Abstract
Background
Although there are several available management strategies for treatment of both acute pain of herpes zoster (HZ) and postherpetic neuralgia (PHN), it is difficult to treat them adequately.
Objective
The aim of this study was to evaluate the efficacy of intravenously administrated vitamin C on acute pain and its preventive effects on PHN in patients with HZ.
Methods
Between September 2011 and May 2013 eighty-seven patients who were admitted for HZ were assessed according to age, sex, underlying diseases, duration of pain and skin lesion, dermatomal distribution, and PHN. It was a randomized controlled study, in which 87 patients were randomly allocated into the ascorbic acid group and control group. Each patient received normal saline infusion with or without 5 g of ascorbic acid on days 1, 3, and 5 then answered questionnaires that included side effects and pain severity using visual analogue scale on days 1, 2, 3, 4, and 5. After discharge, the severity of pain was obtained at out-patient clinic or by telephone on weeks 2, 4, 8, and 16.
Results
There was no differences in severity of pain on patients' age, sex, underlying diseases, duration of pain and skin lesion and dermatomal distribution between two groups (p>0.05). Since 8th week, pain score in ascorbic acid treatment group was significantly lower than control group (p <0.05). The incidence of PHN was significantly lower in the treatment group compared to control group (p=0.014). The changes of overall pain score was significantly different between the two groups (p<0.05).
Herpes zoster (HZ) is an acute skin disease that occurs after primary varicella-zoster virus infection. The virus remains dormant within the dorsal root ganglia and becomes reactivated by the factors that reduce cell-mediated immunity, traveling down the sensory root ganglia to cause acute pain and vesicular eruption123. HZ can cause pain during the acute phase, as well as various complications and sequelae, including postherpetic neuralgia (PHN), encephalomyelitis, and neural paralysis, even after treatment3. Specifically, PHN persists for 1∼6 months even after improvement in cutaneous eruption. Its incidence varies with definition, ranging from 8%∼15%. It reduces the patient's quality of life because of physical disability and mental disorders34. Treatment of HZ aims for quick recovery of skin lesions, reduce the intensity and duration of acute pain, and decrease the incidence of complications such as PHN56. Antiviral drugs, analgesic drugs, lower level laser therapy, and preventive vaccines have been used to alleviate acute pain and PHN; however, treatment of HZ still remains a challenge257.
It has been reported that patients with viral infections showed vitamin C deficiency8. Vitamin C deficiency has been found to play an important role in the pathogenesis of herpes infection and occurrence of PHN910. Several studies reported that intravenous (IV) injection of vitamin C is effective in treating acute pain from HZ and PHN111213. However, disputes remain regarding the appropriateness of using vitamin C to treat HZ14.
In South Korea, the idea of IV injection of vitamin C to patients with HZ remains incomplete. There are several studies about IV injection of vitamin C twice a day without any side effect. The effect of vitamin C has been reported at a dose of 2.5 g in PHN and at a dose of 7.5 g, 15 g in acute phase111213. Therefore, we designed a study with a dose 5 g of vitamin C injection every two days and we assessed the therapeutic effects of IV injection of it on patients who were diagnosed with HZ and were hospitalized.
Of the 128 patients diagnosed with HZ and hospitalized at Department of Dermatology, Chosun University Hostpital (Gwangju, Korea) between September 2011 and May 2013, 87 were surveyed. This protocol confirmed to the guidelines of the Helsinki Declaration in 1975 and was approved by the institutional review board of Chosun University Hospital, Gwangju, Korea (IRB no. CHOSUN 2015-09-004-003). Patients who received any antiviral medications from a different hospital, who were discharged within 5 days, took analgesic anti-inflammatory drugs to control pain before admission, or were not followed-up after discharge were excluded.
Eighty-seven patients hospitalized for HZ were randomly divided into a vitamin C treatment group and a control group. All patients were intravenously injected with 5 mg/kg of acyclovir for 5 days and orally treated with 100 mg of gabapentin and analgesics (acetaminophen 250 mg/ibuprofen 200 mg/codeine phosphate 10 mg mixture) three times a day to control pain. After discharge, all patients took same dose of analgesics and gabapentin for 1 month. The vitamin C treatment group was provided with a mixture of 100 ml normal saline water and 5 g ascorbic acid on the first, third, and fifth days. The patients in the control group received only 100 ml of normal saline water intravenously. Data on age, sex, underlying diseases, duration and intensity of pain, duration of skin lesions, involved dermatome, PHN, and injection-related complications were collected for all patients.
Visual analogue scale (VAS) score was used on the first, second, third, fourth, and fifth days of admission and second, fourth, eight, and sixteenth week of follow-up to measure pain intensity, which was assessed using a scale of 10 (most painful) to 0 (no pain), depending on the subjective evaluation of patients. PHN was defined as a pain score >30% of the first pain score even after 4 weeks of developing skin rash7, and the occurrence was evaluated 4 weeks after hospitalization.
Age, sex, underlying diseases, time interval of skin lesions (<72 or ≥72 hours) and pain (<5 or ≥5 days) until treatment, involved dermatome, and incidence of PHN were compared between the vitamin C treatment group and the control group. Pain intensity at the given time interval was also compared between the two groups.
Statistical analyses were performed by using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). The pain scores of the vitamin C treatment and control groups were measured 9 times with respect to time.
Repeated-measures ANOVA was used to analyze and examine the changes in pain intensity with respect to time. A p-value <0.05 was considered statistically significant. Sex, underlying diseases, time interval of skin lesions and pain until treatment, involved dermatome, and incidence of PHN were compared between the two groups by using the Pearson's chi-square test. Age was compared between the two groups by using the t-test.
Out of 87 patients, 45 (51.7%) were in the vitamin C treatment group and 42 (48.3%) were in the control group. The mean age of the patients in the vitamin C treatment group was 59.02 years, and the sex distribution was 31 females (68.9%) and 14 males (31.3%). The mean age of the patients in the control group was 59.29 years, and the sex distribution was 22 females (52.4%) and 20 males (47.6%). No statistically significant difference was observed between the two groups (p>0.05), and the ratio of women was higher than that of men in both groups (Table 1).
In the vitamin C treatment group, the most common dermatome was the thoracic nerve (21 patients, 46.7%), followed by the trigeminal nerve (9 patients, 20.0%), cervical and sacral nerves (each with 6 patients, 13.3%), and lumbar nerve (3 patients, 6.7%). In the control group, the most common dermatome was also the thoracic nerve (19 patients, 45.2%), followed by the trigeminal nerve (11 patients, 26.2%), cervical nerve (6 patients, 14.3%), sacral nerve (5 patients, 11.9%), and lumbar nerve (1 patient, 2.4%). Involved dermatome was not statistically significant between the two groups (p>0.05; Table 1).
In the vitamin C treatment group, 18 patients (40.0%) had underlying diseases, whereas 27 patients (60.0%) did not have any underlying diseases. In the control group, 13 patients (31.0%) had underlying diseases, whereas 29 patients (69.0%) did not have any underlying diseases. No statistically significant difference was observed between the two groups (p>0.05; Table 1).
The period between developing pain and treatment of HZ was set to 5 days. A group of patients who received treatment before the fifth day and another group of patients who received treatment after the fifth day were compared with the patients in the vitamin C treatment and control groups. No statistically significant difference was observed between the two groups (p>0.05). However, the control group had more patients treated within 5 days of developing pain than the vitamin C treatment group (Table 1). In addition, the period between developing skin lesions and treatment was set to 72 hours, and we compared the vitamin C treatment and control groups in terms of before and after 72 hours. Although no statistically significant difference was observed between the two groups (p>0.05), the vitamin C treatment group had more patients treated within 72 hours (Table 1).
PHN occurred in 14 patients (31.1%) in the vitamin C treatment group and 24 patients (57.1%) in the control group. The incidence of PHN statistically significantly differed between the two groups (p<0.05; Table 1).
The pain decreased over time in both groups. In particular, the pain score measured on the eighth week in the vitamin C treatment group significantly differed from that in the control group (p=0.004; Table 2). The pain score was 1.0 for the vitamin C treatment group and lower than 2.01 for the control group. A statistically significant difference was found between the two groups even on the last week (p<0.001). The pain score for the vitamin C treatment group (0.64) was lower than that for the control group (1.98) by 1.34 points.
Changes in pain score with respect to time were statistically significant between the vitamin C treatment and control groups (Fig. 1). According to the results of the analysis that compared the effects on the control and vitamin C treatment groups for each time interval, pain score was initially higher in the vitamin C treatment group; but after the 2 weeks of follow up, the pain score for the vitamin C treatment group was lower than the control group. Generally, the pain for the control group was scored low in the early part but increased after the second week of follow up, whereas the pain score in the vitamin C treatment group continuously decreased.
We compared the difference in pain score by age, sex, time interval of pain and skin lesions until treatment, and underlying diseases with respect to time in the vitamin C treatment group (n=45). All of the analyses showed significant differences in pain score with respect to time in general (p<0.001). The patients were categorized by age of 60 years as the standard, and 22 patients (48.9%) were younger than 60 years and 51.1% were older than 60 years. No significant change in pain score with respect to time were observed between the two age groups (p=0.932; Fig. 2A). However, a significant difference in pain score with respect to time was observed between sexes (p=0.005; Fig. 2B). Pain score decreased in both male and female groups until measured on day 4 of admission, but the pain score for the females slightly increased on the fifth days unlike male. However, after the 2 weeks of follow up, the pain score for the females continuously decreased (from 2.0±0.4 to 1.2±0.3 to 0.9±0.2 to 0.5±0.1), exhibiting a lower pain score than that for males (from 2.4±0.5 to 2.1±0.5 to 1.2±0.3 to 0.9±0.2). No significant changes in pain score was observed according to time interval of pain and skin lesion until treatment and underlying diseases (p=0.422, 0.161, 0.707; Fig. 2C∼E).
HZ is a skin infection by the reactivation of the varicella zoster virus, which stays dormant after primary infection and develops vesicular skin eruptions unilaterally along the dermatome. PHN persists from several months to several years even after reduction in acute pain and skin rash from HZ, thus largely affecting the patient's quality of life1234. Ninty-six percentage of patients with HZ experience pain, of whom 42% complain of intense pain4 which is more severe than postoperative or labor pain15. The annual prevalence of HZ is 3.2∼4.2 cases per 1,000 people in the United States. HZ occurs in about 10 per 1,000 people older than 60 years, showing that the incidence of HZ increases with age6. In South Korea, it occurs in 10.4 cases per 1,000 people16. The annual incidence of HZ in South Korea had increased for the past 5 years16, and the burden of disease has also increased due to long-term treatment, compared to that in other countries17. The reason is that cell-mediated immunity plays an important role in the reactivation of the varicella zoster virus and the development of HZ, and it decreases with age15. Some reported that 10%∼30% of the population contracted HZ during their lifetime14, and PHN occurred in 18%∼33% of them, depending on the age of the patients and evaluation time11. Yawn et al.18 reported that PHN occurred in 18% of patients with HZ and it occurred in 33% of patients older than 79 years, demonstrating that the incidence of PHN increases with age.
PHN persists even with improvement in skin lesions, and it can be defined variously according to the following time points: 1 month, 3 months, 4 months, and 6 months after developing skin rash3. Moreover, PHN can also be defined as pain score of more than 3 points and persisting for 3 months after developing rash19. PHN is an intractable peripheral neuropathic pain and can be explained by mechanisms of disinhibition of pain transmission, central sensitization, reactive oxygen species, and neuroinflammation1220. Tricyclic antidepressant is regarded as the primary treatment for PHN, but in the recent years, gabapentin and 5% lidocaine patch are used as primary treatment options5. Opioids can be used when patients are resistant to other forms of treatment, and drugs can be chosen according to underlying diseases and patient preference5. A recent study reported that HZ vaccinations decreased the burdens of disease by 61%, incidence of HZ by 51%, and the incidence of PHN by 67%. Similarly, Zostavax Efficacy and Safety Trial studies reported that HZ vaccinations significantly decreased the incidence of HZ by 60% in patients aged 50∼59 years2. In recent studies, oxygen free radicals generated from peripheral inflammation sensitized nociceptors strongly react with noxious stimuli, as well as cause response even to simulation below the threshold. Peripheral sensitization not only causes pain directly but also by inducing central sensitization in the spinal cord21. Thus, oxygen free radicals are thought to play a role in the development and maintenance of PHN, and pain is anticipated to be reduced by injecting scavengers of oxygen free radicals1220.
Because vitamin C eliminates excess oxygen free radicals as a scavenger of oxygen free radicals, it is hypothesized to have protective effects on the nerve12. Vitamin C is an antioxidant that serves as a cofactor for many enzymes, and plays a role in the synthesis of collagen, neurotransmitter, and numerous neuropeptides. It also has important functions in wound healing, energy metabolism, and nervous system11. The high concentration of vitamin C around the immune cells and neurons explains the function of vitamin C11. Virus infection generates large amounts of oxygen free radicals, and because vitamin C is used to eliminate oxygen free radicals generated from infection, its concentration can decrease1122. And vitamin C deficiency can be observed in patients with viral infections822. Vitamin C concentrations were also low in patients with PHN1220. In a recent study, IV injection of high concentrated vitamin C was reported to alleviate acute pain and PHN12131420. Vitamin C reduces inflammation by production of antiviral cytokine and interferon and detoxification and neutralization of oxygen free radicals, and has direct antiviral effect22.
In early investigation, acute phase of HZ was treated using 7.5 g or 15 g dosage of vitamin C, while PHN was treated with 2.5 g of low-dosed vitamin C111213. The results of this study showed that the incidence of PHN statistically significantly was decrease in vitamin C treatment group. Unlike previous reports, no significant change in acute pain within 4 weeks of hospitalization was observed between the vitamin C treatment and control groups when pain score was compared according to time intervals. However, statistically significant differences were observed after the eighth week and continued thereafter. Consistent with previous studies, we found that low-dose of vitamin C was efficient in the treatment of PHN. As we carried out the study for inpatients treated with IV antiviral therapy, we consider that antiviral treatment may offset the effect of vitamin C. Moreover, changes in overall pain with respect to time showed statistically significant difference between the two groups, and pain was more effectively controlled in the vitamin C treatment group than in the control group. In the vitamin C treatment group, changes in the pain score over time by all variables without sex did not show statistically significant differences. The women showed significant decrease in pain score. Perhaps the more they are sensitive to pain at first, it is considered that they had been better in the treatment reaction.
The adverse effects reported in previous studies were minor such as lethargy/fatigue, local vein irritation, phlebitis, kindey stone, hemolysis and elevated blood glucose23. The most common of these side effects were lethargy and fatigue, vein irritation, and nausea and vomiting23. When patients have pre-existing renal insuffiency/failure or glucose 6-phosphate dehydrogenase deficiency, a history of oxalate nephrolithiasis or paroxysmal nocturnal hemoglobinuria that is known to predispose to vitamin C toxicity, IV vitamin C should not be administered23. However, angiodynia from IV injection due to high vitamin C concentration was found in 2 patients, who did not exhibit angiodynia when they were injected with vitamin C diluted with 250 ml of saline water.
Some limitations of this study were as follows: First, the base vitamin C concentration was not measured; thus, whether the patient had vitamin C deficiency or not was uncertain. Therefore, evaluation of the correlation between vitamin C deficiency and PHN was difficult. Second, pain intensity varied widely between the patients; thus, the objectivity of the VAS was questionable. Third, the vitamin C dosage for treatment of HZ varied111213 from 2.5 g, 5 g, 7.5 g, and 15 g, and no standardized intervals for the injections had been established. Fourth, recall bias existed for the patients who did not visit the hospital and were asked to describe their pain over the phone.
IV injection of vitamin C is used widely for fatigue, viral infection, influenza infection, and hepatitis23. Furthermore, it is used as a secondary treatment of HZ infection and has demonstrated its effects on acute pain and PHN. But further studies on various dosage, interval, and periods are necessary.
In this study, the results did not reflect a significant decrease in acute pain, unlike previous studies, but the treatment was effective in preventing PHN. Also, because of the significant changes in pain over time, we argue that this may be a safe treatment for prevention of PHN and pain from HZ without major side effects.
In conclusion, because acute pain and PHN from HZ significantly affects patient's quality of life, appropriate treatment is important. Various treatments have been introduced to date, but when conventional treatment is unresponsive or management is difficult, IV injection of vitamin C can be used as an effective treatment method to control pain from HZ.
Figures and Tables
Fig. 1
The pain score in the vitamin C treatment group and control group. HD: hospital date, W: week.
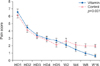
Fig. 2
The pain score change in vitamin C group. (A) In the age <60 and age ≥60 groups. (B) In the female and male groups. (C) Five days before and after pain. (D) Seventy-two hours within and over skin lesion. (E) In the underlying diseases. Means and standard errors are shown. p-value was calculated by repeated-measures analysis of variance (RM ANOVA). HD: hospital date, W: week.

Table 1
Baseline characteristics of the patients

Table 2
The changes in the severity of pain between vitamin C treatment group and control group

ACKNOWLEDGMENT
The present study was supported by grants from the Clinical Medicine Research Institute at Chosun University Hospital, 2013.
References
2. Song H, Lee J, Lee M, Choi WS, Choi JH, Lee MS, et al. Burden of illness, quality of life, and healthcare utilization among patients with herpes zoster in South Korea: a prospective clinical-epidemiological study. Int J Infect Dis. 2014; 20:23–30.

3. Schmader KE, Oxman MN. Varicella and herpes zoster. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 2383–2401.
4. Katz J, Cooper EM, Walther RR, Sweeney EW, Dworkin RH. Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis. 2004; 39:342–348.

5. Tyring SK. Management of herpes zoster and postherpetic neuralgia. J Am Acad Dermatol. 2007; 57:S136–S142.

6. Harpaz R, Ortega-Sanchez IR, Seward JF. Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC). Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008; 57:1–30. quiz CE2-CE4.
7. Falaki F, Nejat AH, Dalirsani Z. The effect of low-level laser therapy on trigeminal neuralgia: a review of literature. J Dent Res Dent Clin Dent Prospects. 2014; 8:1–5.
8. Jain SK, Pemberton PW, Smith A, McMahon RF, Burrows PC, Aboutwerat A, et al. Oxidative stress in chronic hepatitis C: not just a feature of late stage disease. J Hepatol. 2002; 36:805–811.

9. Terekhina NA, Petrovich IuA, Batueva RA, Sosnin DIu, Vesna VA. [Lacrimal and salivary antioxidants in viral infection]. Klin Lab Diagn. 1998; (1):13–15.
10. Chen JY, Chu CC, Lin YS, So EC, Shieh JP, Hu ML. Nutrient deficiencies as a risk factor in Taiwanese patients with postherpetic neuralgia. Br J Nutr. 2011; 106:700–707.

11. Schencking M, Vollbracht C, Weiss G, Lebert J, Biller A, Goyvaerts B, et al. Intravenous vitamin C in the treatment of shingles: results of a multicenter prospective cohort study. Med Sci Monit. 2012; 18:CR215–CR224.

12. Byun SH, Jeon Y. Administration of vitamin C in a patient with Herpes Zoster-a case report-. Korean J Pain. 2011; 24:108–111.

13. Schencking M, Sandholzer H, Frese T. Intravenous administration of vitamin C in the treatment of herpetic neuralgia: two case reports. Med Sci Monit. 2010; 16:CS58–CS61.
14. Peek DF, van Zundert J. The vitamin C controversy. Clin J Pain. 2010; 26:551–552. author reply 552-553.

16. Kim YJ, Lee CN, Lim CY, Jeon WS, Park YM. Population-based study of the epidemiology of herpes zoster in Korea. J Korean Med Sci. 2014; 29:1706–1710.

17. Roh NK, Park YM, Kang H, Choi GS, Kim BJ, Lee YW, et al. Awareness, knowledge, and vaccine acceptability of Herpes Zoster in Korea: a multicenter survey of 607 patients. Ann Dermatol. 2015; 27:531–538.

18. Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc. 2007; 82:1341–1349.

19. Kawai K, Rampakakis E, Tsai TF, Cheong HJ, Dhitavat J, Covarrubias AO, et al. Predictors of postherpetic neuralgia in patients with herpes zoster: a pooled analysis of prospective cohort studies from North and Latin America and Asia. Int J Infect Dis. 2015; 34:126–131.

20. Chen JY, Chang CY, Feng PH, Chu CC, So EC, Hu ML. Plasma vitamin C is lower in postherpetic neuralgia patients and administration of vitamin C reduces spontaneous pain but not brush-evoked pain. Clin J Pain. 2009; 25:562–569.

21. Chung JM. The role of reactive oxygen species (ROS) in persistent pain. Mol Interv. 2004; 4:248–250.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download