Abstract
Accidental displacement of the third molar tooth or its fragment into the anatomical spaces is a rare but potentially serious complication. The most common sites of mandibular third molar displacement are the sublingual, submandibular, and pterygomandibular spaces. Removal of a displaced tooth or its fragments from these spaces may be difficult due to poor access and the vital structures involved in these spaces; therefore, removal may result in permanent damage. This article is intended to provide a concise update of the reported cases of submandibular displacement and to present a case of intraoral management of mandibular third molar root fragments that were displaced into the submandibular space.
Removal of the third molar remains one of the most common oral and maxillofacial surgical procedure and is associated with low morbidity12345. However, like all surgeries, surgical removal of the third molar may be associated with several complications. These complications are more common in the mandible than in the maxilla, with reported incidences ranging from 2.6% to 30.9%1367891011. Accidental displacement of the third molar tooth or root fragment into into different anatomical spaces is a very rare complication of third molar surgery and may be accompanied by severe tissue damage, psychological distress, and medico-legal conditions121314. While iatrogenic displacement is a well-known phenomenon, little information related to this complication is available in the literature17. A few cases have previously reported displacement into different facial spaces, including the maxillary sinus15, infratemporal510, pterygomandibular614, lateral pharyngeal1617, lateral cervical18, pterygopalatine19, buccal20, sublingual921, and submandibular123 spaces. The maxillary sinus and submandibular spaces are the two most commonly affected. Since so few cases have been published, no consensus has yet been reached in terms of the optimum management protocol that can be applied in all circumstances2223.
Here, we present a case of displacement into the submandibular space and review related published cases. To this end, the PubMed-MEDLINE and Google Scholar databases were searched for papers about iatrogenic displacement of the mandibular third molar tooth or tooth fragment into the submandibular space. The date range extended through 2017. The search was performed using the keywords ‘displacement’, ‘submandibular space’, ‘mandibular third molar’, ‘accidental’, ‘complication’, and combinations thereof.
A 48-year-old female patient was referred to Oral and Maxillofacial Surgery Clinic with complaints of headache, paresthesia on the right lateral region of the tongue, and taste impairment. She had undergone a mandibular third molar extraction performed by a general practitioner 3 months earlier. Panoramic radiography showed the presence of a radiopaque mass similar to that of a tooth root.(Fig. 1) Cone-beam computed tomography (CBCT) scans were obtained for detailed radiographic examination and revealed high density areas in the submandibular region.(Fig. 2) A surgical operation was planned under general anesthesia. Potential complications were explained to the patient and written consent was obtained.
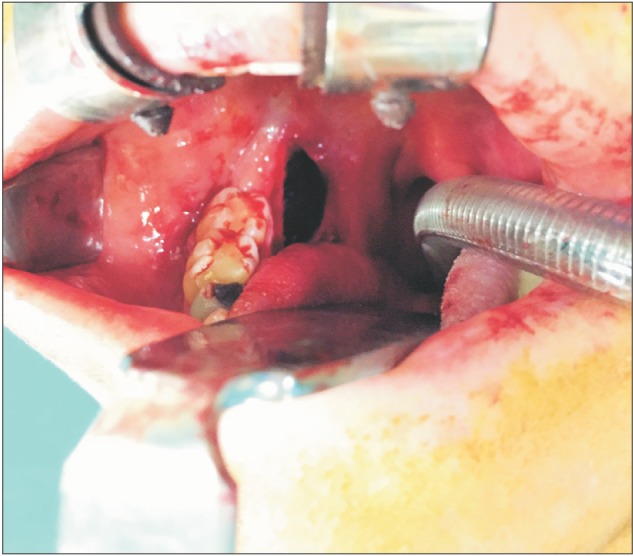
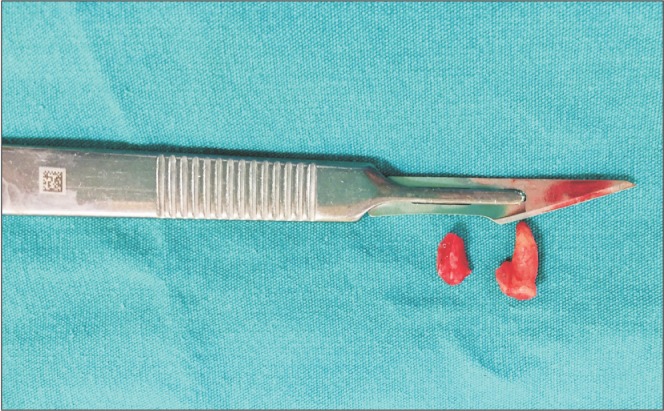
Under general anesthesia, a conventional lingual flap starting from the disto-lingual angle of the first molar was extended to the anterior surface of ramus. The flap was reflected up to the submandibular region with great care and support from an extra-orally placed finger.(Fig. 3). The dislodged root fragments were found by blunt dissection, grasped with a pair of forceps, and removed.(Fig. 4) The patient was given oral antibiotics and analgesics. One week after surgery, the healing of soft tissue was uneventful. However, the patient's complaints of numbness, intense pain, burning tongue, and taste impairment were still present and altered her daily life significantly after the operation.
Accidental displacement of the mandibular third molar tooth or fragments into the submandibular space is very rare, with a reported incidence of less than 1%2. The first case of iatrogenic submandibular displacement was reported by Ho24 in 1980; to date, only 12 reports have been published13472224252627282930.(Table 1) In most of the cases, the major predisposing factors contributing to displacement were a thin lingual plate and uncontrolled maneuvering due to a lack of basic surgical knowledge. However, number of patient and operator related factors have also been reported to potentially contribute to displacement1342225.
The submandibular space is a complex triangular compartment that is bounded superiorly by the mylohyoid muscle, anteriorly by the medial surface of the mandible and the skin, and inferiorly by the superficial fascia and platysma muscle. It encloses vital anatomic structures such as the submandibular salivary gland, facial artery/vein, lingual nerve, and hypoglossal nerve31. The submandibular space also freely communicates superiorly with the sublingual space and inferiorly with the lateral pharyngeal space26. Therefore, accidental displacement of a mandibular third molar root or fragments into this space poses a risk of iatrogenic injury to vital structures. Moreover, the root or fragments could potentially be displaced further into deeper facial spaces. Such deeper displacements usually require additional invasive approaches.
A displaced tooth may remain asymptomatic or cause pain, swelling, paresthesia, and trismus. The effects of a displaced tooth depend on its size, location, and whether or not there is an infection1. Solanki et al.25 reported a case of mandibular third molar displacement into the submandibular space that remained asymptomatic for two years. In a case reported by Anand and Patil4, dysaesthesia occurred immediately in the lip after an unsuccessful surgery performed by a general practitioner. Aznar-Arasa et al.21 reported 6 cases of sublingual displacement; five of the six patients remained asymptomatic. According to Aznar-Arasa et al.21, the symptoms are closely related to the size of the displaced fragment and displacement tends to trigger symptoms when the size of the fragment exceeds 5 mm. In the present case, both medial and distal root fragments of the third molar tooth exceeding 5 mm were displaced into the submandibular fossa and caused paresthesia on the right lateral region of the tongue after the first surgery. Due to the severe psychological distress of the patient, the case management was dramatically complicated.
Once the complication occurs, it is important to rigorously evaluate the severity of the condition. Any attempt to retrieve the displaced tooth or fragment without adequate visibility and surgical/anatomical knowledge may result in further displacement into deeper facial spaces, iatrogenic injury to the vital structures, and life-threatening events such as deep neck infection, mediastinites, and airway compromise2627. Based on the reported cases, it can be concluded that the majority of iatrogenic displacements were caused by practitioners with a lack of surgical expertise. Adeyemi et al.1 reported a case of submasseteric abscess that occurred 1 month after submandibular displacement. The present case showed persistent dysaesthesia caused by an unsuccessful first surgical attempt by a practitioner. Moreover, the operator may be faced with legal implications related to this unsuccessful surgery12. Thus, it is prudent to stop the operation, inform the patient about the condition, and refer the patient to a maxillofacial surgeon as soon as possible22.
On the other hand, this complication can occasionally occur even in the hands of the most experienced surgeons32. Grandini et al.27 reported a case in which a dental surgeon caused the mandibular third molar to displace into the submandibular space and failed to retrieve the tooth for 6 hours, leading to severe tissue injury. Thus, in addition to surgical knowledge and experience, adequate pre-surgical planning, clinical and radiographic examinations, adequate access and visibility, proper technique, and controlled use of force are crucial for reducing the incidence and legal problems of this complication7.
Advanced imaging techniques are useful for thorough case evaluation when complications occur. Computed tomography is considered the most suitable technique and enables the exact location and size of the displaced tooth or tooth fragment to be pinpointed3. However, CBCT scanning, which has the advantage of low radiation exposure, can be used preferably if the fragment or tooth is displaced into deep spaces9. Panoramic, postero-anterior, submento-vertex, and occlusal views, in addition to image intensifiers, are among the other imaging modalities that can also be used to determine the location of displaced teeth or fragments26. We used CBCT to evaluate the fragment locations and sizes because this technique is already available in our Oral and Maxillofacial Surgery Clinic.
No clear consensus has been reached regarding the retrieval time of displaced teeth or their fragments. Some authors have suggested delaying tooth or fragment retrieval to allow fibrosis to develop1217, but others have claimed that delaying fragment removal can result in severe pain, infection, and further migration of the root or root fragment into deep facial spaces727. These authors suggest removal of the tooth or fragment as soon as possible. We conclude that if the fragment is small, is not accompanied by any symptoms, and is in a deep position, then it is better to keep the fragment under observation to prevent further tissue injuries. However, if the patient has symptoms associated with the displaced tooth or fragment and also has severe psychological distress, as in the present case, surgical removal of the fragment should be performed after explaining all possible complications to the patient.
Access to the submandibular space is difficult because of the anatomical structures enclosed by this space31. Many surgical approaches, including trans-oral approaches via general472226 or local anesthesia32527 and extra-oral approaches via local25 or general anesthesia1 have been reported. In 2002, Yeh28 reported a modified technique using a combination of intraoral and extraoral approaches to facilitate the retrieval of displaced teeth and fragments. In addition to the conventional lingual flap extended to the first molar, a hemostat was inserted to stabilize the fragment via a skin incision that was made in the submandibular region. Moreover, recent advancements in biotechnology computer-assisted navigation systems have enabled retrieval of displaced teeth in a matter of minutes3233. In the present case, adequate access and visualization were achieved with a preoperative CBCT scan and by carefully reflecting a deep lingual flap up to the submandibular region and supporting the flap extra-orally with digital pressure.
In conclusion, trans-operative displacement of a tooth or tooth fragment into the facial spaces is a rare but potentially serious condition, commonly requiring a second surgery. A second major procedure may cause further complications or worsen existing ones, as in our case. Thus, the best way to manage a surgical complication is prevention. This can be achieved by thorough evaluation of all significant risk factors and careful execution of the surgical procedure. Also, for optimal surgical outcomes, operation should be preferably performed by maxillofacial surgeons who are highly familiarized with the surgical morphology of the head and neck.
References
1. Adeyemi MO, James O, Lawal AO, Fadeyibi SO. Iatrogenic displacement of impacted mandibular third molar into the submandibular space complicated by submasseteric abscess. Afr J Trauma. 2016; 5:19–22.

2. Brauer HU. Unusual complications associated with third molar surgery: a systematic review. Quintessence Int. 2009; 40:565–572. PMID: 19626231.
3. Jolly SS, Rattan V, Rai SK. Intraoral management of displaced root into submandibular space under local anaesthesia: a case report and review of literature. Saudi Dent J. 2014; 26:181–184. PMID: 25382952.

4. Anand R, Patil PM. Accidental displacement of third molars; report of three cases, review of literature and treatment recommendations. Oral Surgery. 2013; 6:2–8.

5. Primo BT, Stringhini DJ, Klüppel LE, da Costa DJ, Rebellato LBR, de Moraes RS. Delayed removal of maxillary third molar displaced into the infratemporal fossa. Rev Esp Cir Oral Maxillofac. 2014; 30:78–81.

6. Tumuluri V, Punnia-Moorthy A. Displacement of a mandibular third molar root fragment into the pterygomandibular space. Aust Dent J. 2002; 47:68–71. PMID: 12035962.

7. Kamburoglu K, Kursun S, Oztas B. Submandibular displacement of a mandibular third molar root during extraction: a case report. Cases J. 2010; 3:8. PMID: 20148142.

8. De Biase A, Guerra F, Giordano G, Salucci S, Solidani M. Surgical removal of a left lower third molar root after iatrogenic displacement in soft tissue. Case report. Minerva Stomatol. 2005; 54:389–393. PMID: 16175168.
9. Silveira RJ, Garcia RR, Botelho TL, Franco A, Silva RF. Accidental displacement of third molar into the sublingual space: a case report. J Oral Maxillofac Res. 2014; 5:e5.

10. Shahakbari R, Mortazavi H, Eshghpour M. First report of accidental displacement of mandibular third molar into infratemporal space. J Oral Maxillofac Surg. 2011; 69:1301–1303. PMID: 21211881.

11. Selvi F, Cakarer S, Keskin C, Ozyuvaci H. Delayed removal of a maxillary third molar accidentally displaced into the infratemporal fossa. J Craniofac Surg. 2011; 22:1391–1393. PMID: 21772176.

12. Huang IY, Chen CM, Chang SW, Yang CF, Chen CH, Chen CM. Surgical management of accidentally displaced mandibular third molar into the pterygomandibular space: a case report. Kaohsiung J Med Sci. 2007; 23:370–374. PMID: 17606433.

13. Khan M, Mehboob B, Kundi JA. Pattern and management of iatrogenic displacement of teeth in maxillofacial anatomical spaces. Pak Oral Dent J. 2015; 35:186–189.
14. Xavier CB, Gonçalves FR, Batista SH, Veras Filho, Veras Filho Rde O. Spontaneous migration of third molar following displacement to pterygomandibular fossa. J Oral Maxillofac Surg. 2011; 69:1004–1007. PMID: 21193256.

15. Huang IY, Chen CM, Chuang FH. Caldwell-Luc procedure for retrieval of displaced root in the maxillary sinus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:e59–e63.

16. Ertas U, Yaruz MS, Tozoğlu S. Accidental third molar displacement into the lateral pharyngeal space. J Oral Maxillofac Surg. 2002; 60:1217.

17. Esen E, Aydoğan LB, Akçali MC. Accidental displacement of an impacted mandibular third molar into the lateral pharyngeal space. J Oral Maxillofac Surg. 2000; 58:96–97. PMID: 10632172.

18. Gay-Escoda C, Berini-Aytés L, Piñera-Penalva M. Accidental displacement of a lower third molar. Report of a case in the lateral cervical position. Oral Surg Oral Med Oral Pathol. 1993; 76:159–160. PMID: 8361724.
19. Ozer N, Uçem F, Saruhanoğlu A, Yilmaz S, Tanyeri H. Removal of a maxillary third molar displaced into pterygopalatine fossa via intraoral approach. Case Rep Dent. 2013; DOI: 10.1155/2013/392148.
20. Kocaelli H, Balcioglu HA, Erdem TL. Displacement of a maxillary third molar into the buccal space: anatomical implications apropos of a case. Int J Oral Maxillofac Surg. 2011; 40:650–653. PMID: 21211942.

21. Aznar-Arasa L, Figueiredo R, Gay-Escoda C. Iatrogenic displacement of lower third molar roots into the sublingual space: report of 6 cases. J Oral Maxillofac Surg. 2012; 70:e107–e115.

22. Kose I, Koparal M, Güneş N, Atalay Y, Yaman F, Atilgan S, et al. Displaced lower third molar tooth into the submandibular space: Two case reports. J Nat Sci Biol Med. 2014; 5:482–484. PMID: 25097443.
23. Roshanghias K, Peisker A, Zieron JO. Maxillary tooth displacement in the infratemporal fossa. Dent Res J (Isfahan). 2016; 13:373–375. PMID: 27605997.

24. Ho KH. Retrieval of a molar from the submandibular space--a case report. Singapore Dent J. 1980; 5:61–62. PMID: 6935776.
25. Solanki R, Khangwal M, Kumar D, Goel M. Retrieval of mandibular third molar tooth accidentally displaced in submandibular space: series of two cases. Indian J Dent. 2016; 7:105–108. PMID: 27433055.

26. Nusrath MA, Banks RJ. Unrecognised displacement of mandibular molar root into the submandibular space. Br Dent J. 2010; 209:279–280. PMID: 20871549.

27. Grandini SA, Barros VM, Salata LA, Rosa AL, Soares UN. Complications in exodontia--accidental dislodgment to adjacent anatomical areas. Braz Dent J. 1993; 3:103–112. PMID: 8241759.
28. Yeh CJ. A simple retrieval technique for accidentally displaced mandibular third molars. J Oral Maxillofac Surg. 2002; 60:836–837. PMID: 12089704.

29. Ozyuvaci H, Firat D, Tanyel C. Accidental displacement of a mandibular third molar: a case report. Quintessence Int. 2003; 34:278–280. PMID: 12731614.
30. Olusanya AA, Akadiri OA, Akinmoladun VI. Accidental displacement of mandibular third molar into soft tissue: a case report. Afr J Med Med Sci. 2008; 37:77–80. PMID: 18756859.
31. Bonala N, Kishan TV, Sri Pavani B, Murthy PV. Accessory belly of digastric muscle presenting as a submandibular space mass. Med J Armed Forces India. 2015; 71(Suppl 2):S506–S508. PMID: 26858485.

32. Campbell A, Costello BJ. Retrieval of a displaced third molar using navigation and active image guidance. J Oral Maxillofac Surg. 2010; 68:480–485. PMID: 20116728.

33. Guo Y, Xu DD, Lv K, Wan QL, Li ZB, Li Z. Use of computer-assisted navigation in the retrieval of accidentally displaced third molars. J Oral Maxillofac Surg. 2016; 74:889–894. PMID: 26850875.

Fig. 2
Cone-beam computed tomography scan showing the displaced roots in the right submandibular space on the transversal, coronal, and sagittal planes.
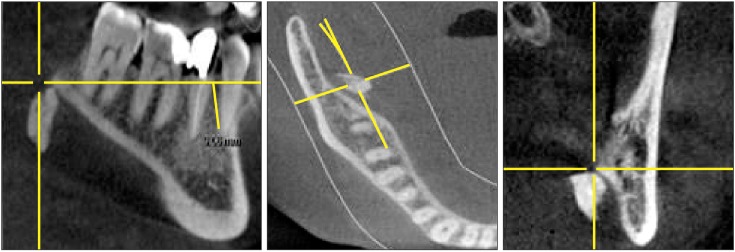
Table 1
Review of published cases of submandibular displacement
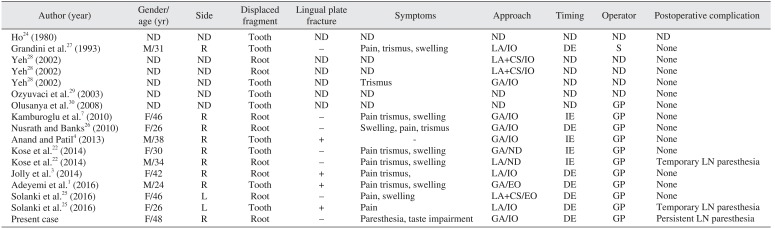
| Author (year) | Gender/age (yr) | Side | Displaced fragment | Lingual plate fracture | Symptoms | Approach | Timing | Operator | Postoperative complication |
|---|---|---|---|---|---|---|---|---|---|
| Ho24 (1980) | ND | ND | Tooth | ND | ND | ND | ND | ND | ND |
| Grandini et al.27 (1993) | M/31 | R | Tooth | − | Pain, trismus, swelling | LA/IO | DE | S | None |
| Yeh28 (2002) | ND | ND | Root | ND | ND | LA+CS/IO | ND | ND | None |
| Yeh28 (2002) | ND | ND | Root | ND | ND | LA+CS/IO | ND | ND | None |
| Yeh28 (2002) | ND | ND | Tooth | ND | Trismus | GA/IO | ND | ND | None |
| Ozyuvaci et al.29 (2003) | ND | ND | Tooth | ND | ND | ND | ND | ND | None |
| Olusanya et al.30 (2008) | ND | ND | Tooth | ND | ND | ND | ND | GP | None |
| Kamburoglu et al.7 (2010) | F/46 | R | Root | − | Pain trismus, swelling | GA/IO | IE | GP | None |
| Nusrath and Banks26 (2010) | F/26 | R | Root | − | Swelling, pain, trismus | GA/IO | DE | GP | None |
| Anand and Patil4 (2013) | M/38 | R | Tooth | + | - | GA/IO | IE | GP | None |
| Kose et al.22 (2014) | F/30 | R | Tooth | − | Pain trismus, swelling | GA/ND | IE | GP | None |
| Kose et al.22 (2014) | M/34 | R | Root | − | Pain trismus, swelling | LA/ND | IE | GP | Temporary LN paresthesia |
| Jolly et al.3 (2014) | F/42 | R | Root | + | Pain trismus, | LA/IO | DE | GP | None |
| Adeyemi et al.1 (2016) | M/24 | R | Tooth | + | Pain trismus, swelling | GA/EO | DE | GP | None |
| Solanki et al.25 (2016) | F/46 | L | Root | − | Pain, swelling | LA+CS/EO | DE | GP | None |
| Solanki et al.25 (2016) | F/26 | L | Tooth | + | Pain | LA/IO | DE | GP | Temporary LN paresthesia |
| Present case | F/48 | R | Root | − | Paresthesia, taste impairment | GA/IO | DE | GP | Persistent LN paresthesia |




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download