Abstract
Atypical femoral fractures differ from ordinary femoral diaphyseal or subtrochanteric fractures in several aspects. Although several authors have reported the results of surgical treatment for atypical femoral fractures, the rate of complications (e.g., delayed union, nonunion, fixation failure, and reoperation) is still high. Therefore, we reviewed principles of surgical treatment and describe useful methods for overcoming femoral bowing in these high-risk patients.
Atypical femoral fractures have several clinical characteristics that distinguish them from ordinary femoral fractures12): First, the fracture line must extend from just distal to the lesser trochanter to just proximal to the supracondylar flare. Second, there is no history of trauma, or the injury occurs due to minimal force (e.g., falling from standing height). Lastly, there are a number of representative radiographic findings such as minimal or no comminution with medial spike, transverse or short oblique fracture orientation, localized thickening of the lateral cortex (Fig. 1). The treatment of atypical femoral fractures varies depending on the form of fracture (complete or incomplete), presence of symptoms (pain), and the patient's general condition. Generally, conservative treatment may be attempted for incomplete atypical femoral fractures without pain; however, surgical treatment using an intramedullary nail is required for complete or incomplete fractures with pain3). However, several authors have reported high rates of complications (e.g., delayed union, nonunion, fixation failure, reoperation after surgical treatment) for atypical femoral fractures. Importantly, there are lack of guidelines on the appropriate treatment method for atypical femoral fractures; previous studies have been reported based on the mixture of surgical methods including intramedullary nail and extramedullary devices4567). In addition, most patients with atypical femoral fracture have anterolateral bowing of the femur, increasing the importance of considering that the intramedullary nail may not fit into the femur8).
Therefore, the authors here reviewed the principles of surgical treatment for atypical femoral fracture and described useful methods for overcoming femoral bowing.
An atypical femoral fracture is a form of stress or insufficiency fracture1), and most patients have a history of bisphosphonate administration. In general, complete fractures are healed through endochondral ossification, which, for union of the fractured segments, involves the initial inflammatory, callus formation, and remodeling phases. In contrast, stress fractures heal through the bone remodeling process. Since bisphosphonate does not affect the initial inflammatory and callus formation phases but does suppress the remodeling process of the bone by inhibiting the bone-resorption of osteoclasts, its use in patients should be considered when deciding on the surgical method for atypical femoral fracture91011). It has also been reported that intramedullary nailing is associated with better outcomes than plate fixation because plate fixation has a high rate of surgical failure due to the inhibition of endochondral ossification (Fig. 2)12). However, plate fixation may be considered if an intramedullary nail cannot be used due to a narrow medullary canal (Fig. 3). In addition, since refracture may occur in the area with stress-concentration if a device of insufficient length is used, the femur should be fixed along its full length. The medullary cavity should be reamed at least 2.5 mm greater than the intramedullary nail, in order to insert intramedullary nail conveniently and reduce the occurrence of iatrogenic fracture and malalignment. Furthermore, if the fixation of the distal screw is expected to weaken due to the thin cortical bone of the distal femur, using the Angular Stable Locking System® (ASLS®; Synthes GmbH, Oberdorf, Switzerland) may increase the fixation strength and reduce the risk of secondary loss of reduction.
Although a task force of the American Society for Bone and Mineral Research (ASBMR) recommended full-length reconstruction nail for atypical femoral fractures12), it is a consensus based on the expert opinions as there is a lack of appropriate controlled trials. However, the authors here have experienced secondary femoral neck fracture or new stress fractures around the interlocking screw after using standard interlocking intramedullary nail when treating atypical femoral fractures; thus, we believe using a reconstruction or cephalomedullary nail is the most optimal strategy.
Although in patients without pain, restricting weight bearing may not be necessary, the restriction of excessive activity is recommended until bone edema noted on magnetic resonance imaging examination is resolved. In patients with mild pain, crutches or a walker can be used to restrict weight bearing, and parathyroid hormone could be used when necessary. However, if symptomatic and radiological improvements are not observed following 2 to 3 months of conservative treatment, prophylactic internal fixation is recommended12).
If an incomplete fracture is confirmed radiologically and is accompanied by pain, prophylactic internal fixation using an intramedullary nail is strongly suggested12), and additional research on the appropriate type of internal fixation device is necessary121314).
The general treatment algorithm of atypical femoral fracture based on the fracture pattern (complete or incomplete) and symptoms (presence of pain) is shown in Fig. 4.
The geometry of the lower extremities including the hip joint and proximal femur affects the amount of stress on the lateral femoral cortex15). Atypical femoral fractures are often bilateral, and frequent occurrence in a similar region suggests that the axis of the lower extremities may affect the development of atypical femoral fractures1). There is also a report indicating that patients with low-energy diaphyseal femoral fractures associated with bisphosphonate have greater femoral bowing than age- and gender-matched control patients with no femoral fractures16). In addition, such bowing may also affect surgical treatment, resulting in leg length discrepancy due to lengthening of the operative limb after intramedullary nail fixation (Fig. 5), malalignment during surgery, posteromedial gap of the fracture site, and presence of iatrogenic fracture (Fig. 6). Several surgical recommendations have been reported to overcome anterolateral femoral bowing; these are summarized as follows.
Using the piriformis fossa as an entry point for the intramedullary nail in the case of anterolateral femoral bowing can cause mismatch between alignment of the nail and femur, thus increasing the risk of complications (e.g., malalignment, iatrogenic fracture). In this case, risks can be reduced by creating an entry point at the greater trochanter using an intramedullary nail with a relatively small diameter (Fig. 7). Kim et al.17) reported that, upon comparing the results of using a lateral entry point beginning at the greater trochanter and the original entry point for intramedullary nail insertion in patients with atypical femoral shaft fracture accompanied by severe anterolateral bowing, there was no observed difference in the degree of union, however, the time to union was significantly reduced.
If intramedullary nails with curvature (e.g., Zimmer Natural Nail [ZNN; Zimmer, Warsaw, IN, USA], Expert Asian Femoral Nail [A2FN; Synthes, Solothurn, Switzerland]) are used in patients with anterolateral femoral bowing, a mismatch between alignment of the intramedullary nail and the femur may occur. In such cases, using the opposite side of the intramedullary nail may reduce this risk; however, special caution is needed for the indication of these nails8) (Fig. 8).
Ipsilateral nails with anterior curvature (e.g., ZNN, A2FN) could be inserted with this method in patients with anterolateral femoral bowing. External rotation of the nail with anterior bowing may cause lateral bowing; therefore, it is a useful method in patients with atypical femoral fracture with severe bowing (Fig. 9). When using this method, the nail is inserted with external rotation when the tip of the intramedullary nail is passed through the apex of the femoral bowing. The degree of external rotation could be determined on the basis of the degree of bowing confirmed prior to the surgery. Inserting the interlocking screw may be difficult when using this method (Fig. 10).
This approach may be used in cases wherein intramedullary nail insertion is difficult (e.g., narrow medullary canal, existing metal device). Since the proportion of patients with atypical femoral fracture who used bisphosphonate is high, achieving endochondral ossification would be preferred over osteoclastic remodeling; thus, it is essential that the principle of minimal invasive plate osteosynthesis is followed (Fig. 11).
With the exception of patients with incomplete fracture without pain, most patients with atypical femoral fracture require surgical treatment. Since it is necessary to achieve endochondral ossification due to bisphosphonate use, using a reconstruction or cephalomedullary nail that covers the full length of the femur provides superior outcomes than when using an extramedullary device, and reaming the medullary canal to a diameter of intramedullary nail greater than 2.5 mm is necessary. Due to frequent cases of anterolateral femoral bowing, it is necessary to be well acquainted with the methods of overcoming this situation and important to choose an appropriate method according to the degree of bowing.
Figures and Tables
Fig. 1
Anteroposterior (A) and lateral (B) radiographs of the left femur showing the common characteristics of atypical femoral fractures. 1, Transverse or short oblique fracture line; 2, noncomminuted or minimally comminuted; 3, localized periosteal or endosteal thickening of the lateral cortex; and 4, medial spike.

Fig. 2
Anteroposterior radiographs of subtrochanteric atypical femoral fracture. (A) Preoperative; (B) open reduction and internal fixation with extramedullary device was performed; and (C) fixation failure developed after 4 postoperative months.

Fig. 3
(A, B) Plating may be performed when a nail cannot be used, such as with an extremely narrow intramedullary canal (circle).

Fig. 4
An illustration revealing the treatment algorithm of atypical femoral fractures.
WB: weight bearing.

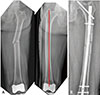
Fig. 5
Anteroposterior radiograph of the right femur (A) after intramedullary nailing reveals straightening of the femur compared with the curved left femur (B).

Fig. 6
Anteroposterior radiographs of pre-operation (A) and post-operation (B) reveal the iatrogenic fracture (arrow) due to mismatch between femoral bowing and intramedullary nail.

Fig. 7
(A) Radiographs of both femurs showing right diaphyseal atypical femoral fracture and a bowed left femur. (B) Postoperative radiograph revealing the far lateral entry point of the standard interlocking nail. (C) Radiograph obtained 4 months after surgery showing progression of union.
Fig. 8
(A) Radiographs of both femurs showing left diaphyseal atypical femoral fracture and bowed right femur. (B) Intramedullary nail on the opposite (right) side was used for overcoming the mismatch.
References
1. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23.

2. Lee KJ, Min BW, Song KS, Bae KC, Cho CH, Lee SW. T-Score discordance of bone mineral density in patients with atypical femoral fracture. J Bone Joint Surg Am. 2017; 99:1683–1688.

3. Al-Ashqar M, Panteli M, Chakrabarty G, Giannoudis PV. Atypical fractures: an issue of concern or a myth? Injury. 2018; 49:649–655.

4. Weil YA, Rivkin G, Safran O, Liebergall M, Foldes AJ. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma. 2011; 71:186–190.

5. Teo BJ, Koh JS, Goh SK, Png MA, Chua DT, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. Bone Joint J. 2014; 96-B:658–664.

6. Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res. 2012; 470:2295–2301.

7. Lee KJ, Yoo JJ, Oh KJ, et al. Surgical outcome of intramedullary nailing in patients with complete atypical femoral fracture: a multicenter retrospective study. Injury. 2017; 48:941–945.

8. Park JH, Lee Y, Shon OJ, Shon HC, Kim JW. Surgical tips of intramedullary nailing in severely bowed femurs in atypical femur fractures: simulation with 3D printed model. Injury. 2016; 47:1318–1324.

9. Hauser M, Siegrist M, Keller I, Hofstetter W. Healing of fractures in osteoporotic bones in mice treated with bisphosphonates - a transcriptome analysis. Bone. 2018; 112:107–119.

10. Cao Y, Mori S, Mashiba T, et al. Raloxifene, estrogen, and alendronate affect the processes of fracture repair differently in ovariectomized rats. J Bone Miner Res. 2002; 17:2237–2246.

11. Martinez MD, Schmid GJ, McKenzie JA, Ornitz DM, Silva MJ. Healing of non-displaced fractures produced by fatigue loading of the mouse ulna. Bone. 2010; 46:1604–1612.

12. Shane E, Burr D, Ebeling PR, et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2010; 25:2267–2294.

13. Ha YC, Cho MR, Park KH, Kim SY, Koo KH. Is surgery necessary for femoral insufficiency fractures after long-term bisphosphonate therapy? Clin Orthop Relat Res. 2010; 468:3393–3398.

14. Demiralp B, Ilgan S, Ozgur Karacalioglu A, Cicek EI, Yildrim D, Erler K. Bilateral femoral insuffiency fractures treated with inflatable intramedullary nails: a case report. Arch Orthop Trauma Surg. 2007; 127:597–601.

15. Crossley K, Bennell KL, Wrigley T, Oakes BW. Ground reaction forces, bone characteristics, and tibial stress fracture in male runners. Med Sci Sports Exerc. 1999; 31:1088–1093.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download