1. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018; 390:2769–2778. PMID:
29050646.

2. van Deen WK, Choi JM, Zand A, et al. Sa1203 The development of e-Health tools for the management of inflammatory bowel diseases. Gastroenterology. 2014; 146(5 Suppl 1):S-229.

3. Rasmussen LM, Phanareth K, Nolte H, Backer V. Internet-based monitoring of asthma: a long-term, randomized clinical study of 300 asthmatic subjects. J Allergy Clin Immunol. 2005; 115:1137–1142. PMID:
15940125.

4. Cox D, Ritterband L, Magee J, Clarke W, Gonder-Frederick L. Blood glucose awareness training delivered over the internet. Diabetes Care. 2008; 31:1527–1528. PMID:
18477813.

5. Weinstock RS, Teresi JA, Goland R, et al. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabetes Care. 2011; 34:274–279. PMID:
21270184.

6. Boyne JJ, Vrijhoef HJ, Wit Rd, Gorgels AP. Telemonitoring in patients with heart failure, the TEHAF study: study protocol of an ongoing prospective randomised trial. Int J Nurs Stud. 2011; 48:94–99. PMID:
20615505.

7. Boyne JJ, Van Asselt AD, Gorgels AP, et al. Cost-effectiveness analysis of telemonitoring versus usual care in patients with heart failure: the TEHAF-study. J Telemed Telecare. 2013; 19:242–248. PMID:
24163233.

8. Omboni S, Ferrari R. The role of telemedicine in hypertension management: focus on blood pressure telemonitoring. Curr Hypertens Rep. 2015; 17:535. PMID:
25790799.

9. Kelly JJ, Sweigard KW, Shields K, Schneider D. Safety, effectiveness, and efficiency: a web-based virtual anticoagulation clinic. Jt Comm J Qual Saf. 2003; 29:646–651. PMID:
14679867.

10. Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017; 318:197–198. PMID:
28586821.

11. Wootton R, Geissbuhler A, Jethwani K, et al. Comparative performance of seven long-running telemedicine networks delivering humanitarian services. J Telemed Telecare. 2012; 18:305–311. PMID:
22869822.

12. Sutherland D, Hayter M. Structured review: evaluating the effectiveness of nurse case managers in improving health outcomes in three major chronic diseases. J Clin Nurs. 2009; 18:2978–2992. PMID:
19747197.

13. Kim AH, Roberts C, Feagan BG, et al. Developing a standard set of patient-centred outcomes for inflammatory bowel diseasean international, cross-disciplinary consensus. J Crohns Colitis. 2018; 12:408–418. PMID:
29216349.

14. Coons SJ, Gwaltney CJ, Hays RD, et al. Recommendations on evidence needed to support measurement equivalence between electronic and paper-based patient-reported outcome (PRO) measures: ISPOR ePRO Good Research Practices Task Force report. Value Health. 2009; 12:419–429. PMID:
19900250.

15. Taenzer P, Bultz BD, Carlson LE, et al. Impact of computerized quality of life screening on physician behaviour and patient satisfaction in lung cancer outpatients. Psychooncology. 2000; 9:203–213. PMID:
10871716.

16. Gutteling JJ, Busschbach JJ, de Man RA, Darlington AS. Logistic feasibility of health related quality of life measurement in clinical practice: results of a prospective study in a large population of chronic liver patients. Health Qual Life Outcomes. 2008; 6:97. PMID:
19000316.

17. Erharter A, Giesinger J, Kemmler G, et al. Implementation of computer-based quality-of-life monitoring in brain tumor outpatients in routine clinical practice. J Pain Symptom Manage. 2010; 39:219–229. PMID:
20152586.

18. Wright EP, Selby PJ, Crawford M, et al. Feasibility and compliance of automated measurement of quality of life in oncology practice. J Clin Oncol. 2003; 21:374–382. PMID:
12525532.

19. Con D, De Cruz P. Mobile phone apps for inflammatory bowel disease self-management: a systematic assessment of content and tools. JMIR Mhealth Uhealth. 2016; 4:e13. DOI:
10.2196/mhealth.4874. PMID:
26831935.

20. Kappelman MD, Palmer L, Boyle BM, Rubin DT. Quality of care in inflammatory bowel disease: a review and discussion. Inflamm Bowel Dis. 2010; 16:125–133. PMID:
19572335.

21. Reddy SI, Friedman S, Telford JJ, Strate L, Ookubo R, Banks PA. Are patients with inflammatory bowel disease receiving optimal care? Am J Gastroenterol. 2005; 100:1357–1361. PMID:
15929770.

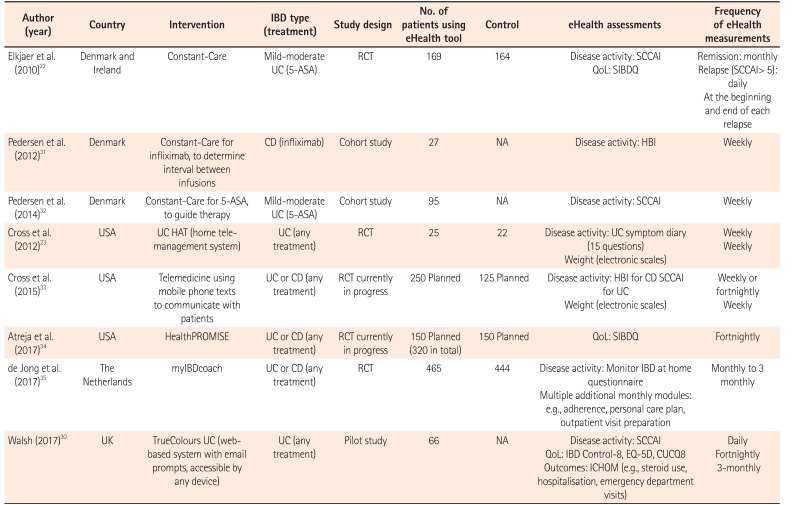
22. Elkjaer M, Burisch J, Avnstrøm S, Lynge E, Munkholm P. Development of a web-based concept for patients with ulcerative colitis and 5-aminosalicylic acid treatment. Eur J Gastroenterol Hepatol. 2010; 22:695–704. PMID:
19543101.

23. Cross RK, Cheevers N, Rustgi A, Langenberg P, Finkelstein J. Randomized, controlled trial of home telemanagement in patients with ulcerative colitis (UC HAT). Inflamm Bowel Dis. 2012; 18:1018–1025. PMID:
21688350.

24. Cross RK, Cheevers N, Finkelstein J. Home telemanagement for patients with ulcerative colitis (UC HAT). Dig Dis Sci. 2009; 54:2463–2472. PMID:
19104937.

25. Atreja A, Khan S, Rogers JD, et al. Impact of the mobile HealthPROMISE platform on the quality of care and quality of life in patients with inflammatory bowel disease: study protocol of a pragmatic randomized controlled trial. JMIR Res Protoc. 2015; 4:e23. PMID:
25693610.

26. de Jong M, van der Meulen-de Jong A, Romberg-Camps M, et al. Development and feasibility study of a telemedicine tool for all patients with IBD: myIBDcoach. Inflamm Bowel Dis. 2017; 23:485–493. PMID:
28267047.

27. Van Deen WK, van der Meulen-de Jong AE, Parekh NK, et al. Development and validation of an inflammatory bowel diseases monitoring index for use with mobile health technologies. Clin Gastroenterol Hepatol. 2016; 14:1742–1750.e7. PMID:
26598228.
28. Hou J, Weatherly J, Sellin J, et al. P-132 Feasibility of screening for anemia using the Crohn's and colitis foundation anemia care pathway in IBD Qorus. Inflamm Bowel Dis. 2017; 23:S46–S47.
29. Hou J, Xu A, Weatherly J, et al. P-129 CCFA quality of care breakthrough series collaborative: improving the delivery of urgent care for patients with IBD. Inflamm Bowel Dis. 2017; 23:S45–S46.
30. Walsh A. TrueColours: real time data collection in patients with ulcerative colitis [Doctoral dissertation]. Oxford, UK: University of Oxford;2017.
31. Pedersen N, Elkjaer M, Duricova D, et al. eHealth: individualisation of infliximab treatment and disease course via a self-managed web-based solution in Crohn’s disease. Aliment Pharmacol Ther. 2012; 36:840–849. PMID:
22971016.

32. Pedersen N, Thielsen P, Martinsen L, et al. eHealth: individualization of mesalazine treatment through a self-managed web-based solution in mild-to-moderate ulcerative colitis. Inflamm Bowel Dis. 2014; 20:2276–2285. PMID:
25248002.
33. Cross RK, Jambaulikar G, Langenberg P, et al. TELEmedicine for patients with inflammatory bowel disease (TELE-IBD): design and implementation of randomized clinical trial. Contemp Clin Trials. 2015; 42:132–144. PMID:
25812483.

34. Atreja A, Khan S, Otobo E, et al. P554 Impact of real world home based remote monitoring on quality of care and quality of life in inflammatory bowel disease patients: one year results of pragmatic randomized trial. J Crohns Colitis. 2017; 11:S362–S363.

35. de Jong M, Van Der Meulen A, Romberg-Camps M, et al. Telemedicine enables a safe shift from examination room based care to personalized care for inflammatory bowel disease: a pragmatic randomized multicenter trial with myIBDcoach. Gastroenterology. 2017; 152(5 Suppl 1):S186.

36. Elkjaer M, Shuhaibar M, Burisch J, et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-Care’ approach. Gut. 2010; 59:1652–1661. PMID:
21071584.

37. D'Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007; 132:763–786. PMID:
17258735.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download