Abstract
Purpose
Since a patient's obesity can affect the mortality and morbidity of the surgery, less drastic surgeries may have a major benefit for obese individuals. This study evaluated the feasibility of performing a totally laparoscopic distal gastrectomy, with intracorporeal anastomosis, in obese patients suffering from gastric cancer.
Materials and Methods
This was a retrospective analysis of the 138 patients, who underwent a totally laparoscopic distal gastrectomy from April 2005 to March 2009, at the National Kyushu Cancer Center. The body mass index of 20 patients was ≥25, and in 118 patients, it was <25 kg/m2.
Results
The mean values of body mass index in the 2 groups were 27.3±2.2 and 21.4±2.3. Hypertension was significantly more frequent in the obese patients than in the non-obese patients. The intraoperative blood loss, duration of surgery, post-operative complication rate, post-operative hospital stay, and a number of retrieved lymph nodes were not significantly different between the two groups.
In Japan, laparoscopy-assisted gastrectomy and lymph node dissection with curative intent have been recommended and practiced for the treatment of early gastric cancers since the first report in 1994 of a laparoscopy-assisted distal gastrectomy (LADG) with a Billroth I anastomosis for a patient with gastric cancer.(1) Obesity is associated with the mortality and morbidity of a gastrectomy in open surgery.(2-5) Obesity might increase the rate of intra-operative or post-operative complications. Therefore, less invasive surgery, such as an LADG, may have a greater impact in the obese patients by reducing the rate of complications, length of the hospital stay, and permitting a more rapid return to physical activities. There have been a few studies that have investigated the impact of obesity on laparoscopy-assisted distal gastrectomy.(6-8) These reports have shown technical difficulties and a longer duration of surgery in the obese patients.
A totally laparoscopic distal gastrectomy (TLDG) is defined as a method used to perform both the resection and anastomosis intracorporeally with a laparoscopic technique. TLDG has several advantages over LADG including smaller wounds, less invasiveness, and a greater chance of a secure ablation.(9) However, the introduction of TLDG for all people still remains controversial, since it is generally believed that the time required for a TLDG is longer and the surgical procedure is more difficult than for a LADG. This study compared the factors associated with the outcome of a TLDG in obese patients and non-obese patients to elucidate the safety and advantages for the obese patients.
One hundred thirty-eight patients underwent a TLDG for gastric cancer in the National Kyushu Cancer Center in Japan between April 2005 and March 2009. A TLDG was performed in patients with T1N0M and T2N0M0 gastric cancer regardless of their gender, age, body mass index (BMI) or comorbidities. The patients were divided into two groups, consisting of obese and non-obese patients, according to the obesity criteria recommended by the Japan Society of Obesity. The BMI in the non-obese group was <25.0 (n=118); in the obese group, the BMI was ≥25.0 (n=20). The concurrent diseases, duration of surgery, blood loss, hospital stay and post-operative morbidity were compared in the two groups. Information was collected from the medical records and anesthesia records including age, gender, duration of surgery, estimated blood loss, blood test data, lung function tests, pathological findings and post-operative complications or parenteral nutritional support.
The distal gastrectomy and lymph node dissection were performed according to the guideline of the Japanese Gastric Cancer Association.(10) The patient was placed under general anesthesia in the supine position. A 12-mm trocar was inserted in the umbilical region using a cut-down method. A laparoscope was inserted through the trocar and the liver was pulled up using a Penrose drain and a J-shaped retractor.(11) The detailed surgical procedure of the TLDG was reported previously.(9,11) The distal stomach was removed and reconstructed using the Billroth I or Roux-en Y method. Billroth I reconstruction was performed with a delta-shaped anastomosis(12) and Roux-en Y reconstruction was also performed using a linear stapler.(13) Both anastomoses were completed intracorporeally.
Intraoperative complications were defined as conditions that required either an open conversion or additional procedures to the planned surgery for any reason. Post-operative minor complications were defined as any abdominal finding during the post-operative course not requiring medication or a systemic complication requiring pharmacologic treatment. Major post-operative complications were defined as any complication requiring surgical or radiological intervention.
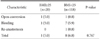
The characteristics of the 138 patients are summarized in Table 1. The mean values of BMI in the 2 groups were 27.3±2.2 and 21.4±2.3, respectively, for obese and non-obese patients. The gender and age, stage of gastric cancer, extent of lymph node dissection and type of reconstruction were not significantly different between the two groups. In addition, the vital capacity and the ratio of the forced expiratory volume in one second, the hemoglobin and the albumin levels were not significantly different in two groups. A severe comorbidity (American Society of Anesthesiologists class 3) was present in 11 patients in the non-obese group and one patient in the obese group. Table 1 shows the pre-operative concurrent diseases in both groups. The most frequent concurrent disease in both groups was hypertension, and the incidence of hypertension was significantly more frequent in the obese patients than in the non-obese patients.
No significant differences were observed regarding the operation time, estimated blood loss, number of retrieved lymph nodes, the value of C-reactive protein 7 days after the operation and post-operative hospital stay (Table 2) between the two groups. Table 3 and 4 summarize the peri-operative complications in univariate analysis. Each group had one conversion case from a laparoscopic gastrectomy to an open gastrectomy. Unexpected bleeding occurred in 8 cases. Post-operative complications were categorized into minor or major complications. No significant differences were noted between the two groups in the incidence of major complications such as anastomotic leakage, anastomotic bleeding and colon injury. Six major factors associated with peri- or post-operative complications were selected for the multivariate analysis. None of the factors significantly increased in the high BMI cases (Table 5).
A laparoscopic distal gastrectomy (LDG) is generally used for the treatment of gastric cancer, since this type of surgery has demonstrated benefits over open surgery.(1,14) Many surgeons expected that the laparoscopic approach for gastric surgery would improve the morbidity and mortality for high risk patients in comparison to open surgery. However, the advantages for high risk patients, such as the obese, elderly and patients with low respiratory function are still controversial. Some previous studies have suggested that there is no difference in the post-operative morbidity and mortality between obese and non-obese patients associated with LDG for gastric cancer.(6-8,15,16) However, a longer duration of surgery and more difficult operations have been reported for obese patients.(7,8)
Recently, a TLDG has been used for the treatment of gastric cancer.(9,17,18) TLDG is a method in which both the resection and anastomosis are performed intracorporeally using laparoscopic procedures. Previous studies have shown favorable results with TLDG and demonstrated this approach with lymph node dissection to be technically feasible, and it is thus considered to be an effective surgical modality for gastric cancer without a high morbidity rate. In this report, we retrospectively compared the factors associated with the outcome of a TLDG in obese patients and non-obese patients to elucidate the safety and advantages for the obese patients. We found no significant differences between the two groups in terms of the duration of surgery, bleeding and post-operative complications.
The most important problem resulting from the laparoscopic surgery for obese patient was anastomosis. The anastomosis is performed in the abdominal cavity in TLDG, and excessive torsion is not applied to the remnant stomach and duodenum. Therefore, no extension of the wound or minilaparotomy is usually necessary. This made the anastomois simple and easy. Therefore, anastomosis-related complications are rarely observed. Wound infections may be more frequent in obese patients.(19,20) The risk for wound infection also decreases following the TLDG procedure because of the smaller wound.
In open surgery, it has been reported that the number of retrieved lymph nodes for gastrectomy with D2 resection was not affected by obesity.(21) On the other hand, another report showed that the number of examined lymph nodes was affected by obesity.(22) Laparoscopic surgery has advantages for minute surgical procedures, such as lymph node dissection, however it is controversial whether the number of retrieved lymph nodes is influenced by obesity or not when using this procedure.(6,15) In our investigation, the duration of surgery and the number of retrieved lymph nodes was not different between obese and non-obese patients. The average number of retrieved lymph nodes in obese patients was 30.8±16.2 and that in non obese patients were 32.7±15.0. Laparoscopic surgery therefore seems to be more suitable for lymph node dissection because of the magnification of the field of vision, even for obese patients.
In conclusion, the TLDG is therefore considered to be a safe and effective procedure for obese patients since there were no differences in the duration of surgery, estimated blood loss, and rate of complications, in spite of the difference in the patients' background. This method can therefore be recommended as a standard treatment for obese patients.
Figures and Tables
Table 1
Clinicopathologic characteristics of patients who underent totally laparoscopic distal gastrectomy

References
1. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994. 4:146–148.
2. Bittner R, Butters M, Ulrich M, Uppenbrink S, Beger HG. Total gastrectomy. Updated operative mortality and long-term survival with particular reference to patients older than 70 years of age. Ann Surg. 1996. 224:37–42.
3. Eguchi T, Fujii M, Takayama T. Mortality for gastric cancer in elderly patients. J Surg Oncol. 2003. 84:132–136.

4. Mochiki E, Ohno T, Kamiyama Y, Aihara R, Nakabayashi T, Asao T, et al. Laparoscopy-assisted gastrectomy for early gastric cancer in young and elderly patients. World J Surg. 2005. 29:1585–1591.

5. Wu CW, Hsieh MC, Lo SS, Wang LS, Hsu WH, Lui WY, et al. Morbidity and mortality after radical gastrectomy for patients with carcinoma of the stomach. J Am Coll Surg. 1995. 181:26–32.
6. Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Effect of obesity on technical feasibility and postoperative outcomes of laparoscopy-assisted distal gastrectomy--comparison with open distal gastrectomy. J Gastrointest Surg. 2008. 12:997–1004.

7. Yasuda K, Inomata M, Shiraishi N, Izumi K, Ishikawa K, Kitano S. Laparoscopy-assisted distal gastrectomy for early gastric cancer in obese and nonobese patients. Surg Endosc. 2004. 18:1253–1256.

8. Noshiro H, Shimizu S, Nagai E, Ohuchida K, Tanaka M. Laparoscopy-assisted distal gastrectomy for early gastric cancer: is it beneficial for patients of heavier weight? Ann Surg. 2003. 238:680–685.
9. Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009. 23:2374–2379.

10. Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma. 1999. 13th edition. Tokyo: Kanehara publishing;(Japanese).
11. Sakaguchi Y, Ikeda O, Toh Y, Aoki Y, Harimoto N, Taomoto J, et al. New technique for the retraction of the liver in laparoscopic gastrectomy. Surg Endosc. 2008. 22:2532–2534.

12. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002. 195:284–287.

13. Takaori K, Nomura E, Mabuchi H, Lee SW, Agui T, Miyamoto Y, et al. A secure technique of intracorporeal Roux-Y reconstruction after laparoscopic distal gastrectomy. Am J Surg. 2005. 189:178–183.

14. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002. 131:S306–S311.

15. Kim KH, Kim MC, Jung GJ, Kim HH. The impact of obesity on LADG for early gastric cancer. Gastric Cancer. 2006. 9:303–307.

16. Lee HJ, Kim HH, Kim MC, Ryu SY, Kim W, Song KY, et al. Korean Laparoscopic Gastrointestinal Surgery Study Group. The impact of a high body mass index on laparoscopy assisted gastrectomy for gastric cancer. Surg Endosc. 2009. 23:2473–2479.

17. Guzman EA, Pigazzi A, Lee B, Soriano PA, Nelson RA, Benjamin Paz I, et al. Totally laparoscopic gastric resection with extended lymphadenectomy for gastric adenocarcinoma. Ann Surg Oncol. 2009. 16:2218–2223.

18. Huscher CG, Mingoli A, Sgarzini G, Brachini G, Binda B, Di Paola M, et al. Totally laparoscopic total and subtotal gastrectomy with extended lymph node dissection for early and advanced gastric cancer: early and long-term results of a 100-patient series. Am J Surg. 2007. 194:839–844.

19. Barber GR, Miransky J, Brown AE, Coit DG, Lewis FM, Thaler HT, et al. Direct observations of surgical wound infections at a comprehensive cancer center. Arch Surg. 1995. 130:1042–1047.

20. Tsukada K, Miyazaki T, Kato H, Masuda N, Fukuchi M, Fukai Y, et al. Body fat accumulation and postoperative complications after abdominal surgery. Am Surg. 2004. 70:347–351.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download