Abstract
This report details a case of post-traumatic pseudocyst in the spleen that was successfully treated with sclerotherapy using ethanol. A sixteen-year-old boy visited our hospital for a follow-up examination of a splenic cyst. He had experienced blunt trauma to the abdomen three years prior to presentation. An abdominal computed tomography scan revealed a large cyst of the lower pole of the spleen. The cyst was 6.8×9.5×7.0 cm and conservative management was tried. A follow-up ultrasonographic examination three years later revealed that the size of the cyst was unchanged and another treatment was needed to prevent complications. One session of sclerosis with ethanol (90 mL of 99% ethanol) percutaneously was applied to the cyst. A follow-up after four months revealed that the cyst had completely resolved.
The spleen is the most frequently affected organ in abdominal trauma. Large cysts of the spleen are uncommon and usually develop following blunt abdominal trauma [1]. Splenic cystic masses are rarely symptomatic. However, they should be treated because they can develop complications such as rupture, bleeding or infection [23].
Splenectomy was the treatment of choice for splenic cysts [4]. Because of the immunologic role of the spleen, new surgical approaches, such as laparoscopic surgery, partial splenectomy, decapsulation and unroofing, have been proposed [5]. Recently, conservative treatment using percutaneous aspiration of the cyst contents with or without instillation of sclerosing agents has been generally accepted [6]. High success rates of alcoholic sclerotherapy in patients with renal and hepatic cysts have been reported [789]. However, there are contradictory reports regarding congenital splenic cysts treated with percutaneous sclerosis using alcohol [610]. The optimal treatment of post-traumatic splenic pseudocysts is not well defined.
We present an adolescent patient with post-traumatic pseudocyst in the spleen, which was treated percutaneously using alcohol as the sclerosing agent.
A sixteen-year-old boy visited our hospital for a follow-up examination of a splenic cyst. He did not complain of any symptoms related to the cyst. Initial laboratory findings are as follows; white blood cell (WBC) 5,710/mm3, aspartate aminotransferase/alanine aminotransferase 16/12 IU/L, total bilirubin 0.4 mg/dL, albumin 4.5 g/dL, amylase/lipase 104/19 IU/L. He had experienced a blunt trauma to the abdomen three years prior to presentation. At that time, he had received emergent laparotomy at another hospital to find out the cause of abdominal pain and was diagnosed as having a splenic cyst in the lower pole of the spleen and hemoperitoneum. The cyst was 6.8×9.5×7.0 cm and asymptomatic (Fig. 1). Conservative management was tried. However, a follow-up ultrasonographic examination three years later revealed that the size of the cyst was unchanged (Fig. 2A) and other treatment options were needed to prevent complications.
The mass was punctured with an 18 G needle under ultrasound guidance, and 170 mL of yellowish serous fluid aspirated. A contrast medium was injected through a pig-tail catheter. The cyst did not have any contact with any other space and had a smooth wall (Fig. 2B). The results of analysis of the aspirated fluid are as follows; pH 8.0, WBC 26/mm3 (lymphocyte 27%, eosinophil 11%, macrophage 61%, neutrophil 1%), glucose 65 mg/dL, total protein 9.6 g/dL, lactic dehydrogenase 590 IU/L. A microbiologic culture of aspirated fluid was sterile. Then 90 mL of ethanol (99%) was injected into the cyst. Two hours later the fluid in the cyst was completely evacuated and the catheter was removed.
Ten days later, an ultrasound showed that the size of the cyst was half of its original size (Fig. 3A). After four months, the ultrasound could no longer detect the cyst and showed a small solid-like lesion (Fig. 3B). One session of sclerosis with ethanol had succeeded in obliterating the cyst. There were no other complications.
Post-traumatic splenic cysts are rare and their true incidence is not known. There may have been an increase in the reported incidence of splenic pseudocysts due to their increased detection through the routine use of computed tomography (CT) scans and ultrasounds. Splenic cysts after trauma can be formed by the encapsulation of a hematoma. Subsequently, the pigment can be absorbed, leading to a serous cyst [11].
Between 30% and 60% of patients do not experience symptoms of post-traumatic pseudocyst [2]. Symptoms can develop when the size of the cyst increases and are related to the compression of adjacent organs, such as the stomach, diaphragm, and kidney [12]. Vascular compression of the portal vein and renal artery results in hypertension [1314]. Diagnosis can be made by evaluating the history of blunt trauma to the abdomen, upper abdominal pain, and conducting imaging studies such as an abdominal CT scan or ultrasound.
In our case study, the patient had had a chronic but asymptomatic post-traumatic splenic pseudocyst for the past three years. The cyst was filled with serous fluid resulting from the absorption of the blood's pigment. The authors decided to take a percutaneous approach when treating the cyst to prevent complications because the patient had already undergone significant abdominal surgery.
Splenic preservation has become the standard treatment for blunt trauma to the spleen [15]. Although a variety of spleen-preserving surgical treatments have been reported in the recent literature [511], there have been many limitations, such as a high recurrence rate of cysts, technical difficulties and difficulty controlling bleeding. Schier et al. [5] suggested that surgical treatment could be considered in case of larger cysts greater than 10 cm and cysts causing symptoms. Recently, Wu and Kortbeek [11] suggested conflicting claims that partial or complete splenectomy should be considered for young and otherwise healthy patients who have large symptomatic splenic pseudocysts.
Several types of sclerosing agents for the percutaneous therapy have been used including formalin, glucose, pantopaque, phenol, and tetracycline or doxycycline [16]. However, all these agents have disadvantages such as a high recurrence rate or toxicity. Ethanol is also a toxic agent, but its successful use as a sclerosing agent in hepatic cysts [8], renal cysts [7], hydatid cysts of the liver [9], postoperative lymphoceles [17], and symptomatic polycystic liver disease [18] has suggested that it could be useful in the treatment of a post-traumatic splenic pseudocyst. There are a couple of reports on the successful treatment of congenital splenic cysts with alcohol as a sclerosing agents [619].
Völk et al. [16] instilled alcohol in the splenic cyst weekly and repeated this procedure five times to achieve complete resolution because of a considerable amount of secretion from the cyst. Añon et al. [6] also treated a congenital splenic cyst successfully after two treatments involving the instillation of alcohol in the cyst. In our case, only one session of sclerosis with ethanol succeeded in obliterating the cyst without complications.
On the basis of our experience, percutaneous alcohol sclerotherapy with catheter drainage seems to be an effective and safe method for the treatment of post-traumatic splenic cysts in children.
Figures and Tables
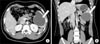
Fig. 1
Axial (A) and coronal (B) computed tomography scan show a low-density, non-enhancing cystic mass (6.8×9.5×7.0 cm) (arrows) located in the inferior pole of the spleen, which does not contain an enhancing solid portion.
References
1. Pachter HL, Hofstetter SR, Elkowitz A, Harris L, Liang HG. Traumatic cysts of the spleen--the role of cystectomy and splenic preservation: experience with seven consecutive patients. J Trauma. 1993; 35:430–436.

2. Labruzzo C, Haritopoulos KN, El Tayar AR, Hakim NS. Posttraumatic cyst of the spleen: a case report and review of the literature. Int Surg. 2002; 87:152–156.
3. Holland AJ, Ford WD, Bourne AJ. Conservative surgery for benign non-parasitic splenic cysts. Pediatr Surg Int. 1997; 12:353–355.

4. Dillemans B, Mottrie A, Decoster M, Gruwez JA. Epidermoid cysts of the spleen. Acta Chir Belg. 1993; 93:265–267.
5. Schier F, Waag KL, Ure B. Laparoscopic unroofing of splenic cysts results in a high rate of recurrences. J Pediatr Surg. 2007; 42:1860–1863.

6. Añon R, Guijarro J, Amoros C, Gil J, Bosca MM, Palmero J, et al. Congenital splenic cyst treated with percutaneous sclerosis using alcohol. Cardiovasc Intervent Radiol. 2006; 29:691–693.

8. Bean WJ, Rodan BA. Hepatic cysts: treatment with alcohol. AJR Am J Roentgenol. 1985; 144:237–241.

9. Akhan O, Ozmen MN, Dinçer A, Sayek I, Göçmen A. Liver hydatid disease: long-term results of percutaneous treatment. Radiology. 1996; 198:259–264.

10. De Caluwé D, Phelan E, Puri P. Pure alcohol injection of a congenital splenic cyst: a valid alternative? J Pediatr Surg. 2003; 38:629–632.

11. Wu HM, Kortbeek JB. Management of splenic pseudocysts following trauma: a retrospective case series. Am J Surg. 2006; 191:631–634.

12. Qureshi MA, Hafner CD. Clinical manifestations of splenic cysts: study of 75 cases. Am Surg. 1965; 31:605–608.
13. Klompmaker IJ, Haagsma EB, Slooff MJ. Splenic vein obstruction due to a solitary echinococcal splenic cyst, resulting in gastric fundus varices: an unusual cause of variceal bleeding. HPB Surg. 1993; 6:229–232.

14. Rakowski TA, Argy WP Jr, Pierce L Jr, Schreiner GE. Splenic cyst causing hypertension by renal compression. JAMA. 1977; 238:2528–2529.

15. Costa Borrás E, Segarra Llido V, Velázquez Terrón J, Menor Serrano F. Evolution of conservative treatment in traumatic spleen injuries. Report of 54 cases. Cir Pediatr. 2003; 16:14–16.
16. Völk M, Rogler G, Strotzer M, Lock G, Manke C, Feuerbach S. Post-traumatic pseudocyst of the spleen: sclerotherapy with ethanol. Cardiovasc Intervent Radiol. 1999; 22:246–248.

17. Akhan O, Cekirge S, Ozmen M, Besim A. Percutaneous transcatheter ethanol sclerotherapy of postoperative pelvic lymphoceles. Cardiovasc Intervent Radiol. 1992; 15:224–227.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download