Abstract
The objectives of the present study were to study the prevalence of the parietal emissary vein in adult South Indian population and to study the distance of foramen from the sagittal suture. There were 58 adult human skulls in the present study which were available at the anatomy department of our institution. The study included 116 parietal bones which have been observed macroscopically for the number, prevalence and topography of the emissary foramen. The emissary foramen was present in 83 parietal bones (71.5%) of the present study. It was present at the junction between the middle 1/3 and posterior 1/3 region of the parietal bone. The foramen was observed solitary in 73 parietal bones (62.9%), double in 8 bones (6.9%), and triple in 2 parietal bones (1.7%). The foramen was not observed in 33 parietal bones (28.4%). The bilateral absence of parietal emissary foramen was seen in 7 skulls (12.1%). It was absent unilaterally in 19 skulls (32.7%). The accessory foramina were seen in only 8 skulls (13.8%). The mean distance of the foramen from the sagittal suture was 6.7±2.9 mm and 6.8±2.8 mm on the right and left sides respectively. The prevalence of parietal emissary vein in the present study was 71.5%. The present study has observed important data about the morphology and morphometry of the parietal emissary vein in South Indian population. The identification of parietal emissary veins and accessory veins is important in the operation room to prevent the blood loss.
The parietal foramina are the symmetrical, oval openings in the skull vault which are located one on either side of the sagittal suture at the posterior aspect of the parietal bone. They are separated from each other by a narrow bridge of bone [1]. They are usually located at the junction between the middle 1/3 and posterior 1/3 of the parietal bone [2]. A bony point over the sagittal suture which is just medial to the parietal foramina is given the name obelion. The name 'obelion' has been derived because of its resemblance to the Greek symbol 'obelos'(÷). The line in the symbol '÷', represents the sagittal suture and the dots represent the bilateral parietal foramina [3]. The parietal foramina have sharply delineated margins and they do not have the surrounding sclerosis. Radiologist should be able to distinguish this foramen from the lytic lesions of the skull. The parietal foramen is smaller than the burr hole of the neurosurgeon; it transmits a bridging vein which connects the extracranial scalp veins with the superior sagittal dural venous sinus. On few occasions, this foramen may transmit a smaller branch arising from the occipital artery. It was described that the parietal foramen is not constantly present and is being subjected to the anatomical variations with respect to its topography, size, number and shape [45].
The fourth layer of the scalp contains the loose areolar tissue and is considered as the dangerous area of the scalp, because it is traversed by the parietal emissary vein. The emissary foramina in man have received attention from many authors [6], since they get involved in the pathways from which the infection is carried to the cranial cavity. All the cranial foramina which transmit an emissary vein are not considered as the emissary foramina. In the routine usage, the term is applied to the parietal foramen, mastoid foramen, condylar foramen and the sphenoidal emissary foramen. It can also include foramen in the occipital bone and the foramen caecum. The emissary foramina are commonly described as the channel for the emissary vein [6]. There are only a few Indian studies [78910] available in literature about the emissary foramina in the occipital, condylar, mastoid and sphenoid bones; however, the studies about the parietal emissary foramina are not found in the medical literature. This was the stimulus to perform this present investigation from the anatomical specimens. The objectives of the present study were to study the prevalence of the parietal emissary vein in adult South Indian population and to study their distance from the sagittal suture. The prevalence of the parietal emissary foramen was compared with the prevalence of other emissary veins of the skull. This was possible by referring our previous reports which had examined the same adult skull specimens from South Indian population.
There were 58 adult human dried crania in the present study. These crania were present at the Department of Anatomy. One hundred and sixteen parietal bones were examined for the number and topography of the emissary foramen. The crania which exhibited the pathological changes of the skull cap were not included. All the crania were examined by the same person and the data were recorded. The foramina were macroscopically observed by using a magnifying lens and a needle was probed into each foramen to check their patency. The morphometric data of the present study was performed by using a divider and the measuring scale. The data are presented as mean±SD and were tabulated.
The emissary foramen was observed in 83 parietal bones (71.5%) of the present study. It was located at the junction between the middle 1/3 and posterior 1/3 region of the parietal bone. It was bilaterally present (Fig. 1A) in 32 skulls (55.2%) and unilaterally present (Fig. 1B) in 19 skulls (32.7%). The bilateral absence (Fig. 1C) of parietal emissary foramen was seen in 7 skulls (12.1%). The frequency of distribution of the number of emissary foramen in the parietal bones is shown in Fig. 2.
Table 1 shows the side wise comparison of the frequency of the number of emissary foramen in the parietal bones of the present study. The foramen was solitary in 73 parietal bones (62.9%), two (Fig. 1D) in 8 parietal bones (6.9%), and three (Fig. 1E) in 2 parietal bones (1.7%). This foramen was absent in 33 parietal bones (28.4%). The parietal emissary foramina were present in multiple (accessory) in only 8 skulls (13.8%). The mean distance of the emissary foramen from the sagittal suture was 6.7±2.9 mm and 6.8±2.8 mm on the right and left sides respectively. The distance of the foramen from the sagittal suture ranged from 0.5 mm to 13 mm and 1 mm to 15 mm on the right and left sides respectively. Table 2 shows the side wise comparison of the range of distance of the foramen from the sagittal suture. There were 2 skulls in the present study (3.4%), which exhibited the parietal foramen over the sagittal suture (Fig. 1F).
The prevalence of the parietal emissary foramen of present study has been compared with the previous reports and is represented in Table 3. The comparison was also done among the different emissary foramina of the South Indian skull, which is given in Table 4. This was possible by referring our previous reports [78910], which were also from the same South Indian adult skull specimens.
The parietal bone develops from the intramembranous ossification at the 8th week of intrauterine life. The ossification center is being located near the parietal eminence and later it radiates towards the periphery in a sunburst pattern [1112]. The four borders of the parietal bone join each with the frontal bone, temporal bone, sphenoid bone, occipital bone and the contralateral parietal bone. The parietal bones form the side and roof of the cranium [13]. It has been reported that the prolonged ossification of the posterior parietal region at obelion would lead to a v-shaped notch, which is given the name, subsagittal suture of Pozzi [14] and pars obelica [15]. The parietal bone ossification may vary and is essential to know about it to learn the architecture of the sagittal suture near the obelion. The formation of sagittal suture is achieved by the closure of 3 fontanelles, the anterior fontanelle which is present in between the frontal and parietal bones, the posterior fontanelle in between the parietal and occipital bones and the third fontanelle. The third fontanelle is also known as the sagittal fontanelle and is present in 50%-80% of cases, leading to the formation of unilateral or bilateral parietal foramina. It has been described that the third fontanelle usually closes within the first two years of life [15]. The variations in the closure of the third fontanelle would lead to formation of obeliac bones, accessory parietal emissary foramen, enlarged parietal foramen and the parietal fissure [16].
The emissary veins drain the neurocranium and cephalic structures. They do have valves; still the blood can go in both the directions. Usually the blood flow is sluggish during the normal situation, but they help in the drainage of blood and would relieve the intracranial tension in a situation like raised intracranial pressure [17]. The function of the parietal foramen, other than transmitting the vessels is not clear and is still under investigation [18]. It is believed that the emissary foramina are typically a character of the humans, they are less frequent in lower animals and in some species they are absent [6]. It has been reported that, there exists an important relationship between the emissary foramina and the diploic veins of the skull, which are involved in the spread of infection from the extracranial to intracranial [6]. It is described that the topography of the parietal foramen varies within a limited range [6]. The parietal foramen is seen bilaterally, however may appear unilateral only and sometimes it is absent [19]. In the neonates, the parietal emissary foramen is observed 2 cm in front of the lambda and in adults it becomes 2-5 cm in front of the inion [4]. In other words the parietal emissary foramen becomes still posterior in the adults.
The incidence of parietal emissary foramen ranges from 50%-80% among the various population groups [45]. The comparison of the prevalence of parietal emissary foramen with previous reports is represented in Table 3. Among our specimens, the prevalence of foramen was higher in comparison to the data of Yoshioka et al. [5] and Boyd [6] studies. Perhaps this is because of the racial variations and our materials were entirely different from them, as they performed the study by using the cadaveric scalps. Boyd [6] reported that the unilateral parietal foramen is seen more common on the right side than the left (20.7%:15.2%). Yoshioka et al. [5] studied 40 parietal regions from the 20 adult cadavers and they observed that each foramen transmitted an anastomotic vessel between the middle meningeal artery and extra cranial arteries. In 55% of cases, there was an anastomosis between superficial temporal and occipital arteries. A branch from this anastomosis was piercing the parietal foramen and it joined with branch of the middle meningeal artery. Rest of the cases (45%) had an anastomosis between the middle meningeal artery and a small artery in the pericranium. The anastomosis was observed to be passing through the parietal emissary foramen. It was opined that this anastomosis is involved in several pathological conditions. In the present study, we could not able to study the vessels and their anastomosis at the parietal foramen, since we performed the study by using the dried skulls.
The variability in the number of parietal foramen is due to the difference in the ossification of the anterior fonticulus [2]. Yoshioka et al. [5] reported that, there may be existence of a transverse suture at one or both sides of the obelion. However that morphology of suture was not observed in any of our specimens. In the study by Boyd [6], the median foramen over the sagittal suture was present in 5.9% cases. This is almost similar to the present study as we observed the median foramen over the sagittal suture in 3.4% of cases. Boyd [6] observed the accessory parietal foramina in 2%-5% of cases. The present study observed a slightly higher frequency and the accessory parietal emissary foramina were present in 13.8% skulls. The reason may be due to the racial and geographical variations.
The study from Mann et al. [16], reported that the sagittal suture will become complex if the parietal foramina are very close each other. They hypothesized that the parietal foramen, may alter and change the direction of the tensile and compressive forces which would lead to a simpler sagittal suture. It has been reported that, if a parietal foramen is larger due to its delayed ossification, the area surrounding it may become thinner and flatter [6]. The delayed ossification may be the reason for the simple morphology of the sagittal suture near the obelion [15]. It is also true that, the complexity of the sagittal suture at the parietal foramen would result in excessive growth of the bone. There will be premature fusion of the suture due to the abnormal fibroblast growth factor and it would lead to osteogenesis imperfecta and the craniofacial malformations [2021]. The distance of the parietal emissary foramen from the sagittal suture is clinically essential. The knowledge is important to the neurosurgical perspective as the emissary veins may be ruptured during the surgical procedure and cause spontaneous bleeding. The present study has provided the data on the distance of the foramen from the sagittal suture. This is novel information and was not available from the South Indian sample.
Le Double [22] opined that the parietal foramina are often absent in White races than in the other primitive races. Boyd [6] reported that the parietal foramina are larger in Australian and New Zealand people than the other races. In the present study from South Indians, it was observed that the parietal emissary foramen was not of larger in size. The parietal foramen is considered as a normal finding of the skull, however it becomes abnormal if it is found with a larger opening [4]. Few authors [2324] reported the abnormally large parietal foramina in their studies. In the present study, we did not observe any such abnormally larger parietal foramen. Perhaps those types of foramina are due to variability in the ossification of the parietal bones [4]. It has been reported that they are not usually associated with an emissary vein [6]. The emissary veins act like safety valves in equalizing the intracranial pressure and sometimes they get enlarged if there is any underlying space occupying lesion. It is advised that, during the clinical examination and the surgical procedures, the possibility of an enlarged parietal foramen should be kept in mind. This has to be differentiated from the other deficiencies in the calvaria.
The osteomyelitis of the cranial vault, meningitis and cerebral abscess are the possible complications due to the infection at the diploic, meningeal and cerebral veins which communicate along with the emissary veins [6]. Boyd [6] reported that Piersol, an author of a text book mentioned that, 'if there were no emissary veins, the injuries and diseases of the scalp would lose half their frequency'. Identification of the emissary foramina is critical for understanding the regional vessels and to distinguish them from the abnormal structures [2]. The misinterpretation would lead to complications like catastrophic bleeding and the treatment failure. The parietal emissary foramina may be absent in a considerable number of people. Perhaps this is the reason in some cases of severe scalp sepsis with no intracranial complications [6]. The knowledge about this foramen is clinically essential since it transmits an emissary vein connecting the extra cranial veins with the superior sagittal dural venous sinus. This plays a role in the spread infection into the dural venous sinuses [19]. The veins may be responsible for the spread of infections like meningitis and the bacterial infection of the central nervous system. The present study has provided additional information about the number, frequency and topography of the parietal foramen. The identification of these veins will prevent the blood loss during the neurological surgery.
The present study compared the prevalence of parietal emissary vein with the other emissary veins of the skull from the same South Indian population. This comparison was possible after referring our previous publications [78910] and this comparison is given in the Table 4. It was observed that the parietal emissary veins have a higher prevalence, which is next to the prevalence of mastoid emissary veins in the South Indian population.
The present study has certain limitations like the male and female differences which are not studied. The in vivo study of the foramen can be done by using the radiological films and computed tomogram scans. The size of the foramen can be estimated by using the computerized software and also by the radiological methods. There are few studies available, which classified the shape of the parietal foramen into circular shape, oval shape and fissure type [252627]. The present study could not able to make the segregation of the different shapes of the parietal foramen.
There is an increased interest in studying the non-metrical cranial traits, which include the study of anatomical variants in relation to the foramina of nerves and vessels of the skull [28]. The present study has provided additional data about the morphology and morphometry of the parietal emissary foramina. The data is given for the accessory parietal emissary foramina, their unilateral and bilateral presence. The present study provided the data on distance of the parietal foramen from the sagittal suture, which has not been reported earlier in the literature. It was observed that the most of the foramina were located about 4-8 mm away from the sagittal suture. The comparison of the data with the previous observations from the same population showed that the parietal emissary vein is common in occurrence among all the other emissary veins of the skull, which is only next to the prevalence of mastoid emissary vein. We believe that the study of the parietal emissary foramina is being reported for the first time among the South Indian literature and it is considered that the findings are of novel importance. We believe that the present study will be enlightening to the neurosurgeon and radiologist. The morphological understanding of the structures will set a trend to open more and more contents into clinical considerations [1].
Figures and Tables
Fig. 1
The crania of the present study. (A) Bilateral presence (arrows) of the parietal emissary foramen (55.2%). (B) The unilateral presence (arrow) of the parietal emissary foramen (32.7%). (C) The bilateral absence of the parietal emissary foramen (12.1%). (D) Right parietal bone showing the double (arrows) emissary foramina (3.5%). (E) Right parietal bone showing the triple (arrows) emissary foramina (0.9%). (F) The parietal emissary foramen (arrow) over the sagittal suture (3.4%).

Fig. 2
The frequency of distribution of the number of emissary foramen in the parietal bones of the present study (n=116).

Table 1
Sidewise comparison of the number of foramen in the parietal bones (n=116)
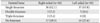
| Parietal bone | Right sided (n=58) | Left sided (n=58) |
|---|---|---|
| Single foramen | 36 (62.1) | 37 (63.8) |
| Double foramen | 3 (5.2) | 5 (8.6) |
| Triple foramen | 2 (3.4) | 0 (0) |
| No foramen | 17 (29.3) | 16 (27.6) |
Table 2
Sidewise comparison of range of distance of the foramen from the sagittal suture
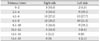
Table 3
Comparison of frequency of parietal emissary foramen with previous reports
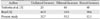
| Author | Unilateral foramen | Bilateral foramen | Absent foramen |
|---|---|---|---|
| Yoshioka et al. [5] | 20 | 40 | 40 |
| Boyd [6] | 40.5 | 19.9 | 39.6 |
| Present study | 32.7 | 55.2 | 12.1 |
Table 4
Comparison of frequency of emissary foramen in the skull at different regions
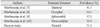
| Authors | Emissary foramen | Prevalence (%) |
|---|---|---|
| Murlimanju et al. [7] | Mastoid | 91.7 |
| Murlimanju et al. [8] | Occipital | 14.1 |
| Murlimanju et al. [9] | Sphenoidal | 37.2 |
| Murlimanju et al. [10] | Paracondylar | 33.3 |
| Present study | Parietal | 71.5 |
Acknowledgements
The authors are sincerely thankful to all their nonteaching staff members of the department of anatomy for the assistance offered during this study.
References
1. Currarino G. Normal variants and congenital anomalies in the region of the obelion. AJR Am J Roentgenol. 1976; 127:487–494.
2. Freire AR, Rossi AC, De Oliveira VC, Prado FB, Caria PH, Botacin PR. Emissary foramens of the human skull: anatomical characteristics and its relations with clinical neurosurgery. Int J Morphol. 2013; 31:287–292.
3. Jamieson EB. Dixon's manual of human osteology. 2nd ed. London: Humphrey Milford;1937.
4. Wysocki J, Reymond J, Skarzyński H, Wróobel B. The size of selected human skull foramina in relation to skull capacity. Folia Morphol (Warsz). 2006; 65:301–308.
5. Yoshioka N, Rhoton AL Jr, Abe H. Scalp to meningeal arterial anastomosis in the parietal foramen. Neurosurgery. 2006; 58:ONS123–ONS126.
6. Boyd GI. The emissary foramina of the cranium in man and the anthropoids. J Anat. 1930; 65:108–121.
7. Murlimanju BV, Chettiar GK, Prameela MD, Tonse M, Kumar N, Saralaya VV, Prabhu LV. Mastoid emissary foramina: an anatomical morphological study with discussion on their evolutionary and clinical implications. Anat Cell Biol. 2014; 47:202–206.
8. Murlimanju BV, Prabhu LV, Pai MM, Jaffar M, Saralaya VV, Tonse M, M DP. Occipital emissary foramina in human skulls: an anatomical investigation with reference to surgical anatomy of emissary veins. Turk Neurosurg. 2011; 21:36–38.
9. Murlimanju BV, Reddy GR, Latha VP, Vasudha VS, Rao CP, Mangala MP, Ashwin K, Rajanigandha V. Foramen of Vesalius: prevalence, morphology, embryological basis and clinical implications. J Surg Acad. 2015; 5:24–28.
10. Murlimanju BV, Chettiar GK, Krishnamurthy A, Pai MM, Saralaya VV, Prabhu LV, Vadgaonkar R. The paracondylar skull base: anatomical variants and their clinical implications. Turk Neurosurg. 2014; 25:844–849.
11. Hoheisel WF. An anomalous Indian occiput. Anat Rec. 1930; 45:129–135.
12. Steele DG, Bramblett CA. The anatomy and biology of the human skeleton. College Station, TX: Texas A & M University Press;1988.
13. Snell RS. Clinical anatomy. 7th ed. Philadelphia, PA: Lippincott Williams and Wilkins;2004.
14. Breathnach AS. Frazer's anatomy of the human skeleton. 6th ed. London: J&A Churchill Ltd.;1965.
15. Scheuer L, Black SM. The juvenile skeleton. Amsterdam: Elsevier Academic Press;2004.
16. Mann RW, Manabe J, Byrd JE. Relationship of the parietal foramen and complexity of the human sagittal suture. Int J Morphol. 2009; 27:553–564.
17. Reis CV, Deshmukh V, Zabramski JM, Crusius M, Desmukh P, Spetzler RF, Preul MC. Anatomy of the mastoid emissary vein and venous system of the posterior neck region: neurosurgical implications. Neurosurgery. 2007; 61:5 Suppl 2. 193–200.
18. Wu YQ, Badano JL, McCaskill C, Vogel H, Potocki L, Shaffer LG. Haploinsufficiency of ALX4 as a potential cause of parietal foramina in the 11p11.2 contiguous gene-deletion syndrome. Am J Hum Genet. 2000; 67:1327–1332.
19. Sicher H, DuBrul EL. Oral anatomy. 6th ed. Rio de Janeiro: Guanabara Koogan;1977.
20. Moore R, Ferretti P, Copp A, Thorogood P. Blocking endogenous FGF-2 activity prevents cranial osteogenesis. Dev Biol. 2002; 243:99–114.
21. Sarkar S, Petiot A, Copp A, Ferretti P, Thorogood P. FGF2 promotes skeletogenic differentiation of cranial neural crest cells. Development. 2001; 128:2143–2152.
22. Le Double AF. Traite des variations des os du crane de l'homme, et de leur signification au point de vue de l'anthropologie zoologique. Préface d' Edmond Perrier. Paris: Vigot Freres;1903. p. 67p. 116–124. p. 176p. 317–323. p. 333
23. Griessenauer CJ, Veith P, Mortazavi MM, Stewart C, Grochowsky A, Loukas M, Tubbs RS. Enlarged parietal foramina: a review of genetics, prognosis, radiology, and treatment. Childs Nerv Syst. 2013; 29:543–547.
24. Stibbe EP. Skull showing perforations of parietal bone, or enlarged parietal foramina. J Anat. 1929; 63(Pt 2):277–278.
25. Keats TE. Atlas of normal roentgen variants that may simulate disease. 5th ed. St. Louis, MO: Mosby Year Book;1992.
26. Mann RW. Enlarged parietal foramina and craniosynostosis in an American Indian child. AJR Am J Roentgenol. 1990; 154:658.
27. O'Rahilly R, Twohig MJ. Foramina parietalia permagna. Am J Roentgenol Radium Ther Nucl Med. 1952; 67:551–561.
28. Kaur J, Srivastava D, Singh D, Raheja S. The study of hyperostosic variants: significance of hyperostotic variants of human skulls in anthropology. Anat Cell Biol. 2012; 45:268–273.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download