1. Uribe FA, Chandhoke TK, Nanda R. Individualized orthodontic diagnosis. In : Nanda R, editor. Esthetics and biomechanics in orthodontics. 2nd ed. St. Louis (MA): Elsevier Saunders;2015. p. 1–32.
2. Bourzgui F, Sebbar M, Hamza M. Orthodontics and caries. In : Naretto S, editor. Principles in contemporary orthodontics. Rijeka: INTECH;2011. p. 309–326.
3. Chaussain C, Opsahl Vital S, Viallon V, Vermelin L, Haignere C, Sixou M, Lasfargues JJ. Interest in a new test for caries risk in adolescents undergoing orthodontic treatment. Clin Oral Investig. 2010; 14:177–185.

4. Lynch CD, Opdam NJ, Hickel R, Brunton PA, Gurgan S, Kakaboura A, Shearer AC, Vanherle G, Wilson NH; Academy of Operative Dentistry European Section. Guidance on posterior resin composites: Academy of Operative Dentistry - European Section. J Dent. 2014; 42:377–383. PMID:
24462699.

5. Ferracane JL. Current trends in dental composites. Crit Rev Oral Biol Med. 1995; 6:302–318. PMID:
8664421.

6. Ilie N, Hickel R. Resin composite restorative materials. Aust Dent J. 2011; 56(Supplement 1):59–66. PMID:
21564116.

7. de Andrade AK, Duarte RM, Medeiros e Silva FD, Batista AU, Lima KC, Monteiro GQ, Montes MA. Resin composite class I restorations: a 54-month randomized clinical trial. Oper Dent. 2014; 39:588–594. PMID:
25084108.

8. Ferracane JL. Resin composite--state of the art. Dent Mater. 2011; 27:29–38. PMID:
21093034.

9. Gresnigt MM, Kalk W, Ozcan M. Randomized controlled split-mouth clinical trial of direct laminate veneers with two micro-hybrid resin composites. J Dent. 2012; 40:766–775. PMID:
22664565.

10. Wolff D, Kraus T, Schach C, Pritsch M, Mente J, Staehle HJ, Ding P. Recontouring teeth and closing diastemas with direct composite buildups: a clinical evaluation of survival and quality parameters. J Dent. 2010; 38:1001–1009. PMID:
20826192.

11. Neves Ade A, Coutinho E, De Munck J, Van Meerbeek B. Caries-removal effectiveness and minimal-invasiveness potential of caries-excavation techniques: a micro-CT investigation. J Dent. 2011; 39:154–162. PMID:
21111770.
12. de Souza Costa CA, Teixeira HM, Lopes do Nascimento AB, Hebling J. Biocompatibility of resin-based dental materials applied as liners in deep cavities prepared in human teeth. J Biomed Mater Res B Appl Biomater. 2007; 81:175–184. PMID:
16969818.

13. Demirci M, Uysal O. Clinical evaluation of a polyacid-modified resin composite (Dyract AP) in Class I cavities: 3-year results. Am J Dent. 2006; 19:376–381. PMID:
17212081.
14. Barnes DM, Blank LW, Gingell JC, Gilner PP. A clinical evaluation of a resin-modified glass ionomer restorative material. J Am Dent Assoc. 1995; 126:1245–1253. PMID:
7560584.
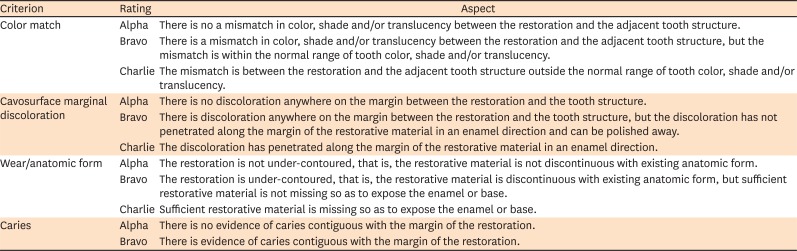
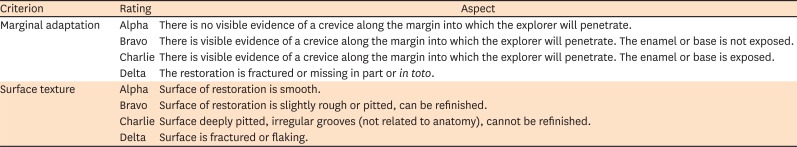
15. Ryge G. Clinical criteria. Int Dent J. 1980; 30:347–358. PMID:
6935165.
16. Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig. 2005; 9:215–232.
17. Sakaguchi RL, Powers JM. Craig's restorative dental materials. 13th ed. Philadelphia (PA): Elsevier Mosby;2012. p. 166–167.
18. 3M Dental Products Laboratory (US). Filtek™ Z250 universal restorative system: technical product profile. St. Paul (MN): 3M;1998.
19. Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent. 2013; 38:E1–E11.

20. Lempel E, Tóth Á, Fábián T, Krajczár K, Szalma J. Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater. 2015; 31:115–122. PMID:
25480695.

21. da Rosa Rodolpho PA, Cenci MS, Donassollo TA, Loguércio AD, Demarco FF. A clinical evaluation of posterior composite restorations: 17-year findings. J Dent. 2006; 34:427–435. PMID:
16314023.

22. Manhart J, Chen H, Hamm G, Hickel R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004; 29:481–508. PMID:
15470871.
23. Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012; 28:87–101. PMID:
22192253.

24. Bagheri R, Burrow MF, Tyas M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent. 2005; 33:389–398. PMID:
15833394.

25. Manhart J, Chen HY, Hickel R. Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J Adhes Dent. 2010; 12:237–243. PMID:
20157663.
26. Wilder AD Jr, May KN Jr, Bayne SC, Taylor DF, Leinfelder KF. Seventeen-year clinical study of ultraviolet-cured posterior composite Class I and II restorations. J Esthet Dent. 1999; 11:135–142. PMID:
10825870.

27. Baldissera RA, Corrêa MB, Schuch HS, Collares K, Nascimento GG, Jardim PS, Moraes RR, Opdam NJ, Demarco FF. Are there universal restorative composites for anterior and posterior teeth? J Dent. 2013; 41:1027–1035. PMID:
24001506.

28. Da Rosa Rodolpho PA, Donassollo TA, Cenci MS, Loguércio AD, Moraes RR, Bronkhorst EM, Opdam NJ, Demarco FF. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent Mater. 2011; 27:955–963. PMID:
21762980.

29. Schirrmeister JF, Huber K, Hellwig E, Hahn P. Four-year evaluation of a resin composite including nanofillers in posterior cavities. J Adhes Dent. 2009; 11:399–404. PMID:
19841767.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download