Abstract
Objectives
Mandibular angle reduction or reduction genioplasty is a routine well-known facial contouring surgery that reduces the width of the lower face resulting in an oval shaped face. During the intraoral resection of the mandibular angle or chin using an oscillating saw, unexpected peripheral nerve damage including inferior alveolar nerve (IAN) damage could occur. This study analyzed cases of damaged IANs during facial contouring surgery, and asked what the basic standard of care in these medical litigation-involved cases should be.
Materials and Methods
We retrospectively reviewed a total of 28 patients with IAN damage after mandibular contouring from August 2008 to July 2015. Most of the patients did not have an antipathy to medical staff because they wanted their faces to be ovoid shaped. We summarized three representative cases according to each patient's perceptions and different operation procedures under the approvement by the Institutional Review Board of Seoul National University.
A prominent rectangular mandibular angle can originate from an enlarged masseter muscle, angular bone hypertrophy, or a combination of both. The bulging of the mandibular angle and a prominent chin has been considered to be unattractive, especially by the young Asian population.
Regardless of its muscular or bony origin, the surgical approach to bony reduction with supplemental myotomy has been considered the gold standard, and an intraoral approach using an oscillating saw for resection of a predetermined angular bone is a routine method in this standard of care. For the predetermination of excess bony resection, three-dimensional computed tomography (CT) with or without a rapid prototype model fabrication has been recommended more recently. And without CT, gross but easy measurements from a panoramic view could be also preceded in the private clinic for avoiding any hazardous contact to inferior alveolar nerve (IAN).
More recently, some patients wanted as much bone resection as possible regardless of IAN damage or its complete cutting, and they indicated their desired on the operation consult form without any hesitation. Some plastic or maxillofacial surgeons did confirm this preoperatively and even did as the patients' desired without considering the legal liability attending IAN damage. Thus, surgeons were faced with several medicolegal lawsuits, most of which were due to patients litigating over their less-than-perfect plastic surgery outcomes. These well-known claims were also due to the failure of appropriate communication between surgeon and patient.
From these points of view, is it possible that better outcomes from the patient's perspective could be balanced with the basic legal liability of surgeons? This article focused on better outcomes for patients with IAN damage, and outlining the basic standard of care for facial contouring surgery, including angle reduction and genioplasty procedures.
During August 2008 to July 2015, a total of 28 patients with damaged IANs after mandibular contouring surgery have visited to one professor (S.M.K.) in the Department of Oral and Maxillofacial Surgery at Seoul National Dental University Hospital (Seoul, Korea).
All patients had a history of mandibular angle reduction with or without masseter muscle excision or genioplasty with mandibular shaving within 6 months to 5 years, and finally visited for IAN damage management. Most of these suffered from consequent surgical sequelae, but they had provided preoperative permission in spite of the dangerous risk of IAN damage, and even agreed to IAN cutting to achieve a small round face. Among these patients, we summarized three representative cases according to each patient's perceptions and surgical procedures. This retrospective data analysis was approved by the Institutional Review Board of Seoul National University (S-D20170025).
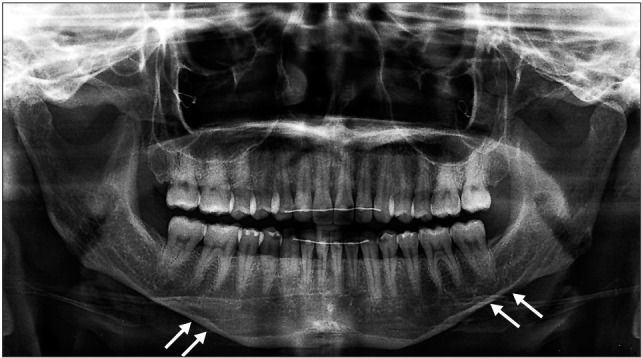
A 31-year-old Korean female visited complaining of an abnormal facial sensation due to previous mandibular angle contouring facial plastic surgery at a local plastic surgery clinic. On panoramic view, the inferior alveolar canals on each side of the mandible did not look normal after both mandibular angle reduction procedures. The canal was cut from the area below the left mandibular second molar with discontinuation in the left mandible. The right inferior alveolar canal was intimately contacted to the inferior border of the mandible without marked mental foramen.(Fig. 1)
We tested the degree of IAN injury using the nerve mapping method suggested by Lee et al.1, which consists of five checkpoints including the contact threshold, direction, two-point discrimination, pin prick, and thermal discrimination. The patient showed abnormal sensation in both the lower lip and chin areas as expected. She had mild to moderate paresthesia in both sides of the mandible, thus we predicted there was direct damage to the axon and epineurium, with a diagnosis of axonotmesis in the left mandible. Some damage to the epineurium in the right side resulted in a diagnosis of neuropraxia, which is a first degree injury according to Sunderland's classification2.
The patient received facial contouring surgery with bilateral zygoma reductions and both angle reductions with mandibular shaving five years previously. She did not have any antipathy to the clinic nor to the surgeon. She had desperately asked the hospital staff for a small round face, regardless of any disruptions to anatomical structures, including IAN damage. But as time went on, she could not endure the continuous pain in both lower cheek areas in spite of many prescriptions for neuro-depressive and analgesic drugs.
Although several consultations about her present symptoms predicted aggravated future outcomes and advised decompressive neurorrhaphy procedures to relieve her symptoms, the patient did not want any further operations not because of her fear for operation, but because of possible changes in the appearance of her face.
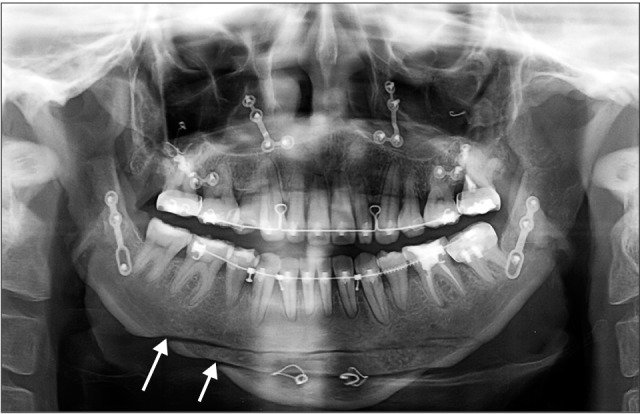
A 35-year-old Korean female complained of decreased lower lip and tongue sensation due to orthognathic surgery combining zygoma reduction and facial contouring at a local maxillofacial clinic. On panoramic view, the mental foramen and inferior alveolar canal on each side of mandible looks not normal after genioplasty procedure. The canal was cut from the below area of the right mandibular second molar with discontinuation in the right mandible, and the left inferior alveolar canal was also discontinued below the first molar and the second premolar area due to a horizontal bony cut.(Fig. 2)
The patient received whole facial contouring surgery with maxillary advancement, mandibular setback, zygoma reduction, genioplasty and combined facial shaving two years previously. She expressed her asking to the local maxillofacial surgeon only for a small face, regardless of nerve damage or any disruptions of essential anatomical structures. But she also noted that as time went on, she regretted her decision due to severely aggravated continuous pain in both lower cheeks. In spite of treatment with several neuro-depressive drugs and opioids, she suffered from severe depression with no continuation of her daily social and familial life.
The minimal corrective approach, including plate and wire removal with decompressive neurorrhaphy to relieve her pain was recommended during the 9 month follow-up period, but the patient did not agree to receive any further operations. Her major concern was retaining her small face, with which she was satisfied.
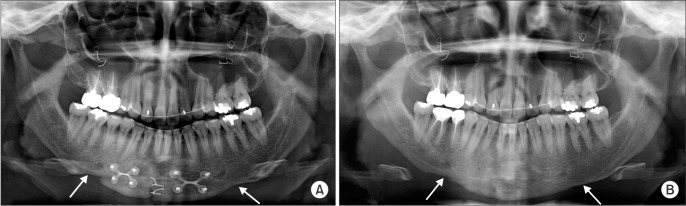
A 22-year-old Korean female complained of absolute numbness in her right lower face and an abnormal facial sensation in her left lip and cheek. She had received facial contouring surgery with both zygoma and angle reductions accompanied by total mandibular shaving two years previously at a local plastic clinic. After that, numbness and paresthesia sensation continued into her whole face with related paroxysmal pain in both lower cheeks that was aggravated recently. On panoramic view, the inferior alveolar canal on each side of her mandible looked abnormal, showing IAN cutting on the right and abrupt discontinuation on the left side.(Fig. 3. A)
We tested the degree of IAN injury using the nerve mapping method. She showed abnormal and even no sensation on both lower lips and chin areas, per our expectations. She had moderate to severe paresthesia in both sides of mandible, thus we predicted that there was direct damage to the axon and epineurium, resulting in a diagnosis of neurotmesis in the right IAN and axonotmesis in the left IAN.
Regardless of her antipathy to her first surgeon, we strongly recommended prompt IAN decompressions combed with previously adapted plate and wire removals. Due to her recent severely aggravated pains, she also wanted to receive an open procedure for the nerodecompressive IAN as soon as possible.
After all removals of foreign bodies and both IANs decompression with keeping continuations of inferior alveolar canal and neuroma excision (Fig. 3. B), the patient's pains were mitigated to less than half of her first visual analogue scale score. She was satisfied with her decompressive results three months later and her continuous pain could be managed with neuro-depressive drugs.
Recently, facial bone contouring surgery has become increasingly popular, especially in many East Asian countries. Many Asian young people usually consider a broad and rectangular face to be unattractive and unaesthetic, and find an oval and round face more desirable. Facial contouring surgery including reduction malarplasty or zygoma reduction, mandibular anguloplasty or mandibular angle reduction, and reduction genioplasty are representative surgical methods34.
Mandibular angle reduction or reduction anguloplasty of mandible is a well-known and popular contouring surgery that reduces the width of the lower face and results in an oval round shaped face. The main procedures for this reduction are intraoral resections of the outer cortex of the angular bone and mandibular body. This cortical cutting using an oscillating saw is known to be safe and effective. But according to the amounts of maximum resection and to the thickness of the lateral cortex of mandible in severely lateral flaring cases, this procedure is never considered to be easy, but rather a highly risky procedure that can include nerve damage.
Reduction genioplasty is also a representative facial contouring procedure in patients with a prominent chin or hypertrophic mentum. In a reduction genioplasty for vertical shortening of the chin, two routine horizontal osteotomies parallel to each other and to the occlusal plane used to be performed and the final fixation of the mobile chin is also performed. The mental foramen with mental nerve and its minor branches could be easily excised or injured during these procedures.
The essential points required to achieve satisfactory results after a facial contouring surgery are to meet each patient's aesthetic expectations and to reduce the possible risks of unexpected complications. Also, a standardized surgical technique is also important to produce simplified and predictable outcomes with a low incidence of complications. However, no surgical technique for facial contouring has been established as a standard. On the contrary, surgical methods used in facial contouring must have some degree of versatility and variability to meet each patient's expectations and to obtain superior cosmetic outcomes. Due to these reasons, although aesthetic surgical techniques mainly depend on the surgeon's subjective evaluation, some amount of error may occur, but steps to avoid unintentional injury should be instituted during the surgical procedure4.
Maxillofacial and plastic surgeons must always be aware of the possibilities of being sued or litigated. The main issues of patients and surgeons involved in lawsuits could be classified according to the individual surgical procedure, pre- and postoperative communications, and each individual Nation's relevant laws. As patients have become increasingly aware regarding medical care, an increase in the unexpected side effects of procedures has been observed, thereby leading to an increase in disputes regarding medical malpractice5. Form a total of 54 judgments made in South Korean courts between 2000 and 2013 that were related to the field of plastic surgery, violation of the duty of explanation (29%), the duty of care (17%), both duties (35%), and no violation of duty (10%) were seen. The Supreme Court requires plastic surgeons to determine the type, timing, methods, and scope of their treatments when considering possible results5. As more lawsuits have been filed by patients against surgeons, they have led to social and financial losses for the physicians involved. Vila-Nova da Silva et al.6 reported the determining factors that influenced judicial decisions against plastic surgeons from analysis of 98 malpractice claims obtained from a state court of justice in Brazil. The most common complaints were scars and resulting contour (48.9%), general dissatisfaction (25.6%), and complications (25.2%). Judicial decisions were mainly influenced by the quality of medical records, informed consent, and expert report conclusions6.
An analysis of unsolicited patient complaints from 31,077 physicians, 3,935 surgeons, 338 plastic and reconstructive surgeons, and 519 dermatologists showed that the overall mix of patient complaints from plastic and reconstructive surgeons was nearly the same as for the national cohort of all physicians, including care and treatment (49%), communication (19%), accessibility and availability (14%), money or payment issues (9%), and concern for patient/family (9%)7. In another retrospective analysis of verdict and settlement reports for the contributing factors to medical negligence relevant to craniofacial surgery, the most common alleged factors included intraoperative negligence (69.0%), permanent deficits (54.8%), requiring additional surgery (52.4%), missed diagnosis of a complication (42.9%), disfigurement or scarring (28.6%), postoperative negligence (28.6%), and inadequate informed consent (20.6% of surgical cases). Failure to diagnose a fracture (19.0%) and cleft-reparative procedures (14.3%) were the most frequently litigated entities8. In another retrospective analysis of malpractice litigations, characterization of complications leading to litigation was of special interest to practitioners of facial plastic surgery procedures because of the higher proportion of elective cases relative to other subspecialties. The most litigated procedures were blepharoplasties and rhinoplasties. Alleged lack of informed consent was noted in 38.6% of cases; excessive scarring/disfigurement, functional considerations, and postoperative pain were also reasons for litigation9. Informed consent was the most reported entity in these malpractice suits. This finding emphasizes the importance of open communication between physicians and their patients regarding expectations as well as documentation of specific risks, benefits, and alternatives.
Plastic surgery is a field that demands perfection, yet despite our best efforts errors occur every day. Most errors are minor, but occasionally patients are harmed by our mistakes. Although there is a strong ethical requirement for full disclosure of medical errors, data suggest that surgeons have a difficult time disclosing errors and apologizing, “Conventional wisdom” has been used to avoid frank discussion of errors with patients. This concept is fueled by the fear of litigation and the notion that any expression of apology leads to malpractice suits10.
Based on the previously reports of body contouring litigation, younger plaintiff age and iatrogenic injury strongly favored plaintiffs in either awarded damages or awarding of a settlement. Disfigurement favored plaintiffs only in awarded damages. Paik et al.11 emphasized the need for adequate, expeditious communication with the patient, including explaining realistic aesthetic results, risks of the procedure, and iatrogenic organ injury. Incorporating these recommendations into clinical practice may promote an improved physician-patient relationship while reducing litigations' health care costs. A retrospective analysis of the reasons plastic surgery patients made complaints and claims of negligence, the most common reasons were poor communication and treatment delays. There were 3 successful cases which all mentioned adverse scarring, suggesting that this risk was either not discussed or the informed consent process was inadequately documented. Poor communication is highlighted as the main reason for patients making formal complaints. Inadequate documentation of informed consent discussions may also contribute to successful negligence claims12.
Many surgeons could find themselves faced with a claim of malpractice, most of which may be due to a less-than-perfect outcome from the patient's perspective. Attention to legal principles such as standard of care, warranty and disclosure, knowledge of patient factors, and the ability to communicate clearly and effectively will hopefully maximize the possibility of remaining a claims-free surgeon131415. But, if the patient asks for an operation beyond the standard of practice, beyond the common medicolegal boundary, how can we manage the patient? Could we just prepare litigation for facial plastic surgery procedures and characterize factors important in determining legal responsibility, as this information may be of great interest and use to practitioners in several specialties?
Patient expectations and demands about the outcomes of surgery have significantly increased over the last decade. Several medicolegal databases regarding medical malpractice in the field of facial plastic surgery show a physician's favor, an out-of-court settlement, and a jury awarding damages for malpractice have been vindicated usually. If we also consider the patient desires beyond the standard of care that can include procedures such as IAN cutting, the verdict for us will be in the realm of criminal law, excluding of medicolegal law.
Any medical management of irreversible harm-causing care to the patient can be never apologized for nor forgiven in the moral medical mind. Although there are too many commercial medical market and patients' desperate desires to be beautiful face, surgeon's ethical mission should be remained stronger and stronger. In addition, the patient's basic rights and responsibilities that enable them to receive the only formal and right surgical treatment also should be taught to the patient. This is another essential responsibility of surgeons.
Maxillofacial surgeons need sincere and sound strategies for dealing with patients presenting with previous facial esthetic surgery that may constitute malpractice. For the solving any complaints brought by wrong informed consent surgical outcomes in unhappy patient, only ethnical and academical advices should be given, not as an attorney but as a medical specialist in a related field. This ethical analysis of adverse outcomes and presentation of measures to improve outcomes is fundamental to a patient's recovery and well-being.
Notes
References
1. Lee JH, Lee SY, Song SI, Lee EJ, Ahn KM, Kim SM, et al. Sensory normative values of lower lip and tongue for evaluation of inferior alveolar or lingual nerve damage. J Korean Assoc Maxillofac Plast Reconstr Surg. 2003; 25:114–122.
2. Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain. 1951; 74:491–516. PMID: 14895767.

3. Morris DE, Moaveni Z, Lo LJ. Aesthetic facial skeletal contouring in the Asian patient. Clin Plast Surg. 2007; 34:547–556. PMID: 17692710.

4. Lee TS. Standardization of surgical techniques used in facial bone contouring. J Plast Reconstr Aesthet Surg. 2015; 68:1694–1700. PMID: 26346781.

5. Park BY, Kim MJ, Kang SR, Hong SE. A legal analysis of the precedents of medical disputes in the cosmetic surgery field. Arch Plast Surg. 2016; 43:278–283. PMID: 27218027.

6. Vila-Nova da Silva DB, Nahas FX, Ferreira LM. Factors influencing judicial decisions on medical disputes in plastic surgery. Aesthet Surg J. 2015; 35:477–483. PMID: 25908704.

7. Hultman CS, Gwyther R, Saou MA, Pichert JW, Catron TF, Cooper WO, et al. Stuck in a moment: an ex ante analysis of patient complaints in plastic surgery, used to predict malpractice risk profiles, from a large cohort of physicians in the patient advocacy reporting system. Ann Plast Surg. 2015; 74(Suppl 4):S241–S246. PMID: 25785388.
8. Svider PF, Eloy JA, Folbe AJ, Carron MA, Zuliani GF, Shkoukani MA. Craniofacial surgery and adverse outcomes: an inquiry into medical negligence. Ann Otol Rhinol Laryngol. 2015; 124:515–522. PMID: 25595141.
9. Svider PF, Keeley BR, Zumba O, Mauro AC, Setzen M, Eloy JA. From the operating room to the courtroom: a comprehensive characterization of litigation related to facial plastic surgery procedures. Laryngoscope. 2013; 123:1849–1853. PMID: 23299988.
10. Vercler CJ, Buchman SR, Chung KC. Discussing harm-causing errors with patients: an ethics primer for plastic surgeons. Ann Plast Surg. 2015; 74:140–144. PMID: 24830658.
11. Paik AM, Mady LJ, Sood A, Lee ES. Beyond the operating room: a look at legal liability in body contouring procedures. Aesthet Surg J. 2014; 34:106–113. PMID: 24259355.
12. Patel AJ, Morrison CM. Opportunities to reduce plastic surgery claims through an analysis of complaints data. J Plast Reconstr Aesthet Surg. 2013; 66:455–459. PMID: 23312235.

13. Dyer C. Clinical negligence claims against plastic surgeons rise “significantly”. BMJ. 2012; 344:e298. PMID: 22234910.

14. Mehta S, Farhadi J, Atrey A. A review of litigation in plastic surgery in England. Lessons learned. J Plast Reconstr Aesthet Surg. 2010; 63:1747–1748. PMID: 20356812.

15. Gorney M. Claims prevention for the aesthetic surgeon: preparing for the less-than-perfect outcome. Facial Plast Surg. 2002; 18:135–142. PMID: 12063661.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download