Abstract
Purpose
It has been reported that children with hypopituitarism have features of metabolic syndrome, including obesity, impaired glucose tolerance, and dyslipidemia. The aim of this study was to investigate the clinical features and liver histology of pediatric non-alcoholic fatty liver disease (NAFLD) associated with hypopituitarism.
Methods
We reviewed the clinical data of 11 children diagnosed with NAFLD among patients with hypopituitarism.
Results
The mean age at the time of diagnosis of hypopituitarism was 10.4±3.2 years, and the mean age at the time of diagnosis of NAFLD was 13.1±2.7 years. A craniopharyngioma was the most common cause of pituitary dysfunction. At the time of diagnosis of NAFLD, 9 patients (82%) had a body mass index greater than the 85th percentile, 5 patients (45%) had elevated fasting blood glucose levels, and 9 patients (82%) had hypertriglyceridemia. The mean height SD score was significantly lower at the time of diagnosis of NAFLD than at the time of diagnosis of hypopituitarism. Of the six patients who were biopsied, one had cirrhosis, two had non-alcoholic steatohepatitis (NASH) with bridging fibrosis, two had NASH with mild portal fibrosis, and one had simple steatosis.
With the increasing prevalence of pediatric obesity, nonalcoholic fatty liver disease (NAFLD) has become a common cause of chronic liver disease in the preadolescent and adolescent age groups1). The spectrum of NAFLD extends from simple steatosis to nonalcoholic steatohepatitis (NASH) and cirrhosis. NASH is defined as a fatty liver disease that causes liver inflammation and varying degrees of hepatic fibrosis. Simple steatosis has a relatively benign course, whereas NASH can progress to cirrhosis2). NAFLD is associated with abdominal obesity, insulin resistance and features of metabolic syndrome 3).
Children and adolescents with hypopituitarism have features of metabolic syndrome, including obesity, insulin resistance and dyslipidemia4). Adults with hypothalamic and pituitary dysfunction are at risk of developing NAFLD with cirrhosis, which increases the risk of liver-related death5,6). A few case reports have described the development of NASH in children with panhypopituitarism 7~11). We investigated the clinical features and liver histology of pediatric NAFLD associated with hypopituitarism.
Children included in this study were diagnosed as having NAFLD among patients with hypopituitarism at the Seoul National University Children's Hospital between January 2000 and July 2009. All subjects were diagnosed with NAFLD after exclusion of other causes of chronic hepatitis, including hepatitis A, B, and C viruses, autoimmune hepatitis, Wilson's disease, drug toxicity, total parenteral nutrition and chronic alcohol intake. Diagnosis of NAFLD was based on evidence of a fatty liver from a percutaneous liver biopsy or abdominal computerized tomography (CT). Fatty liver was diagnosed from unenhanced CT images when the liver minus spleen attenuation difference was less than or equal to -10 H. Percutaneous liver biopsy was performed in 6 patients. Approval for this study was obtained from the Ethical Committee of the Seoul National University Hospital, and all patients or responsible guardians provided written informed consent.
Height, weight, serum concentrations of aspartate aminotransferase (AST), alanine aminotransferase (ALT) and glucose and lipid profiles were measured. Body mass index (BMI) was calculated as weight (kg) divided by the height (m) squared. Obesity was defined as a BMI>95th percentile, adjusted for age and sex; overweight was defined as a BMI between the 85th and 95th percentiles.
Fasting hypertriglyceridemia was defined as a serum triglyceride level >110 mg/dL. Fasting hyperinsulinemia was defined as a serum insulin level >20µIU/mL.
In childhood, GH deficiency was diagnosed if the GH peak was less than 5µg/L on two provocative tests using L-dopa, clonidine, glucagon or insulin. We performed GH stimulation test 1 year after completion of tumor therapy. If parents agreed to receive the GH, we started GH treatment in a dose of 15 IU/m2 per week. We reassessed GH secretion using insulin in adolescents who attained the final height. If peak GH concentration was less than 3µg/L, childhood-onset adult GH deficiency was diagnosed and GH was administered in a dose of 0.006~0.012 mg/kg per day.
Secondary hypoadrenalism was diagnosed if peak cortisol less than 18µg/dL after insulin-induced hypoglycemia or blunted ACTH response after corticotrophin-releasing hormone administration. TSH deficiency was defined by low free T4 level without appropriate elevation of TSH after thyrotropin-releasing hormone administration. Hypogonadotropic hypogonadism was defined by low sex steroid level without appropriate LH/FSH elevation after gonadotropin releasing hormone administration after the age of 10 years (female) or 12 years (male).
Liver biopsy specimens were evaluated according to the classification of Brunt et al12).
Of the 11 children, seven were male. The mean age at the time of diagnosis of hypopituitarism was 10.4±3.2 years and the mean age at the time of diagnosis of NAFLD was 13.1±2.7 years.
Craniopharyngioma was the most common cause of pituitary dysfunction, affecting seven patients (64%). Two patients had germ cell tumors, one had a medulloblastoma and one had idiopathic hypopituitarism. All patients with tumors underwent surgery, three of whom received additional radiotherapy and chemotherapy. All patients were diagnosed with hypoadrenalism and hypothyroidism and received Levo-thyroxine and hydrocortisone with a dose of less than 12 mg/m2. Desmopressin was administered to eight patients. All patients presented with childhood-onset GH deficiency. Five children were treated with GH in their childhood. GH was not administered to six children (residual tumor mass in 2 children, parental refusal in 2, maintenance of linear growth in 1, attainment of the final adult height in 1).
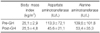
At the time of diagnosis of hypopituitarism, five patients (41%) had a BMI greater than the 85th percentile. At the time of diagnosis of NAFLD, nine patients (82%) had a BMI greater than the 85th percentile. Six patients were overweight and three were obese. The mean height SD score was significantly lower at the time of diagnosis of NAFLD (-1.47±1.81) than at the time of diagnosis of hypopituitarism (-0.89±1.16). NAFLD was diagnosed 2.7±2.7 years after the diagnosis of hypopituitarism (Table 1). At the time of diagnosis of hypopituitarism, liver enzyme levels were available for nine patients, five of whom had levels within the normal range. All patients except one had developed elevated liver enzymes by the time of diagnosis of NAFLD (Table 2).
Fasting blood glucose level at the time of diagnosis of hypopituitarism was elevated in one patient. At the time of diagnosis of NAFLD, fasting blood glucose level was elevated in five patients (45%), of whom two had diabetes mellitus and three had glucose intolerance (fasting glucose>110 mg/dL). At the time of diagnosis of NAFLD, fasting triglyceride levels were elevated in nine patients (82%). At the time of diagnosis of NAFLD, acanthosis nigricans was observed in three patients and fasting insulin levels were elevated in four patients (Table 2).
Six patients were diagnosed with NAFLD from liver biopsy results. One patient was cirrhotic (Fig. 1A), two had NASH with bridging fibrosis (Fig. 1B), two had NASH with mild portal fibrosis and one had simple steatosis. Two with bridging fibrosis had short statures (height SD score less than -2.0) and fasting hyperinsulinemia; one had diabetes. One cirrhotic patient had idiopathic hypopituitarism, which was diagnosed at age 11. He had severe growth retardation, early-onset severe obesity and diabetes mellitus. He is now in a vegetative state because of intracerebral hemorrhage. Three patients with no fibrosis or mild fibrosis had normal fasting insulin levels.
The childhood-onset adult GH deficiency was detected in seven adolescents who attained the final adult height. GH replacement therapy was administered to these adolescents. Serum AST level in adolescents with childhood-onset adult GH deficiency decreased from 113.3±72.1 IU/L to 45.6±21.1 IU/L after GH therapy (p<0.05). Serum ALT level decreased significantly from 139.6±101.8 IU/L to 53.4±35.3 IU/L after GH therapy. There was no significant change in mean BMI (25.1±2.9 vs. 25.5±4.8) after GH therapy (Table 3).
An extreme degree of obesity may develop in association with a hypothalamic tumor. Hypothalamic damage resulting from a tumor, surgery, or radiation is the primary cause of obesity in survivors of childhood brain tumors13). In this study, craniopharyngioma was the most common cause of NAFLD associated with hypopituitarism. Of all childhood brain tumors, craniopharyngioma is associated with the highest risk of obesity. Approximately 50% of children who are surgically treated for craniopharyngioma are obese at follow-up14).
Adults with GH deficiency, with or without hypopituitarism, have features of metabolic syndrome, including excess abdominal adiposity, insulin resistance and dyslipidemia 15,16). Kaji et al. reported that NAFLD was the third most common complication after hypercholesterolemia and hypertriglyceridemia in adults with GH deficiency17). Children who develop hypopituitarism after craniopharyngioma surgery also have features of metabolic syndrome, including high abdominal fat and hypertriglyceridemia 4). In this study, nine (82%) of 11 children were overweight or obese at the time of diagnosis of NAFLD. Hypertriglyceridemia and fasting hyperinsulinemia were detected in nine (82%) and four (36%) children, respectively. The mean interval between diagnosis of hypopituitarism and development of NAFLD was 2.7 years, which is shorter than the 6.4-year interval reported by Adams et al. for a group that included adults. They described 21 patients with hypothalamic or pituitary dysfunction that was accompanied by excessive weight gain, impaired glucose tolerance, dyslipidemia and NAFLD. Biopsies were taken from 10 patients, of whom six had cirrhosis5). Previously we reported that the prevalence of advanced fibrosis was 8.8% in children with NAFLD associated with simple obesity18). So we believed that the liver disease was more severe in children with NAFLD associated with hypopituitarism; 50% of the patients biopsied had advanced fibrosis in this study.
In this study, children with bridging fibrosis or cirrhosis had short statures and fasting hyperinsulinemia. This suggests that GH deficiency and insulin resistance may play an important role in the progression of NASH. The hepatic effects of hypothalamic and pituitary diseases seem to be primarily mediated by GH deficiency. The metabolic effects and subsequent development of obesity that occur in GH-deficient individuals result in the development of NASH19). Patients with NASH demonstrate similarities to those with adult GH deficiency and patients with NAFLD have lower GH levels compared with controls20). Adult patients with anterior pituitary dysfunction and GH deficiency have hepatic steatosis more frequently than those with anterior pituitary deficiency without GH deficiency, which indicates that GH deficiency is a risk factor for NAFLD21). GH replacement reduces total body fat and normalizes insulin sensitivity in GH-deficient adults16).
Fukuda et al. demonstrated that 29% of adults who had been diagnosed with childhood-onset GH deficiency developed NAFLD within 21 years of discontinuation of GH therapy. They suggested that lifelong GH replacement might be important for improving the overall metabolic profile22). There is a case report of an adult with hypopituitarism who suffered from NAFLD, which improved with GH treatment9). Administration of GH replacement therapy to an adult patient with hypopituitarism reversed steatosis, inflammation and fibrosis in the liver according to histology23). This improvement was associated with a marked reduction in oxidative stress in the liver, suggesting that GH plays an essential role in metabolic and redox regulation in the liver, which is consistent with previous findings showing that GH replacement therapy reduced free radical levels24).
In the present study, GH therapy improved liver dysfunction, but had no salutary effect on BMI. This finding suggests that GH may affect metabolic profiles directly rather than indirectly via weight reduction. However, liver histology between pre- and post-GH treatment was not compared. Further studies are necessary to determine whether GH replacement will ameliorate the degree of fibrosis or steatosis.
Hypothyroidism induces dyslipidemia and obesity, and can lead to the development of NASH25). All of our patients received thyroid hormones after the diagnosis of hypopituitarism and had normal thyroid function tests. The development of NAFLD is less likely associated with hypothyrodism in this study.
In conclusion, children with hypopituitarism are at risk of short stature, obesity, dyslipidemia and NAFLD. Early diagnosis of NAFLD is important in children with hypopituitarism because advanced fibrosis is common. The role of GH in the development of NAFLD in patients with hypopituitarism remains to be investigated.
Figures and Tables
Fig. 1
Liver histologic findings show micro-nodular cirrhotic changes (A) and bridging fibrosis (B) (H&E, ×200).

References
1. Patton HM, Sirlin C, Behling C, Middleton M, Schwimmer JB, Lavine JE. Pediatric nonalcoholic fatty liver disease: a critical appraisal of current data and implications for future research. J Pediatr Gastroenterol Nutr. 2006. 43:413–427.
2. Hubscher SG. Histological assessment of non-alcoholic fatty liver disease. Histopathology. 2006. 49:450–465.

3. Manco M, Marcellini M, Devito R, Comparcola D, Sartorelli MR, Nobili V. Metabolic syndrome and liver histology in paediatric non-alcoholic steatohepatitis. Int J Obes (Lond). 2008. 32:381–387.

4. Srinivasan S, Ogle GD, Garnett SP, Briody JN, Lee JW, Cowell CT. Features of the metabolic syndrome after childhood craniopharyngioma. J Clin Endocrinol Metab. 2004. 89:81–86.

5. Adams LA, Feldstein A, Lindor KD, Angulo P. Nonalcoholic fatty liver disease among patients with hypothalamic and pituitary dysfunction. Hepatology. 2004. 39:909–914.

6. Lee HH, Byun YH, Shin WY, Kim SH, Song MH, Jo YJ, et al. A case of cryptogenic liver cirrhosis with hypopituitarism. Korean J Med. 2007. 72:S116–S120.
7. Altuntas B, Ozcakar B, Bideci A, Cinaz P. Cirrhotic outcome in patients with craniopharyngioma. J Pediatr Endocrinol Metab. 2002. 15:1057–1058.
8. Basenau D, Stehphani U, Fischer G. Development of complete liver cirrhosis in hyperphagia-induced fatty liver. Klin Padiatr. 1994. 206:62–64.
9. Takano S, Kanzaki S, Sato M, Kubo T, Seino Y. Effect of growth hormone on fatty liver in panhypopituitarism. Arch Dis Child. 1997. 76:537–538.

10. Nakajima K, Hashimoto E, Kaneda H, Tokushige K, Shiratori K, Hizuka N, et al. Pediatric nonalcoholic steatohepatitis associated with hypopituitarism. J Gastroenterol. 2005. 40:312–315.

11. Park JY, Ko JS, Seo JK, Lee R, Shin CH, Kang GH, et al. Nonalcoholic fatty liver disease progressing to cirrhosis in an obese boy with hypopituitarism. Korean J Pediatr Gastroenterol Nutr. 2008. 11:204–209.

12. Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999. 94:2467–2474.

13. Lustig RH, Post SR, Srivannaboon K, Rose SR, Danish RK, Burghen GA, et al. Risk factors for the development of obesity in children surviving brain tumors. J Clin Endocrinol Metab. 2003. 88:611–616.

14. Muller HL, Bueb K, Bartels U, Roth C, Harz K, Graf N, et al. Obesity after childhood craniopharyngioma--German multicenter study on pre-operative risk factors and quality of life. Klin Padiatr. 2001. 213:244–249.

15. Johansson JO, Fowelin J, Landin K, Lager I, Bengtsson BA. Growth hormone-deficient adults are insulin-resistant. Metabolism. 1995. 44:1126–1129.

16. Hwu CM, Kwok CF, Lai TY, Shih KC, Lee TS, Hsiao LC, et al. Growth hormone (GH) replacement reduces total body fat and normalizes insulin sensitivity in GH-deficient adults: a report of one-year clinical experience. J Clin Endocrinol Metab. 1997. 82:3285–3292.

17. Kaji H, Sakurai T, Iguchi G, Murata M, Kishimoto M, Yoshioka S, et al. Adult growth hormone deficiency in Japan: results of investigation by questionnaire. Endocr J. 2002. 49:597–604.

18. Ko JS, Yoon JM, Yang HR, Myung JK, Kim HR, Kang GH, et al. Clinical and histological features of nonalcoholic fatty liver disease in children. Dig Dis Sci. 2009. 54:2225–2230.

19. Loria P, Carulli L, Bertolotti M, Lonardo A. Endocrine and liver interaction: the role of endocrine pathways in NASH. Nat Rev Gastroenterol Hepatol. 2009. 6:236–247.

20. Lonardo A, Loria P, Leonardi F, Ganazzi D, Carulli N. Growth hormone plasma levels in nonalcoholic fatty liver disease. Am J Gastroenterol. 2002. 97:1071–1072.

21. Ichikawa T, Hamasaki K, Ishikawa H, Ejima E, Eguchi K, Nakao K. Non-alcoholic steatohepatitis and hepatic steatosis in patients with adult onset growth hormone deficiency. Gut. 2003. 52:914.

22. Fukuda I, Hizuka N, Yasumoto K, Morita J, Kurimoto M, Takano K. Metabolic co-morbidities revealed in patients with childhood-onset adult GH deficiency after cessation of GH replacement therapy for short stature. Endocr J. 2008. 55:977–984.

23. Takahashi Y, Iida K, Takahashi K, Yoshioka S, Fukuoka H, Takeno R, et al. Growth hormone reverses nonalcoholic steatohepatitis in a patient with adult growth hormone deficiency. Gastroenterology. 2007. 132:938–943.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download