I. Introduction
Focal osteoporotic bone marrow defect (FOBMD) is a radiolucent area corresponding to the uncommon presence of hematopoietic tissue found in the jaws, usually at former extraction sites
1,
2. The lesion is usually asymptomatic and is incidentally detected during radiographic analysis. Radiographi-cally, it is localized, poorly demarcated radiolucency that varies in size, trabeculae, and border definition
2-
4.
Since FOBMD is occasionally included in the differential diagnosis of radiolucent lesions of the jaws, knowledge of the radiographic, clinical, and histopathological characteristics in association with accurate examination are mandatory to distinguish it from other most common intrabony defect lesions such as odontogenic cysts or traumatic bone cyst (TBC), aneurismal bone cyst, central giant cell granuloma, tumors, and primary or metastatic malignancies
2.
Placement of dental implant has become a quite predictable procedure; nonetheless, there are risks associated with the surgical phase. Well-known intraoperative complications and accidents related to surgery include nerve damage, thermal damage, hemorrhage, damage of adjacent tooth, lack of primary stability, and displacement of implants.
The displacement of implants occurs intraoperatively or within a short period because of insufficient surgical technique or anatomical variances of the jaws. Deficiency of initial stability of implants can result from the low density of trabecular bone, thinness of the cortical bone, and osteopenia or osteoporosis; problems related to the use of surgical technique by an inexperienced operator, such as inadequate planning, overworking of the implant drilling, mishandling, and incorrect manipulation, have also been suggested as possible factors
5,
6. The investigators concluded that the medullar component in the posterior mandible may be similar to that found in the maxilla, and that it could facilitate the displacement of dental implants during surgery
5.
In this report of 3 rare cases, the displacement of implants into the mandible corpus and its management are presented together with a review of literature on FOBMD.
Go to :

III. Discussion
FOBMD of the jaws has been reported as an unusual radiolucency often detected fortuitously in the posterior mandible of a middle-aged woman
2,
7-
9. Radiographically, this radiolucency varies in size from several millimeters to centimeters in diameter, and the shape and borders are ill-defined with fine central trabeculation
1,
3,
9. The lesion frequently occurs in an edentulous region where tooth extraction was previously performed
4,
7. The pathogenesis of the lesion is not confirmed. Various theories include the following: aberrant bone regeneration after tooth extraction; persistence of fetal marrow, and; marrow hyperplasia in response to increased demand for erythrocytes
9. Some osteoporotic bone marrow defects (OBMDs) are multifocal; others are bilateral, and few of them are symptomatic
1-
4. More than 75% of all cases are discovered in adult women. About 70% occur in the posterior mandible, often in edentulous areas. No clinical and radiological expansion of the jaw is noted
9. According to the study conducted by Shankland and Bouquot
4, the bilateral occurrence of OBMD within the jaws affected 3% of patients. Previous OBMDs documented in English literature frequently indicate that the radiographic appearance may be confused with other intraosseous patho-logic conditions
1-
4,
7,
8. Mandibular cysts or tumors often have bilateral radiolucency with indistinct margins. Based on age, site, and clinical and radiographic findings, OBMD was considered a differential diagnosis. The final diagnosis of OBMD should be established on microscopic features
1,
4. Microscopically, the existence of hematopoietic marrow composed of erythroid, monocytic, granulocytic, and lympho-cytic series as well as megakaryocytes associated with fatty marrow is required for the diagnosis of this lesion
4,
7-
9.
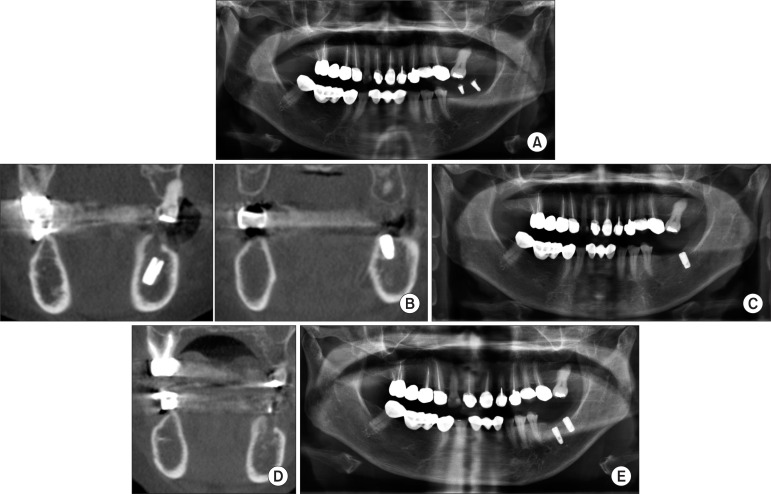
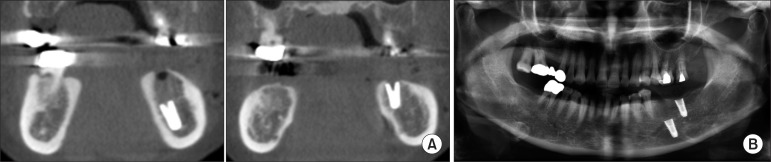
FOBMD was considered a differential diagnosis based on age, site, and clinical and radiographic findings without biopsy for all our cases. Radiologically, cortical bone density and thickness were at normal levels; the endosteal cortical margin was even, and there were no cystic epithelial walls.(
Figs. 1-
3) The cancellous bone marrow was almost absent, and the pattern with hematopoietic marrow tissue was filled roughly. Our CBCT imaging showed the weakness of bone marrow density near the mandibular canal of the molar area.(
Figs. 1. A,
2. B, and
3. A) Thus, we diagnosed our 3 patients as FOBMD based on age, site, and clinical and radiographic findings.
TBCs
10 of the jaws are asymptomatic cystic lesions detected incidentally on radiographs or during surgery. The lesion is mainly diagnosed among young patients most frequently during the second decade of life, with men affected somewhat more frequently. Expansion of the cortical plate of the jaw bone is often noted, usually buccally, resulting in intraoral and extra-oral swelling. TBC, or extension of the empty bone cavity, will stop expanding once the cortical bone has been reached. A characteristic of TBC is the "scalloping effect" when extending between the roots of the vital teeth
10. Preoperatively, we could not detect any radiolucency to confirm diagnosis of TBC radiographically. A histological examination of TBC revealed normal-looking bone spicules with parts of vascular connective tissue. Occasional hemosiderin-laden macrophages were also noted
10. Nonetheless, FOBMD frequently occurs in an edentulous region of a middle-aged woman, and a radiolucent appearance is usually not observed on the preoperative panoramic radiograph
2. Based on the panoramic view of our patients, we could not detect any cystic lesion on the mandible (
Figs. 1. B,
2. B, and
3. B), finding that the cancellous bone marrow was almost nonexistent based on CBCT imaging.(
Figs. 1. A,
2. B, and
3. A)
Whether the lesion is TBC or OBMD, the radiolucent appearance of a possible lesion was more likely not observed on the preoperative panoramic radiograph
5. Bender and Seltzer
11 showed that the removal of cancellous bone from the posterior region of cadaver mandibles did not alter the radiographic appearance of the trabeculae. It was only when the endosteal surface of the cortical bone was removed was the radiographic image altered.
None of our patients had a medical history of osteoporosis. Note, however, that osteoporosis is very common particularly among postmenopausal women. The lesion is characterized by decrease in bone mass and strength
5. Vlasiadis et al.
12 demonstrated that later postmenopausal date and number of tooth loss were related to higher degree of osteoporosis. Studies of subjects with osteoporosis have shown no differences in the survival of implants compared with healthy subjects; a review of the published data did not find evidence that osteoporosis could be a risk factor for osseointegrated dental implants
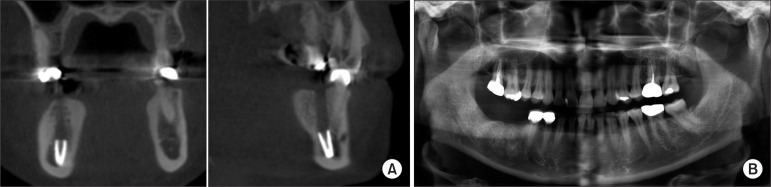
13. The #37 (4.5 mm wide, 8.0 mm long) implant placed simultaneously with #36 (4.5 mm wide, 10.0 mm long) had good initial stability.(
Figs. 2. B, 2. C) Note, however, that only the #36 implant fell down into the mandible body.(
Fig. 2B) Three months later, the replacement of the #36 implant (4.0 mm wide, 10 mm long) was performed with autogenic and xenogenic bone graft. The bone grafts were made on the upper third portion of the implant. It had three walled defects, but primary stability was sufficient. Six months after the #37 implant placement and three months after the #36 implant replacement (
Fig. 2E), delivery of prosthetics was carried out, and healing proceeded uneventfully without any postoperative complication.
The displacement of an implant will occur intraoperatively or within a short period due to the poor use of surgical technique by an inexperienced operator or anatomical variances. Failure of initial implant stability can result from low trabecular bone density, decreased thickness of the cortical bone, anatomical variances, and osteopenia or osteoporosis; problems related to the use of surgical technique by an inexperienced operator, such as inadequate planning, overworking of the implant drilling, mishandling, and incorrect manipulation, have also been suggested as possible factors
5,
6. According to Theisen et al.,
14 during the tightening of the healing screw, the implant was displaced inferiorly into the preparation, and attempts to remove the screw and retrieve the implant body resulted in the further inferior displacement of the implant body. One case (case 1) exhibited hypoesthesia of lower lip and chin. She already had hypoesthesia on the lower lip when she visited our dental center. Thus, we assumed that the nerve had been damaged when the implant fell down into the mandible.
Although dental implant surgery is considered a simple and predictable procedure, unforeseen complications and rare accidents could occur especially in the posterior segments with lower trabecular bone density than in anterior segments. As previously reported by Theisen et al.,
14 when the location of the inferior alveolar canal could not be delineated on a panoramic radiograph, large medullary components could be detected on the CT section. Thus, additional radiographic evaluations such as preoperative CT may be necessary for patients whose molar teeth were extracted much earlier in their life, particularly among postmenopausal women. Operators should take care against implant displacement into FOBMD. We recommend securing the healing screw in the implant body prior to the placement of the implants. Even if implants fall down into FOBMD, removal of the implants was performed carefully without any damage to nerve and vessel bundles, and replacement of implants was done as a common method of immediate placement after teeth extraction. Nonetheless, additional studies with more cases and long-term follow-up should be conducted.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download