Abstract
Nevus sebaceous (NS) is a type of classical nevus or congenital malformation that is often present at birth and commonly involves the scalp or face. The lesion usually presents as a linear, yellow, hairless, and verrucous plaque. It has been well-established that several benign and malignant tumors can develop from the NS; however, there have been no reports about ectopic fat cells in the dermis, and cornoid lamella arising from the NS. We report a case of NS on the scalp with accompanying unusual histopathologic findings.
Nevus sebaceous (NS) is a congenital hamartomatous disorder that commonly involves the scalp or face. The lesion usually presents as a linear, yellow, hairless, and verrucous plaque, characteristically evolves, and changes in morphology with time1,2. It has been well-established that various types of appendageal tumors develop secondarily within lesions of NS.
A 78-year-old female patient presented with a 3×5 cm solitary, yellow, verrucous plaque on the scalp. On histopathologic examination, syringocystadenoma papilliferum and a trichoblastoma-like lesion arising from the NS were observed. In addition, there were fat cells in upper dermis and cornoid lamella. These findings arising from NS have been rarely reported in the dermatologic literature. We report a case of NS with unusual accompanying findings and give a brief review of the relevant literature.
A 78-year-old female presented to the department of dermatology for evaluation of a scalp lesion. Since birth, she had a solitary 3×5 cm yellow, verrucous plaque on the scalp (Fig. 1). She had no family history of similar lesions and had no previous relevant medical history, including history of local trauma or previous surgeries to that site. She only complained of mild tenderness in the area of the lesion. The lesion was completely excised for diagnosis and treatment.
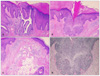
On histopathologic examination, the epidermis showed hyperkeratosis, irregular acanthosis, and papillomatosis. Incompletely differentiated hair structures, which are typical features of nevus sebaceous, also were observed in the dermis (Fig. 2). On the basis of clinical and histopathologic findings, the lesion was diagnosed as a NS.
In addition, there was cystic invagination extending downward from the epidermis within the lesion. Papillary projections, lined by two rows of cells, extended into the lumina in the lower portion of the invagination (Fig. 3A). From these findings, the cystic invagination was diagnosed as syringocystadenoma papilliferum. Moreover, basaloid epithelial proliferations, trichoblastoma-like lesions that showed PAS negative arising from the NS were observed (Figs. 3B, D). There was a parakeratotic column overlying the trichoblastoma like-lesion, resembling cornoid lamella of porokeratosis (Fig. 3B). In addition, there were fat cells in the upper dermis, which were unusual findings in NS (Fig. 3C). The lesion was removed completely, and there were no signs of recurrence.
It has been well-established that NS is a common site for the development of secondary neoplasms, usually benign but sometimes malignant. The most commonly associated appendageal tumors to develop secondarily within NS have been thought to be syringocystadenoma papilliferum and trichoblastoma3,4. Syringocystadenoma papilliferum has been found in 8% to 19% of NS1. Basaloid epithelial proliferations have been clinically evident in 5% to 7% of NS5. In the current case, syringocystadenoma papilliferum and trichoblastoma-like lesions arising from the NS were observed. Other relatively common secondary neoplasms include nodular hidradenoma, syringoma, sebaceous epithelioma, chondroid syringoma, and trichilemmoma6. Recent studies have revealed that the development of malignant tumors like basal cell carcinoma in NS is very rare. Among the malignant tumors associated with NS, basal cell carcinoma was thought to be the most common; however, most reported basal cell carcinomas in NS are now believed to be trichoblastomas8. In a study of 596 cases of NS by Cribier et al., basal cell carcinoma was seen in only 0.8% of cases3.
Multiple neoplasms may occasionally arise within the same NS7. In a study of 155 cases of NS by Jaqueti et al., there were eight cases in which two neoplasms developed in the same NS4. Moreover, there have been some reports of three or more tumors within same NS7. In this case, two kinds of neoplasms, syringocystadenoma papIlliferum, and a trichoblastoma-like lesion occurred simultaneously. There were some unique findings in this case. There were ectopic fat tissues in the upper dermis. Further, conditions like nevus lipomatosus superficialis, cutaneous nodules of focal dermal hypoplasia, or skin tags demonstrated ectopic fat tissue on histopathologic examination. However, we could not find any reports related to NS associated with ectopic fat tissue. There was one paper that may help explain this phenomenon8. In that report, the presence of fat cells within long-standing intradermal melanocytic nevi represented an involutionary phenomenon rather than an association of a nevus lipomatosus with melanocytic nevus8. In addition, Ahn et al.9 reported that fatty changes in long-standing neurofibromas may be related to senescent change in older patients. Therefore, we believe that the presence of fat cells within long-standing NS may be an involutionary phenomenon rather than an association with other conditions. Prophylactic excision of NS is warranted for cosmesis or for the prevention of secondary malignancies in early age and therefore, involutionary phenomenon has not been well-reported in the elderly. More study is required to confirm involutionary changes associated with aging.
Another unique finding was cornoid lamella, which possessed homogeneous horny cells and pyknotic nuclei within the parakeratotic column. Though cornoid lamella is a characteristic finding of porokeratosis, it has also been found in a variety of other conditions, especially solar keratosis and verruca vulgaris10. Cornoid lamella associated with NS has rarely been reported. The presence of abnormal basaloid proliferation located at the base of the parakeratotic column may explain the porokeratosis.
In summary, this case was a classic NS, which contained typical secondary neoplasms, syringocystadenoma papilliferum, and a trichoblastoma-like lesion. In addition, there were some unique findings, fat tissues in the dermis, and cornoid lamella that arose from the NS. These findings have rarely been reported in the dermatologic literature, and further studies will be needed to confirm the possibility that these changes were associated with the aging process of NS.
Figures and Tables
Fig. 2
Histopathology of the yellow, verrucous plaque. Hyperkeratosis, irregular acanthosis, and papillomatosis were present in the epidermis. Incompletely differentiated hair structures were in the dermis (H&E, ×12.5).

Fig. 3
(A) Cystic invagination extended downward from the epidermis (H&E, ×40), which was diagnosed as a syringocystadenoma papilliferum. (B) There was a parakeratotic column overlying the trichoblastoma like-lesion, resembling the cornoid lamella of porokeratosis (H&E, ×40). (C) There were fat cells in upper dermis (H&E, ×40). (D) The basaloid epithelial proliferation showed PAS negative finding (PAS, ×100).
References
1. Mehregan AH, Pinkus H. Life history of organoid nevi. Special reference to nevus sebaceous of Jadassohn. Arch Dermatol. 1965. 91:574–588.
2. Baker BB, Imber RJ, Templer JW. Nevus sebaceous of Jadassohn. Arch Otolaryngol. 1975. 101:515–516.

3. Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000. 42:263–268.
4. Jaqueti G, Requena L, Sánchez Yus E. Trichoblastoma is the most common neoplasm developed in nevus sebaceus of Jadassohn: a clinicopathologic study of a series of 155 cases. Am J Dermatopathol. 2000. 22:108–118.

5. Jones EW, Heyl T. Naevus sebaceus. A report of 140 cases with special regard to the development of secondary malignant tumours. Br J Dermatol. 1970. 82:99–117.
6. Stavrianeas NG, Katoulis AC, Stratigeas NP, Karagianni IN, Patertou-Stavrianea M, Varelzidis AG. Development of multiple tumors in a sebaceous nevus of Jadassohn. Dermatology. 1997. 195:155–158.

7. Nakai K, Yoneda K, Moriue J, Moriue T, Matsuoka Y, Kubota Y. Sebaceoma, trichoblastoma and syringocystadenoma papilliferum arising within a nevus sebaceous. J Dermatol. 2008. 35:365–367.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download