Abstract
Purpose
The purpose of this study is to describe a method of inserting cement in the femoral head before fixation with dynamic hip screw to prevent screw cut out due to osteoporosis and to evaluate its clinical outcome in these patients.
Materials and Methods
In this prospective study, 30 patients aged 60 years and older with intertrochanteric fracture were included. Bone mineral density was measured. After reaming of the femoral head and neck with a triple reamer and polymethyl methacrylate, bone cement was introduced into the femoral head using a customized nozzle and a barrel fitted on a cement gun. A Richard screw was inserted and the plate was fixed over the femoral shaft. Patients were mobilized and clinical outcomes were rated using the Salvati and Wilson's scoring system.
Results
More patients included in this study were between 66 and 70 years old than any other age group. The most common fracture according to the Orthopaedic Trauma Association classification was type 31A2.2 (46.7%). The T-score was found to be −2.506±0.22 (mean±standard deviation); all patients were within the range of −2.0 to −2.8. The duration of radiological union was 13.67±1.77 weeks. Salvati and Wilson's scoring at 12 months of follow up was 30.96±4.97. The majority of patients were able to perform their normal routine activities; none experienced implant failure or screw cut out.
Intertrochanteric fractures are relatively common in the elderly, particularly in women who are osteoporotic (i.e., three to four times more likely than in non-osteoporotic women), and trivial falls are the most common cause1). While extramedullary and intramedullary implants are available for the treatment of intertrochanteric fractures, fixation failure following these treatment approaches is not uncommon in osteoporotic patients (i.e., reported incidence of up to 10%23)). A decrease in bone mineral density (BMD) could also lead to fixation failure even if all other factors (e.g., screw position) are satisfactory, since: i) it is difficult to obtain sufficient anchorage of a neck screw in the femoral head which may lead to superior screw cut out, and ii) backing out of the screw may occur (Fig. 1). To improve implant anchorage, augmentation of the implant with bone cement has been employed. Cement in the femoral head increases the load-bearing area of the device (i.e., area through a plane perpendicular to the applied load), thereby reducing the risk of implant failure and superior reduction in the risk of screw cut out4).
We conducted this study with the aim of describing a simple, yet innovative, technique involving the introduction of cement into the femoral head to provide additional anchorage for lag screws in osteoporotic patients with intertrochanteric fractures treated with dynamic hip screws (DHS) and to assess the related functional outcomes.
This prospective study was conducted following approval from our institution's ethics committee (approval no. - F.3/Acad./Ethical comm./MCK/2015/440). Patients aged 60 years and older with an intertrochanteric fracture occurring fewer than three weeks prior were included in this study after obtaining informed consent. All fractures were classified using the Orthopaedic Trauma Association (OTA) classification criteria. Patients with the following were excluded: i) unstable lateral wall or greater trochanter fractures, ii) changes in electrocardiography (as cement-related complications may occur in such patients), iii) malunited or open trochanteric fractures, iv) medically unstable, or v) other femur and/or pathological fractures. BMD was calculated using a peripheral dual-energy X-ray absorptiometry (pDEXA) scanner within 24 hours of admission. A total of 44 patients were screened but only 30 who had BMD less than −2.0 were included in study. Patients in this study were put on preoperative, below-knee skin traction with up to 4 kg of weight. Parenteral and oral analgesics, as available in hospital, were given to all patients to relieve pain and were taken for elective surgery as soon as possible after preoperative work-up. A 135° barrel plate along with standard DHS instrumentation was employed. For the purpose of augmentation, low viscosity polymethyl methacrylate (PMMA) bone cement inserted into the femoral head using a cement gun with a customized nozzle as indicated in Fig. 2 was used. The customized nozzle diameter (7.5 mm mounted over a barrel) allowed for insertion into the void created following triple reaming (diameter of 8 mm). Because the screw track and nozzle have similar diameters, the screw track was completely obliterated during cement injection, thereby preventing any backflow during injection. Patients were positioned supine on the fracture table and the fracture was reduced. Following incision and exposure of the proximal shaft, guide wires were inserted and triple reaming done. PMMA bone cement was mixed to a semi-liquid state and placed in a cement gun. Under fluoroscopic control, the long barrel of the cement-filled gun was inserted as far as possible into the hole in femoral head over the guide wire and cement was injected (Fig. 3). Because of the nature of proximal femur anteversion, the cement in the proximal fragment had a tendency to flow backward and leak into the fracture gap when the patient was lying in the supine position. To overcome proximal femur anteversion, the fracture table was tilted 30° toward the contralateral side of the patient's injured limb. Cement injection was started from the most proximal part of the screw tract (from femoral head towards the trochanter) while simultaneously pulling the femoral nozzle backward; cement injection was stopped when the tip of the nozzle reached within 1 cm of the cervicotrochanteric area. After injection, the cement gun was quickly removed and a lag screw of appropriate length was quickly inserted (Fig. 4). Next, the guide wires were removed followed by: i) attachment of a side plate, ii) tightening of the compression screw, and iii) closure over suction drainage. Satisfactory fracture reduction and a tip apex distance (TAD) of less than 25 mm was ensured. Antibiotics and analgesics were provided postoperatively and sutures removed on post-operative day 12. Patients were encouraged to start static quadriceps exercises and active knee bending from post-operative day 2. All patients were allowed partial weight bearing under the guidance of a physiotherapist after suture removal, and were allowed full weight bearing as soon as possible, depending on the tolerance of the patient. The patients were followed up clinically and radiologically at regular intervals. Radiological union was assessed by cortical continuity and progressive loss of fracture line on radiographs during follow up and the clinical outcomes were rated using the Salvati and Wilson's scoring system at every follow up.
Two patients expired and one was lost during follow up; hence, 27 patients were included in the final analysis. More patients in this study were in the age group of 66 to 70 years (9 cases, 30.0%) than any other age group, and the mean age was 73.23 years (standard deviation [SD], 9.41). The male:female in this study was 2:3, suggesting that females over 60 years old may be more prone to intertrochanteric fractures. The patient's left side was involved in 17 cases (56.7%) and 27 patients (90.0%) sustained their injury due to trivial trauma. The most common fracture type in this study (according to OTA classification) was 31A2 (31A2.1-14 and 31A2.2-6) followed by 31A1 (31A1.2-9 and 3A1.3-1). Twenty-two (73.3%) patients in our study had comorbid medical conditions, most commonly hypertension, followed by chronic obstructive pulmonary disease and diabetes mellitus.
BMD for each patient was calculated using a pDEXA scanner; the mean T-score was −2.506 (SD, 0.22), and all patients fell within the range of −2.0 to −2.8. The mean follow-up duration was 13.6 months and the average time from injury to surgery was 1.8 days. The mean duration of radiological union in our study was 13.67 weeks (SD, 1.77) with a range of 11 to 16 weeks (Fig. 5). All 27 patients who completed the one-year follow up had radiological union in a good position. At one-year of follow up, the mean TAD was 20.7. Mean movements at the end of follow up were slightly less than normal. Mean flexion was 105.5° (SD, 10.9°), mean extension was 6.72° (SD, 2.71°), mean abduction was 32.06° (SD, 7.76°) and mean adduction was 18.1° (SD, 5.77°).
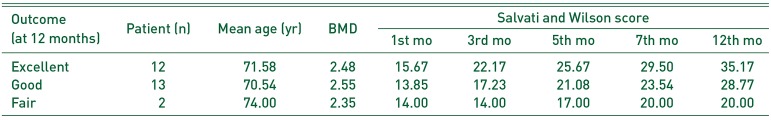
We used the Salvati and Wilson's scoring system-which uses four parameters (i.e., pain, walking, muscle power and function)-to assess clinical outcomes. The results are classified following a sum of the scores for these four parameters as follows: ‘excellent’ (32 or more), ‘good’ (24 to 31), ‘fair’ (16 to 23), and ‘poor’ (15 or less). The mean Salvati and Wilson's scoring at 12 months of follow up was 30.96 (SD, 4.97)-classified as ‘good.’ We observed a progressive increase in all parameters during the follow up (Table 1). Individual results are as follows: ‘excellent’ (n=12), ‘good’ (n=13), and ‘fair’ (n=2) (Table 2).
At the end of the one-year follow-up period, 11 patients (40.7%) reported having “no” pain, while 13 (48.1%) reported having occasional “slight” pain. No patients were bedridden at the conclusion of the one-year follow-up. While 19 patients (70.4%) could walk without any support even for long distances, five (18.5%) reported requiring a single stick for longer distance (>400 yards) and three (11.1%) required a single stick for even shorter distances (<400 yards). Nineteen patients (70.4%) had “good” muscle power (i.e., flexion of more than 90° and abduction of more than 20°), while eight patients (29.6%) had “fair” muscle power (i.e., flexion of 60°–90° and abduction of 10°–20°). The majority of patients were able to perform their normal routine activities, with seven (25.9%) returning to their pre-injury functional status or with only mild restriction, and 11 (40.7%) being able to do most of the house work. Only four patients (14.8%) were house bound (i.e., limited only to activities of daily living), and no patients were bedridden.
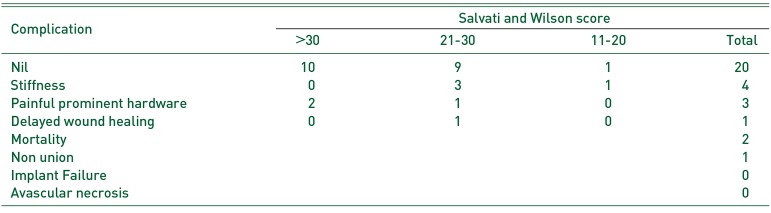
Two patients expired during follow up (mortality rate of 6.7%) due to cardiac arrest owing to their premorbid medical conditions (i.e., hypertension) at 16 weeks and 31 weeks after surgery. Three patients had painful prominent hardware, and four others had stiffness of the hip joint. One patient had delayed wound healing and later developed stiffness of the hip joint. None of our patients had superior screw cut out or any other type implant failure and/or non-union (Table 3).
In elderly patients with osteoporosis, the holding power of a screw can be influence by an increase in porosity of the bone which occurs in these individuals5). Seebeck et al.6) have suggested that most fracture-fixation techniques rely on sufficient screw anchorage in the metaphyseal and diaphyseal regions of the bone and hence safe anchorage of the screws is a prerequisite for success of the entire fixation construct. According to Tencer7), the pullout strength of a screw in trabecular bone depends on the outside diameter of the screw, its length of engagement, the density of bone into which it is embedded, and its thread shape. This author explained that when a screw pulls out of trabecular bone it does so by cutting or shearing with it a core of bone, cutting the core as the threads move outward and trapping the core within the threads. The properties of the outer surface of the core of bone define the screw-purchase strength since failure occurs at this interface. If the outer core is smaller in diameter, shorter, or if the bone material at the interface has lower shear strength (due to loss of bone mass as in osteoporosis), the pullout strength of the screw will decrease. As a result, secondary failure of fixation can occur. Such a failure is bone failure rather than implant failure and can occur in up to 10% of cases23).
Increasing the number of screws, or augmenting the density of bone around the screw, are strategies that have been used to restore screw pullout strength. Augmentation acts by adding a “grout” that helps to resist hardware pullout. Choueka et al.8) noted in their cadaveric study that the greatest average load to failure was in the cemented group with the lowest in the uncemented sliding hip screw group. They also found that device cut out as a cause of failure occurred mostly in the uncemented lag screw group. According to this group, even sliding of the screw was enhanced by methods that increase the fixation surface area within the femoral head, however, it was subject to encroachment of the cement in the region of the barrel-screw junction. Our fixation construct also works based on this principle.
The technique we describe is reasonably simple and uses most of the instrumentation of a conventional DHS, which decreases additional cost. We were able to successfully introduce cement around the femoral head without compromising radiological union or functional outcomes. The latter was rated as per the Salvati and Wilson's scoring system. Most of the patients were pain free at one year with an average pain score of 8.59. There have been other authors who documented good functional outcomes following the use of cemented DHS. Gupta et al.9) had an average pain score of 8.63, similar to the results presented here. Lee et al.10) also reported that in a cemented group, mean hip pain was significantly lower. Gupta et al.9) graded their functional results as ‘excellent’ and ‘good’ in 76.7% (n=46) and 21.6% (n=13) of the cases, respectively. Although the total number of patients with ‘excellent’ outcomes was slightly less in our study (i.e., 44.4%), the total number of patients with scores more than 24 (which includes patients with ‘good’ and ‘excellent’ outcomes) were greater than 90% in both studies. Hence, most patients experienced an improvement in functional outcomes. Bartucci et al.11), using Iowa hip scores, also showed statistically significantly improved results in the cemented group vs. the uncemented group.
We had four patients with stiffness, three with painful prominences and one with delayed wound healing which healed with serial dressings. Two patients expired during follow up due to premorbid-associated cardiac arrest at 16 and 31 weeks. Painful prominences could be attributed to poor and frail musculature and less body fat. In four patients who had stiffness, flexion was limited to 90° or less, compromising squatting and cross legged position necessary for routine activities in our country. All of these complications are related to the procedure of conventional DHS and not the result of using cement. We experienced no patients with lag screw cut out. Lee et al.10)-who conducted a comparative study between cemented and non-cemented group-also noted that the overall complication rate was much lower when cementing was used. Although Wu et al.12) noted incidences of 6 implant failures (out of 67), this was lower when compared with the uncemented group. However, they observed that the mode of implant failure was due to side plate breakage and not lag screw cut out as seen in the uncemented group. Clearly, the incidence of lag screw cut out is almost eliminated with the use of cement augmentation.
The only concern in this procedure is the risk of cement related complications like non-union due to intrusion of cement in the fracture site and avascular necrosis of the femoral head as a result of thermogenic effect of the cement. One of the patients included in this study had no signs of union and constant pain three-months post-operatively (Fig. 6). Unfortunately the patient could not be followed up further as she died due to cardiac arrest. Such incidence of non-union typically results from the intrusion of excess cement at the fracture site. Additionally, as a result of excess cement, we were unable to tighten the screw all the way to the femoral head, resulting in a subpar position of the screw. Using a smaller amount of cement, and limiting it to the cervicotrochanteric area, will not only prevent these complications, but would also decrease the likelihood of avascular necrosis as suggested by Boner et al13). In 2008, this group conducted an in-vitro study to describe the risk of thermal necrosis in human femoral heads during PMMA screw augmentation in osteoporotic bone and concluded that the risk of thermal necrosis exists with cement layer thickness greater than 5.0 mm or with up to 6 mL of PMMA bone cement. It is to be noted that signs of avascular necrosis of the femoral head should appear by the end of one year and none of our patients had such signs; importantly however, Wu et al.12) reported it only in one patient. We do note that if implant removal is warranted as a result of any complication, it would be very challenging and can pose a problem in further management. Thereby, we advocate that cementing should be used only in very elderly patients with limited life expectancy who are at potential risk of a screw cut out due to osteoporosis.
Our study does have several notable limitations. First, the sample size of our study was relatively small; to firmly establish the role of cement in preventing osteoporotic-related fixation failure, studies with larger sample sizes may be required. Secondly, to ideally measure BMD, a central DEXA scanner may provide increased sensitivity. However, this device was not available at our institute, leading us to opt for the pDEXA scanner. Importantly, the International Society for Clinical Densitometry (ISCD) have thoroughly reviewed14) the various aspects of pDEXA and have justified its use for diagnosis of osteoporosis, especially in places where central DEXA is not available.
Augmentation with cement around the threads of a screw may help in anchoring the screw in osteoporotic bone and can decrease the chance of screw cut out without compromising functional outcomes. It is possible to perform the same with conventional DHS instrumentation using a customized nozzle which is highly cost effective. However, introduction of excess cement into fracture site may lead to complications such as non-union.
References
1. Kaufer H. Mechanics of the treatment of hip injuries. Clin Orthop Relat Res. 1980; (146):53–61. PMID: 7371269.

2. Broderick JM, Bruce-Brand R, Stanley E, Mulhall KJ. Osteoporotic hip fractures: the burden of fixation failure. Scientific World Journal. 2013; 2013:515197. PMID: 23476139.

3. Giannoudis PV, Schneider E. Principles of fixation of osteoporotic fractures. J Bone Joint Surg Br. 2006; 88:1272–1278. PMID: 17012413.

4. Choueka J, Koval KJ, Kummer FJ, Crawford G, Zuckerman JD. Biomechanical comparison of the sliding hip screw and the dome plunger. Effects of material and fixation design. J Bone Joint Surg Br. 1995; 77:277–283. PMID: 7706347.

5. Giannoudis PV, Schneider E. Osteoporosis. In : Ruedi T, Buckley R, Morgan CG, editors. AO Principles of fracture management. 2nd ed. Stuttgart: Thieme;2007. p. 469–482.
6. Seebeck J, Goldhahn J, Morlock MM, Schneider E. Mechanical behavior of screws in normal and osteoporotic bone. Osteoporos Int. 2005; 16(Suppl 2):S107–S111. PMID: 15517184.

7. Tencer AF. Mechanics of internal fixation of bone. In : An YH, editor. Internal fixation in osteoporotic bone. New York: Thieme Medical Publisher;2002. p. 42–45.
8. Choueka J, Koval KJ, Kummer FJ, Zukerman JD. Cement augmentation of intertrochanteric fracture fixation: a cadaver comparison of 2 techniques. Acta Orthop Scand. 1996; 67:153–157. PMID: 8623570.
9. Gupta RK, Gupta V, Gupta N. Outcomes of osteoporotic trochanteric fractures treated with cement-augmented dynamic hip screw. Indian J Orthop. 2012; 46:640–645. PMID: 23325965.

10. Lee PC, Hsieh PH, Chou YC, Wu CC, Chen WJ. Dynamic hip screws for unstable intertrochanteric fractures in elderly patients--encouraging results with a cement augmentation technique. J Trauma. 2010; 68:954–964. PMID: 20386288.

11. Bartucci EJ, Gonzalez MH, Cooperman DR, Freedberg HI, Barmada R, Laros GS. The effect of adjunctive methylmethacrylate on failures of fixation and function in patients with intertrochanteric fractures and osteoporosis. J Bone Joint Surg Am. 1985; 67:1094–1107. PMID: 4030829.

12. Wu MH, Lee PC, Peng KT, Wu CC, Huang TJ, Hsu RW. Complications of cement augmented dynamic hip screws in unstable type intertrochanteric fractures--a case series study. Chang Gung Med J. 2012; 35:345–353. PMID: 22913862.
13. Boner V, Kuhn P, Mendel T, Gisep A. Temperature evaluation during PMMA screw augmentation in osteoporotic bone--an in vitro study about the risk of thermal necrosis in human femoral heads. J Biomed Mater Res B Appl Biomater. 2009; 90:842–848. PMID: 19353575.
14. Hans DB, Shepherd JA, Schwartz EN, et al. Peripheral dual-energy X-ray absorptiometry in the management of osteoporosis: the 2007 ISCD official positions. J Clin Densitom. 2008; 11:188–206. PMID: 18442759.

Fig. 1
Implant failure due to screw cut out in both extramedullary (A) and intramedullary (B) devices.
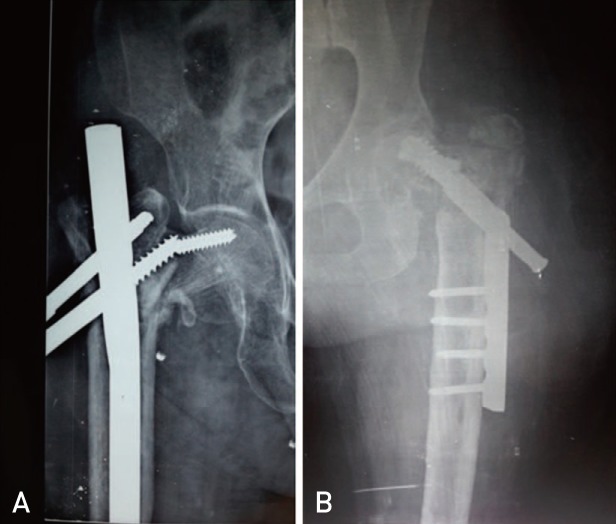
Table 1
Salvati and Wilson Score during Follow Up
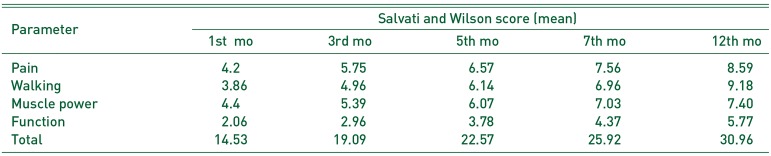
Table 2
Demographics and Functional Outcome in Our Patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download