INTRODUCTION
Penile verrucous carcinoma is a rare, low-grade penile squamous cell carcinoma (SCC) exhibiting slow invasive growth. Regional lymph node metastasis is rare and distant metastasis has yet not been reported1. Penile verrucous carcinoma accounts for 5 to 24% of all penile malignancies and represents 5 to 16% of all penile SCCs2. In our present study, we analyzed 11 cases of penile verrucous carcinoma in our hospital between the period of 2002 and 2009, accounting for 15% of the hospitalized patients with penile carcinoma at the same time.
CASE REPORT
We retrospectively analyzed the data of 11 patients with penile verrucous carcinoma. The patients were in age range from 49 to 85 years, with a mean age of 62 years. All the patients were presented with exophytic, papillary, caulifower-like or verrucose lesions involving the penis with the greatest dimension ranging from 2 to 10 cm. The tumors were located at glans in 7 cases, invaded the coronoid sulcus in 3 cases and invaded the shaft of the penis in 1 case. All the patients were presented with tumors from a time span of 3 months to 8 years before surgery. Physical examination and ultrasonography revealed enlarged inguinal lymph nodes in 8 cases. Distant metastasis was excluded on the basis of chest radiography and computed tomography of the abdomen.
A total of 10 cases underwent preoperative biopsy. Whereas, 7 cases underwent partial penectomy and the other 3 cases with the tumor confined exclusively to the glans underwent local excision. During the procedure, the standard surgical margins of 2 cm for partial penectomy were followed and the surgical margins of 0.5~1 cm for the local excision were adopted according to the size of tumor. The patient without any biopsy underwent circumcision due to phimosis accompanied by recurrent infection. During the operation, a neoplasm with 2 cm of the greatest dimension invading the coronoid sulcus was found and a local tumor excision was simultaneously performed. The postoperative histopathologic examination described the lesion as verrucous carcinoma with the positive surgical margins and the patient had to undergo partial penectomy. The lymph nodes biopsies were simultaneously performed in 5 cases. At the end of two months of follow up, it was found that that the enlarged lymph nodes were still present in the other 3 cases and they subsequently underwent modified bilateral inguinal lymphadenectomy.
The microscopic examination of all the tumors revealed the presence of well-differentiated papillary constitutions with acanthosis and hyperkeratosis extending into the underlying stroma with broad bases and pushing borders. The microscopic examination of lymph nodes by biopsy and excision revealed only inflammation without any metastatic tumor cells.
All the patients were disease free at the end of 6 to 60 months (mean of 36 months) of follow-up. No recurrence or metastasis was detected later on. The clinical characteristics of patients and the operative data are listed in Table 1.
DISCUSSION
Verrucous carcinoma is an uncommon, exophytic, low-grade and well-differentiated variant of SCC with slow invasive growth and without any distant metastasis. Its presence was first described in 1948 by Ackerman in the oral cavity3. Since then it has been also described at other sites, including the anus, female genitalia, penis, soles and at any location on the skin4. Verrucous carcinoma is also known by several other names, e.g., giant condyloma acuminatum or Buschke-Lowenstein tumor5. However, some researchers consider giant condyloma acuminatume or Buschke Loewenstein tumor as a distinct disease which only represents an intermediate condition between condyloma acuminatum and verrucous carcinoma6,7. Currently, the common opinion is that both the lesions are similar and should not be separated into two different entities8.
The specific etiologic factors of penile verrucous carcinoma remain unclear. Predisposing factors include lack of circumcision, poor hygiene, phimosis, tight prepuce and chronic infection. However, no systematic case series have been studied so far9,10. It has been reported that penile SCC can arise in males circumcised at birth. Thus, the preventive effect of newborn circumcision on the development of penile SCC is still unclear10. Kanik et al.11 once described penile verrucous carcinoma in a 37-year-old white man who had been circumcised in infancy without any predisposing penile anatomic abnormalities. In our study, the series includes 6 cases with redundant prepuce and the others with phimosis who did not undergo newborn circumcision. Additionally, as per the earlier studies, human papillomavirus (HPV) infection, especially the low-risk types, HPV-6 and HPV-11, play a vital role in the pathogenesis of the tumor12. However, other studies have not found a significant association between penile verrucous carcinoma and HPV1,4,13.
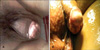
Clinically, penile verrucous carcinoma arises anywhere on the penis, mostly on the glans or foreskin as a gradually enlarging, exophytic, papillary, caulifower-like or verrucose mass which may be foul smelling and sometimes ulcerated, with fstulae that release a purulent discharge. Shaft involvement is less frequent in such a condition. In rare cases, it may resemble a penile horn (Fig. 1). Microscopic histopathologic appearance should be carefully identified so as to differentiate penile verrucous carcinoma from condyloma accuminatum and penile SCC. Microscopically, penile verrucous carcinoma is a very well differentiated papillary neoplasm with acanthosis and hyperkeratosis (Fig. 2). It is classified as Ta stage according to the TNM staging system14.
Surgical excision, sparing as much of the penis as possible is the usual treatment for penile verrucous carcinoma. Local excision and partial penectomy are most commonly used15. Hatzichristou et al.8 suggested that glansectomy is an appropri-ate treatment for patients with penile verrucous carcinoma confined exclusively to the glans penis and that more radical techniques (e.g., partial or total penectomy) are reserved as second-line treatments for cases of local recurrence. Due to the lack of recognition, only 3 cases in our series that should be treated by local excision or glansectomy due to the presence of a small mass confined to the glans penis underwent overtreatment. Regardless of any operative strategies, the negative surgical margins must be ensured. Accordingly, in our series, the standard surgical margins of 2 cm for partial penectomy were followed and the surgical margins of 0.5~1 cm for the local excision were adopted according to the size of the tumor. Additionally, the cases in our series must undergo a second partial penectomy since the pathological diagnosis indicated positive margins after the first circumcision. The presence and the extent of metastasis to the inguinal region are the most important prognostic factors for survival in patients with squamous penile cancer15. To date, no patients with penile verrucous carcinoma had suffered from regional lymph node metastasis4,10. In our series, the histologic examination of lymph node biopsies in 5 cases and bilateral inguinal lymphadenectomy in 3 cases indicated lymph node metastasis to be negative. With the follow up of mean 36 months, no evidence of lymph node metastasis was found. Additionally, lymphadenectomy was found to be associated with a significant risk of morbidity. So, we suggest that lymphadenectomy is not necessary in case of the patients with the final diagnosis of penile verrucous carcinoma by histologic examination.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download