are at risk of reactions to penicillin.
There are a number of reasons for the large occurrence of over-reporting of penicillin allergies. A major reason is a lack of ability of patients to differentiate between a side effect of a drug and an allergic reaction. Another reason is the propensity for children to develop rashes, associated with febrile viral illnesses either as a consequence of the infectious agent or as a result of pyrexia [1]. Examples of viral or bacterial infections that may be mistaken for allergic reactions are roseola infantum, impetigo, coxsackie and enteroviruses. Also, some patients do not recall their allergies, but rather have been informed of the reaction by a carer (usually a parent) and therefore cannot adequately describe a reaction to rule out allergy. Overdiagnosis may be a result of clinicians merely accepting a diagnosis of allergy without taking a detailed history to determine likelihood of actual allergy [1, 7].
Our results showed that patients with positive challenges tended to have clearer patient-reported clinical histories of reaction. Seventy two percent of patients with confirmed reactions to penicillin, either with oral challenge or skin testing, had a well-defined description of the original reaction compared with 51% of negative-reactors. In the positive reactor group, 29% of reactions were urticarial (compared to 13% in negative group) and 24% described anaphylaxis (compared to 4% in negative group). This indicates that patients with a previous history of anaphylaxis or urticaria were more likely to react positively on challenge.
If no facilities are available to evaluate patients, those with a well-defined history of allergic symptoms, or descriptions of urticaria or anaphylaxis following penicillin use previously, should avoid the use of penicillins.
Eighteen patients without a specific history of penicillin allergy were tested due to the presence of other drug allergies. None of these patients tested positive to penicillin reagents. Comparably, Salkind et al. [1] calculated the likelihood of a positive test in the absence of a history of penicillin reaction to be 0.05% based on a review of four other studies, thus demonstrating the importance of a history of allergy, and the lack of utility of skin testing in the absence of any history.
Thirty-nine percent of patients who gave a history of age of onset of reaction described reactions under the age of ten years. This was the most commonly described age of onset of reaction in both those that reacted positively to allergy testing and those that didn't. This is most likely due to penicillin being the most commonly prescribed outpatient drug for minor infections in this age group or development of rash due to the presence of a viral illness.
A notable finding was that other than penicillin, cephalosporins were the most commonly described "other drug adverse reaction", with 29% describing reactions to cephalosporins in the positive group and 57% in the negative group. The similarity between the positive and negative groups reflects the usage patterns with these antibiotics. The relation between allergy to penicillin and cephalosporins cannot be commented on in this study due to the small number of patients that were tested for both drugs and the limited history of cephalosporin allergy collected.
Only six patients had a positive family history of penicillin allergy. Therefore, the influence of family history on occurrence of penicillin allergy could not be adequately tested. Current literature states the risk of cross-reactivity of penicillins and cephalosporin allergy is much lower than previously estimated with some studies stating figures between 1.5%-1.6% [1, 4, 8]. Thirty six patients in this study were also tested for cephalosporin allergy as well as penicillin allergy. Of these, no patients were found to have both penicillin and cephalosporin allergy. Our sample size was too small to accurately calculate risk of cross-reactivity.
Skin testing is a reflection of IgE-mediated hypersensitivity and has no value in predicting other mechanisms of adverse drug reactions (either immunological or non-immunological) [1, 2]. In this study, SPT for IgE-mediated penicillin hypersensitivity had very poor sensitivity but strong specificity. This highlights the importance of performing IDT and oral challenge testing regardless of a negative SPT.
Of the patients undergoing oral challenges that had a positive result, 8/13 (57%) presented with delayed reactions to the challenge drug. This emphasises the utility of performing three-day challenges to detect non-IgE-mediated hypersensitivity.
Patients who were found to be positive on skin testing were not challenged; therefore the positive predictive value of skin testing could not be determined by this study.
The poor correlation between patient-reported allergy histories and positive allergy test reactions shown in this study demonstrates the requirement for further testing to determine the presence of penicillin allergy. However, the relatively high false negative rate of skin testing (13/17, 76%) suggests that the use of skin testing is not as valuable as three-day oral challenge testing. These results suggest that if clinically safe, oral challenge testing is the best test to determine the presence of penicillin allergy.
In conclusion, of one hundred and ten patients with a self-reported history of penicillin allergy and eighteen patients with suspected penicillin allergy due to multiple other allergies, only seventeen had positive reactions to allergy testing. Nine were found to have IgE-mediated allergy on skin prick or oral challenge testing and eight were found to have delayed-type reactions. Thus only 15.5% of patient-reported penicillin allergy resulted in allergic reactions to penicillin. The use of a detailed history is limited by patient recall. For patients with accurate histories, factors likely to discriminate positive reactors to allergy testing from negative are the presence of a clear description of reaction and a history of anaphylaxis. Other historical factors were not significantly different between positive and negative reactors.
This low correlation between history of allergy and proven allergy demonstrates the utility of performing allergy tests. A negative test result then allows the use of the most cost effective antibiotic therapy and limits the use of second line agents that are generally more expensive.
While skin testing proved to be a reasonable screen, full elucidation of allergy required a three-day oral challenge.
Figures and Tables
ACKNOWLEDGEMENTS
The authors acknowledge Prof. B Frankum, Dr. K Keat, Dr. S Gala for referring patients and Mrs. P Burton and Mrs. F Perram who performed the skin tests.
References
1. Salkind AR, Cuddy PG, Foxworth JW. The rational clinical examination. Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy. JAMA. 2001. 285:2498–2505.
2. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD, Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009. 54:72–77.

3. Kalogeromitros D, Rigopoulos D, Gregoriou S, Papaioannou D, Mousatou V, Katsarou-Katsari A. Penicillin hypersensitivity: value of clinical history and skin testing in daily practice. Allergy Asthma Proc. 2004. 25:157–160.
4. DePestel DD, Benninger MS, Danziger L, LaPlante KL, May C, Luskin A, Pichichero M, Hadley JA. Cephalosporin use in treatment of patients with penicillin allergies. J Am Pharm Assoc (2003). 2008. 48:530–540.

5. MacPherson RD, Willcox C, Chow C, Wang A. Anaesthetist's responses to patients' self-reported drug allergies. Br J Anaesth. 2006. 97:634–639.

6. Australasian Society of Clinical Immunology and Allergy and Allergy Skin Prick Testing Working Party. Skin prick testing for the diagnosis of allergic disease: a manual for practitioners. 2006. Balgowlah, NSW: Australasian Society of Clinical Immunology and Allergy;26. [revised 2009 March].
7. Surtees SJ, Stockton MG, Gietzen TW. Allergy to penicillin: fable or fact? BMJ. 1991. 302:1051–1052.

8. Chaabane A, Aouam K, Boughattas NA, Chakroun M. Allergy to betalactams: myth and realities. Med Mal Infect. 2009. 39:278–287.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download