This article has been
cited by other articles in ScienceCentral.
Dear Editor:
Porokeratosis of Mibelli (PM) is one type of porokeratosis (PK) that is characterized clinically by hyperkeratotic papules or plaques surrounded by a thread-like elevated border that expands centrifugally
1. Although many treatments such as topical steroids, topical 5-fluorouracil and imiquimod creams, and cryotherapy have been attempted to treat PK, the results have often been disappointing.
A 65-year-old male patient presented with a large erythematous scaly plaque with a raised border on his left buttock for 20 years (
Fig. 1A). After a skin biopsy, the lesion was histologically diagnosed as PM (
Fig. 1B). We initially attempted to treat the lesion using cryotherapy, topical steroids, and topical imiquimod cream but the lesion did not decrease in size and the lesion became erosive after treatments. So we considered performing methyl aminolevulinate- photodynamic therapy (MAL-PDT). Prior to applying topical MAL cream (Metvix®; PhotoCure ASA, Oslo, Norway) on the lesion, we removed the scales on the surface using forceps and a blade to facilitate penetration of the cream and red light. After a three-hour incubation period for the MAL to be fully absorbed, we washed off the cream and confirmed the absorption of MAL through a Wood lamp (
Fig. 1C). The lesion was then irradiated with a beam of red light (Aktilite® CL 128 lamp; Photocure ASA) at a wavelength of 630 nm, total light dose 37 J/cm
2 without any analgesic prophylaxis. During and after irradiation of red light, the patient felt pain but said it was tolerable. A month after the treatment, the elevated border disappeared and the size of the lesion decreased with no adverse effect (
Fig. 1D). Hence, we performed a second MAL-PDT, and noticed three months after the treatment that the size of the lesion was more decreased and the margin became more blurred (
Fig. 1E). We concluded that MAL-PDT was effective for the lesion and suggested additional treatments to the patient, but he was lost to follow-up. We received the patient's consent form about publishing all photographic materials.
PDT is approved for the treatment of actinic keratosis (AK), basal cell carcinoma, and Bowen disease
2. And there have been several attempts to use MAL-PDT for the treatment of PK (
Table 1)
2. In choosing a photosensitizer, Ko et al.
3 noted that MAL-PDT was similar to 5-aminolevulinic acid–PDT in terms of long-term efficacy, recurrence rate and cosmetic outcomes but the former is less painful and therefore suitable for the treatment of multiple AK lesions. So we considered MAL to be more appropriate for the treatment of the large lesion in this case.
Treating PK is usually unnecessary but it is necessary if the lesion is problematic, cosmetically unacceptable, or potentially malignant
4. And because the lesion has improved considerably after only two sessions of treatment without any serious adverse effect, we would like to report this case. Further studies are needed to determine whether MAL-PDT can be used as a treatment for PK and to establish its therapeutic usage.
Figures and Tables
Fig. 1
(A) Erythematous scaly plaque with a raised border on the left buttock. (B) Column of parakeratosis arising from an invagination of the epidermis (H&E, ×40). (C) Wood lamp examination after an incubation period of 3 hours during the first methyl aminolevulinate-photodynamic therapy (MAL-PDT). The fluorescence was emitted by the porokeratotic lesion pretreated with methyl aminolevulinate. (D) One month after the first treatment. The second MAL-PDT treatment was performed on the same day. (E) The size of the lesion decreased, and the thread-like elevated border became blurred 3 months after the second treatment.
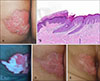
Table 1
Clinical features of patients of porokeratosis treated with PDT in dermatologic journal

ACKNOWLEDGMENT
This study was supported by research funds from Dong-A University.
References
1. O'Regan GM, Irvine AD. Porokeratosis. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 563–568.
2. Gutiérrez Paredes E, Bella Navarro R, Montesinos Villaescusa E, Jordá Cuevas E. Porokeratosis of Mibelli: a new indication for photodynamic therapy? Actas Dermosifiliogr. 2013; 104:259–261.


4. Sertznig P, von Felbert V, Megahed M. Porokeratosis: present concepts. J Eur Acad Dermatol Venereol. 2012; 26:404–412.






 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download