Abstract
In cases of severe alveolar bone atrophy in the posterior maxillary area, which has only a thin sinus floor, the autogenous tooth bone graft block (ABTB) was used to wrap the implant to enhance its primary stability and osseointegration in the sinus. These cases with four years of clinical follow-up demonstrate the applicability of the ABTB in maxillary sinus membrane elevation to improve the outcomes of implant placement.
There have been considerable efforts in basic and clinical research to find the best bone graft material for implant osseointegration in the sinus. The autogenous tooth bone graft (AutoBT; Korea Tooth Bank, Seoul, Korea) was firstly developed in 2008. There have been several clinical studies evaluating the use of AutoBT in the sinus, with all results showing more favorable outcomes in bone regeneration as compared to other conventional graft materials12. The autogenous tooth bone graft block (ABTB), which is made from root dentin, has been shown to be both clinically safe and efficacious in several studies. In particular, the ABTB has been reported to be an appropriate material for socket preservation, guided bone regeneration (GBR), and ridge augmentation. ABTB already has shown good osteoinductive, osteoconductive, and remodeling ability due to its type I collagenous nature as well as its three-dimensional scaffold34. This collagenous nature could act as an excellent vascular scaffold in the sinus cavity, which has a poor blood supply. The major role of the ABTB in this report was to wrap around the implant to enhance its primary stability and osseointegration into the sinus. This is called the "ring technique".
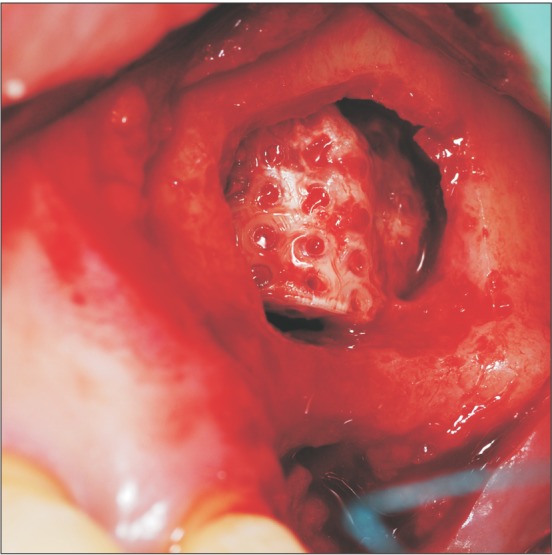
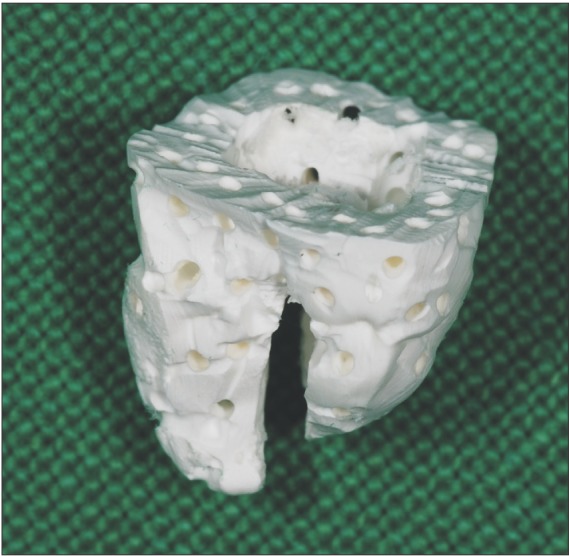
This technique can be used in cases during which the residual alveolar bone height to the maxillary sinus floor is insufficient for implant stability. In our case, a 51-year-old man presented with his left maxillary first molar missing for several months. We decided to perform sinus bone graft and simultaneous implant placement.(Fig. 1) ABTB was prepared from his son's wisdom tooth because the patient did not have teeth to be extracted for manufacturing. This process met the standards of the technical manual of the Korea Tooth Bank, as has been previously reported56. The extracted wisdom tooth was immersed in 75% alcohol and then the soft tissues and calculus were removed. Crowns were severed at the cement enamel junctions and ABTBs were made from the root portion of the tooth. Additional holes sized 0.2 mm were made at the surface of the canal area to create macropores for promoting vascular invasion and bone formation.(Fig. 2)
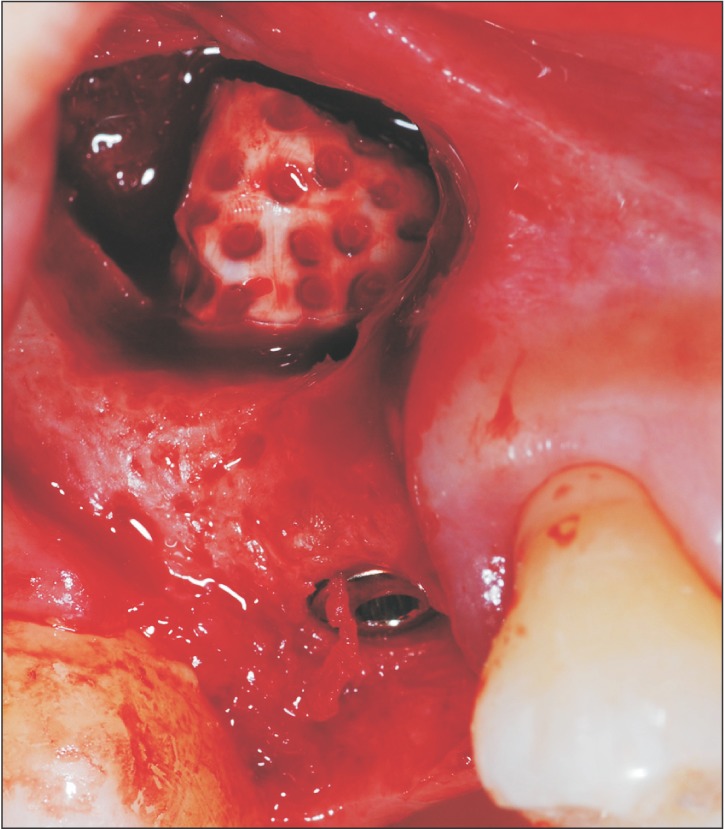
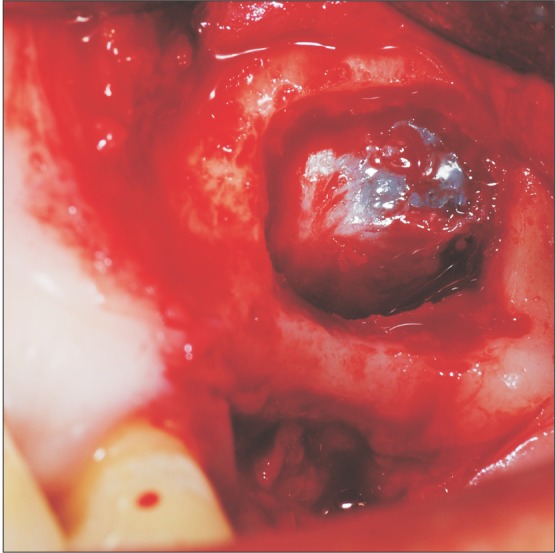
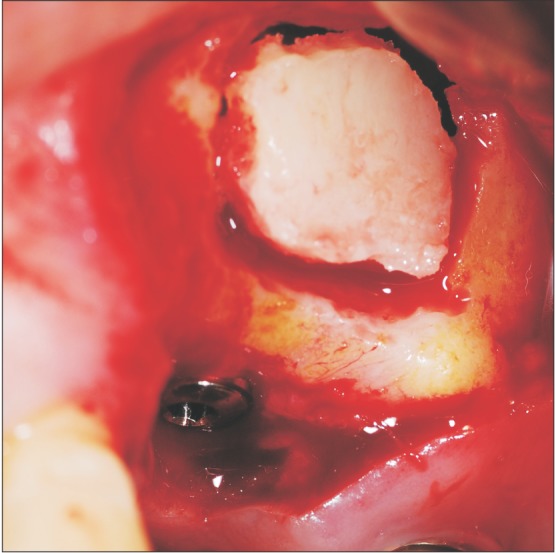
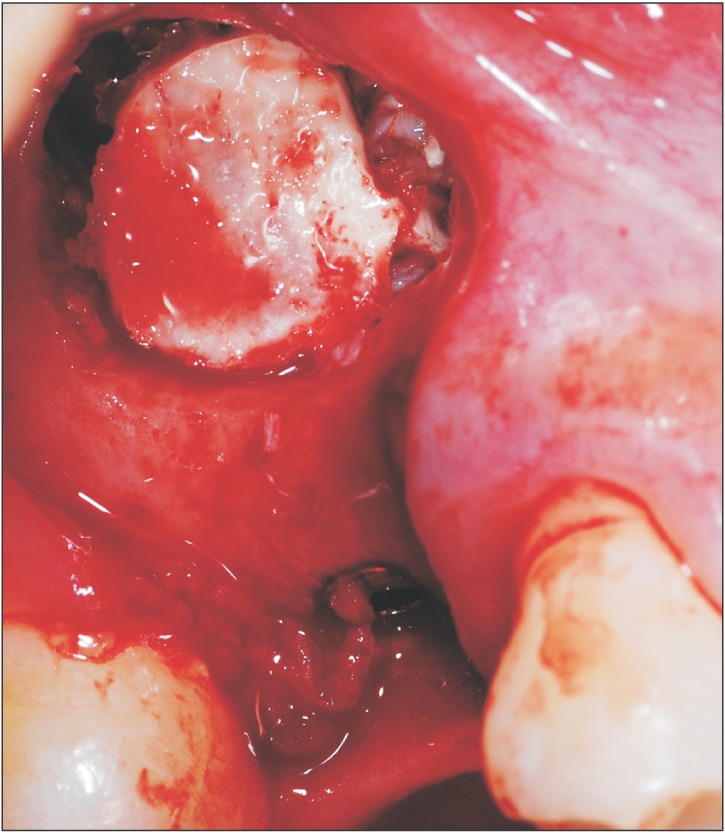
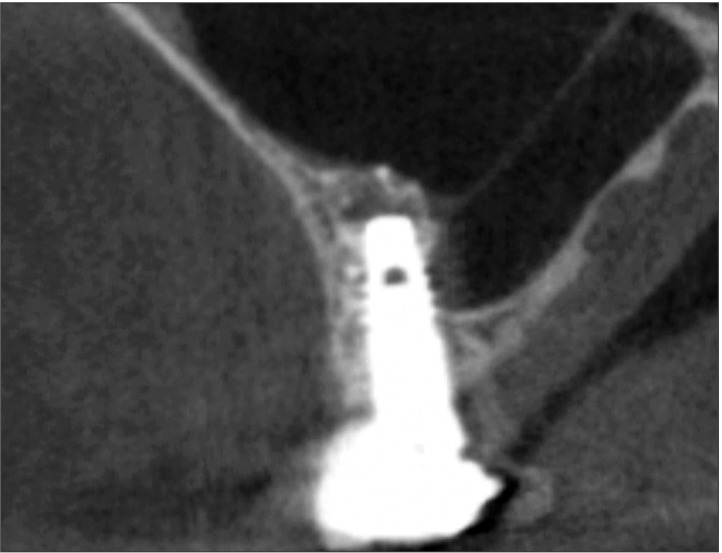
Through the routine lateral window approach, we lifted the sinus membrane to identify the thin sinus floor, locate the implant hole, and spare the space for the ABTB.(Fig. 3) Before placing the ABTB into the sinus, the implant was adapted to extraorally fit into the ABTB through the pulp chamber as tightly as possible. With this procedure, we could secure additional stability of the thin alveolar bone.(Fig. 4) After inserting the ABTB upside down into the sinus, the implant was placed through the thin sinus floor and into the apex of the ABTB while being grabbed by a small Kelly or mosquito clamp to provide stability without additional fixation. We could see blood pooling of the ABTB, which met the wettability requirements of bone graft substitutes.(Fig. 5, 6) The lateral wall was then replaced in situ.(Fig. 7) When compared to the X-rays obtained immediately after the operation, the X-rays after four years showed well-formed bone surrounding the implant. The border between the implant and ABTB almost disappeared, which means the ABTB was successfully incorporated. Moreover, it was difficult to identify any marginal bone loss even with the final prosthesis.(Fig. 8, 9)
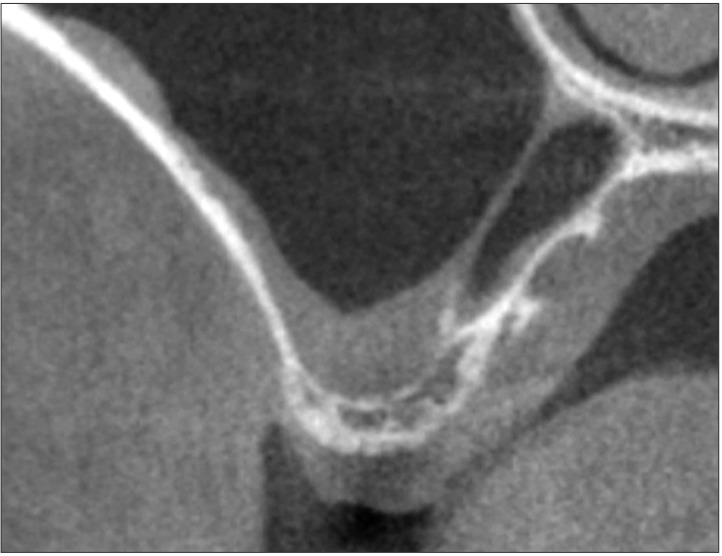
In another case, a 27-year-old man presented with a missing #16 tooth for several years without any restoration, so that only a thin sinus floor remained due to severe pneumatization. The #16 area became an anatomic defect of the alveolar bone with about 1 to 2 mm of residual bone height.(Fig. 10) In order to install the implant in a single stage, sinus augmentation was inevitable and an ABTB was chosen to obtain initial stability of the implant on the thin alveolar bone. An ABTB was prepared using his lower right impacted mandibular third molar.(Fig. 11) A pulp chamber that is too small to accommodate an implant can be enlarged with an instrument to fit the implant.(Fig. 12) The sinus membrane was elevated and simultaneous implant placement was performed using the ABTB graft similar to the case above.(Fig. 13, 14, 15) Four years later, we could see that the implant osseointegrated with the final prosthesis. The whole bone housing was intact and there was no marginal bone resorption around the implant neck area when compared to the films immediately after the operation.(Fig. 16, 17)
Since Murata7 reported that autogenous demineralized dentin matrix could be used for sinus augmentation, there have been several reports of the use of AutoBT in the sinuses. Lee et al.8 compared the use of AutoBT powder with synthetic hydroxyapatite (HA) in the sinus of miniature pigs. Histomorphometrical analysis showed that more new bone was formed in the AutoBT group than the synthetic HA group. In a clinical trial, Kim et al.9 reported that the AutoBT particles united well with the new bone in the sinus, with bone formation starting from the alveolus and gradually rising toward the sinus. When comparing the use of AutoBT with synthetic HA in the sinus in both prospective and retrospective human clinical trials, the authors reported that AutoBT could be an alternative to synthetic bone grafts in sinus lifts based on the observation that the average bone resorption with AutoBT powder was similar to that of osteon composites 1 year after surgery with no serious complications or implant failures12. Kim et al.4 reported the clinical results of 12 cases involving ABTB, which included GBR, ridge augmentation, extraction socket graft, and sinus bone graft. Among these cases, only 3 were in the sinus, though they showed that ABTB could be useful in various surgical procedures in the sinus. However, the ABTB in this report was used only when mixed with other powder forms of bone graft materials, and acted as a membrane.
In this technical report, the ABTB acted as a scaffold for the implant, which penetrates the thin sinus floor to the apex of the ABTB. This method is known as the "ring technique," which was developed based on reports from animal studies and human clinical trials1011. In 2014, the author was the first to report the technique and short-term clinical results of ABTB with simultaneous sinus implant. An additional four years of follow-up of these cases indicated that ABTB works very well in the sinus to secure primary stability, bone formation, and marginal bone resorption12. In addition, the disappearance of the border between the sinus floor and the alveolus indicated that the ABTB has the capability of incorporation and continuous remodeling with low-crystalline inorganics and type I collagen1314.
References
1. Kim YK, Lee J, Yun JY, Yun PY, Um IW. Comparison of autogenous tooth bone graft and synthetic bone graft materials used for bone resorption around implants after crestal approach sinus lifting: a retrospective study. J Periodontal Implant Sci. 2014; 44:216–221. PMID: 25368809.

2. Jun SH, Ahn JS, Lee JI, Ahn KJ, Yun PY, Kim YK. A prospective study on the effectiveness of newly developed autogenous tooth bone graft material for sinus bone graft procedure. J Adv Prosthodont. 2014; 6:528–538. PMID: 25551014.

3. Park SM, Hwang JK, Kim YK, Um IW, Lee GH, Kim KW. Microscopic feature, protein marker expression, and osteoinductivity of human demineralized dentin matrix. J Korean Dent Sci. 2012; 5:77–87.

4. Kim YK, Kim SG, Um IW, Kim KW. Bone grafts using autogenous tooth blocks: a case series. Implant Dent. 2013; 22:584–589. PMID: 24225779.
5. Kim YK, Um IW, Murata M. Tooth bank system for bone regeneration: safety report. J Hard Tissue Biol. 2014; 23:371–376.
6. Lee JY, Kim YK, Um IW, Choi JH. Familial tooth bone graft: case reports. J Korean Dent Assoc. 2013; 51:459–467.
7. Murata M. Autogenous demineralized dentin matrix for maxillary sinus augmentation in humans: the first clinical report. Gothenburg: 81th International Association for Dental Research;2003.
8. Lee DH, Yang KY, Lee JK. Porcine study on the efficacy of autogenous tooth bone in the maxillary sinus. J Korean Assoc Oral Maxillofac Surg. 2013; 39:120–126. PMID: 24471029.

9. Kim YK, Jun SH, Um IW, Kim SY. Evaluation of the healing process of autogenous tooth bone graft material nine months after sinus bone graft: micromorphometric and histological evaluation. J Korean Assoc Maxillofac Plast Reconstr Surg. 2013; 35:310–315.

10. Kim SK, Kim SW, Kim KW. Effect on bone formation of the autogenous tooth graft in the treatment of peri-implant vertical bone defects in the minipigs. Maxillofac Plast Reconstr Surg. 2015; 37:2. PMID: 25750910.

11. Pikos MA. Mandibular block autografts for alveolar ridge augmentation. Atlas Oral Maxillofac Surg Clin North Am. 2005; 13:91–107. PMID: 16139756.

12. Um IW, Lee JK. Familial tooth bone graft. In : Murata M, Um IW, editors. Advances in oral tissue engineering. Chicago: Quintessence Publishing;2014. p. 67–72.
13. Kim YK, Kim SG, Oh JS, Jin SC, Son JS, Kim SY, et al. Analysis of the inorganic component of autogenous tooth bone graft material. J Nanosci Nanotechnol. 2011; 11:7442–7445. PMID: 22103215.

Fig. 1
The cone-beam computed tomography of the sinus before the operation. The residual bone height was about 1 to 2 mm on #26.
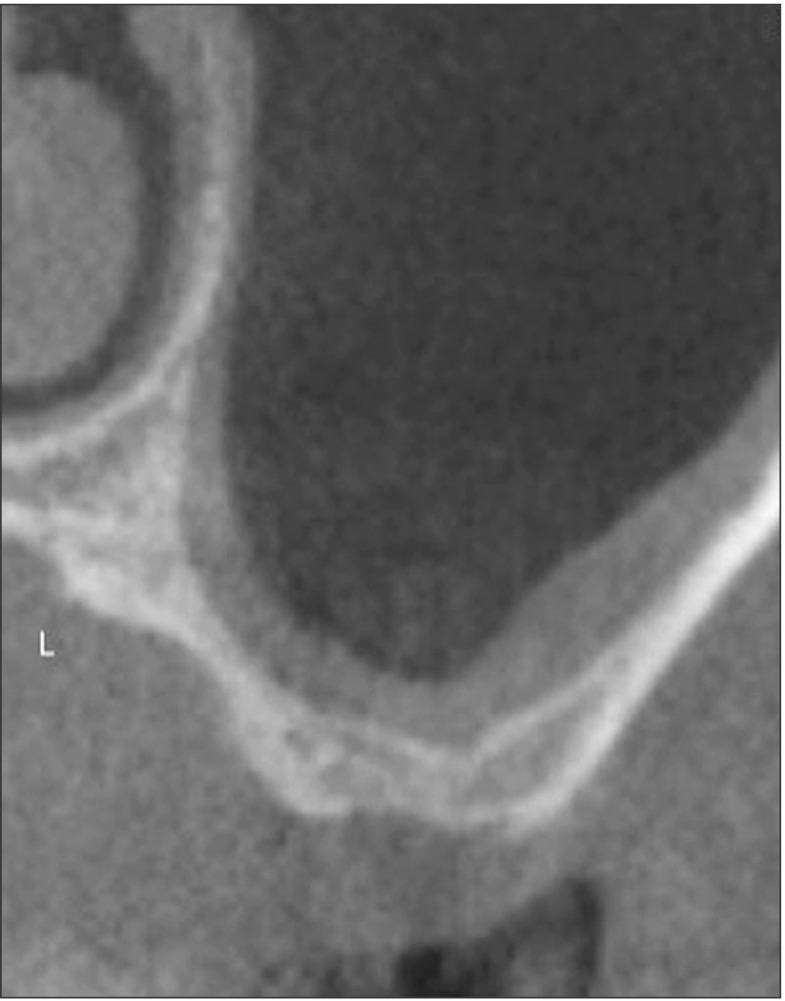
Fig. 2
The occlusal view of the autogenous tooth bone graft block, which was made from the root portion of the extracted tooth.
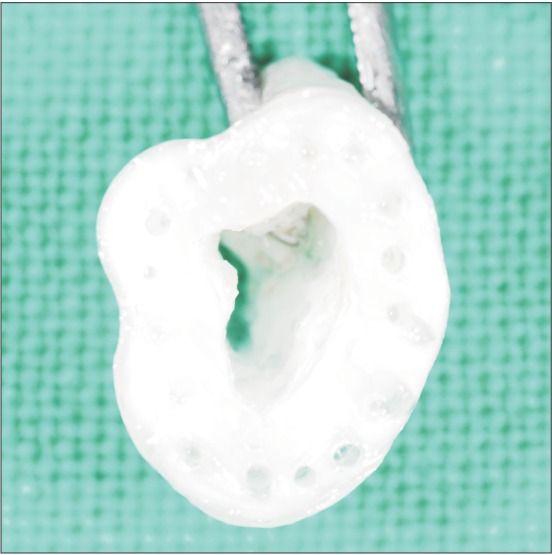
Fig. 6
The implant was simultaneously installed through the alveolar bone and into the autogenous tooth bone graft block.
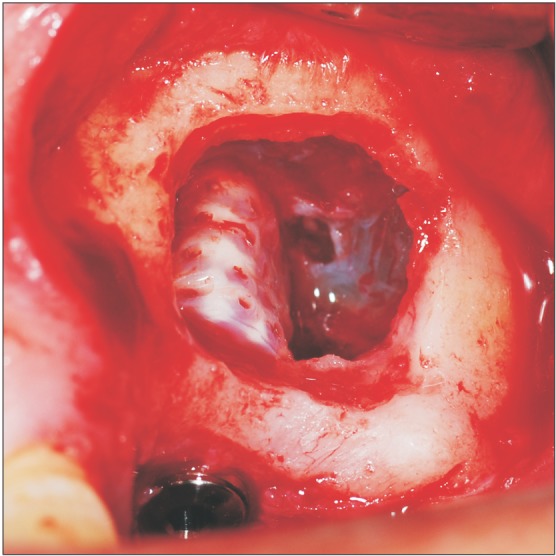
Fig. 8
The cone-beam computed tomography immediately after the simultaneous installation of the implant and the autogenous tooth bone graft block.
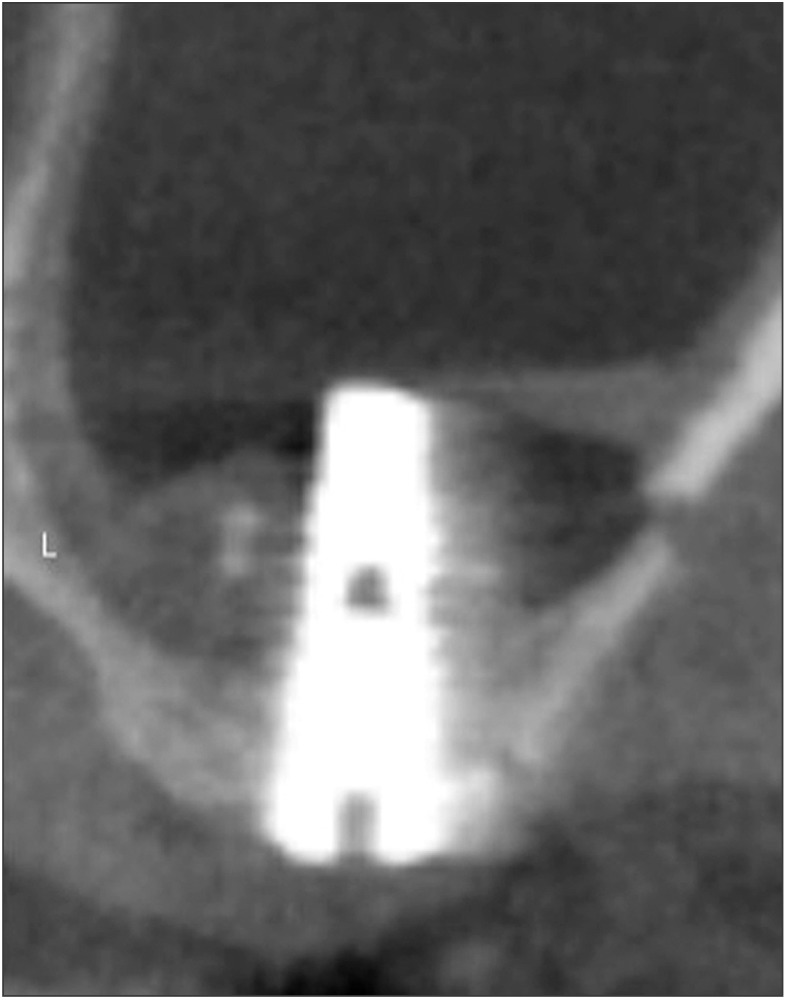
Fig. 13
The lateral sinus window opening and the preparation of the implant site on the alveolar bone.
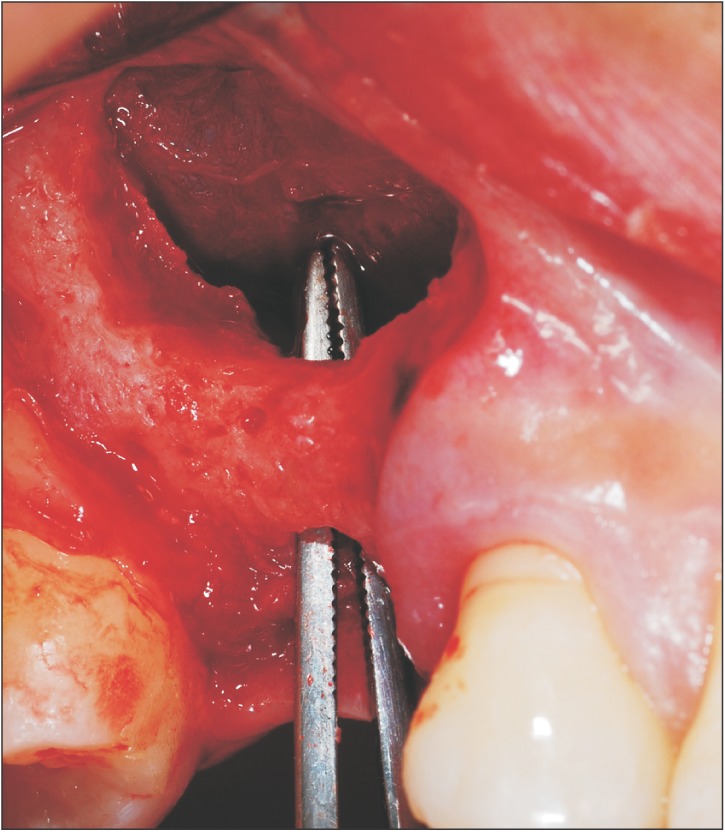
Fig. 14
The insertion of the autogenous tooth bone graft block (ABTB) into the sinus and the installation of the implant through the thin alveolar bone to the ABTB.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download