Dear Editor:
Onychomycosis is a common fungal infection of the nails, approximately 2% to 13% of the general population is affected by onychomycosis1. There are several therapeutic modalities, among which oral antifungal agents are considered the gold standard. While these agents are generally well tolerated, they carry a treatment failure risk of approximately 25% to 40% primarily due to poor patient compliance and drug interactions. There are also several contraindications for oral antifungal drugs including liver disease and congestive cardiac failure. Apart from these medical causes, some patients are reluctant to take oral antifungal drugs due to concerns and misconceptions about the risks associated with systematic antifungals. Thus, there is a growing need for new therapeutic options that are safe and beneficial to a wider population without contraindications. Recently, a number of different devices have been developed, most of which utilize a 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser3. Although not included in recent guidelines2, several studies have shown that 1064 nm Nd:YAG lasers are effective in treating onychomycosis, while other studies have reported conflicting results456. The Food and Drug Administration has also approved the 1064 nm Nd:YAG laser for the indication of increasing clear nails in patients with onychomycosis temporarily, but not as a definitive cure. For this reason, it is important to identify patients who will respond to 1064 nm Nd:YAG laser therapy, although more research is needed on this topic. In this retrospective study, we evaluated the clinical factors that influence the clinical outcomes of 1064 nm Nd:YAG laser treatment for onychomycosis.
Data from onychomycosis patients treated by 1064 nm Nd:YAG laser treatment between February 2014 to September 2016 were collected. The diagnosis of onychomycosis was made based on microscopic examination after treatment with 20% potassium hydroxide. In cases of ambiguous results on microscopic examination, fungal culture was performed using Sabouraud's dextrose agar. Patients taking oral antifungal medications within one year of the study as well as those who used other topical antifungal agents for onychomycosis were excluded from the study.
We collected data on patient age, sex, and information about infected nails such as location, clinical type, and severity of onychomycosis evaluated by the onychomycosis severity index (OSI) score7. Before laser treatment, nails thicker than 2 mm were mechanically debrided using a nail grinder. All patients were treated using a 1064 nm Nd:YAG laser (Pinpointe Footlaser; Pinpointe USA Inc., Chico, CA, USA) at the following settings: pulse energy, 200 mJ; pulse width, 0.1 ms; spot size, 1.5 mm; frequency; 30 Hz; and temperature, 40℃~60℃. For each treatment session the laser beam was first moved in a spiral fashion to cover the entire nail plate followed by a 2-minute pause, and this process was then repeated twice. Laser treatments were scheduled at 4-week (±10 days) intervals, and a total 4 to 6 sessions of laser treatments were performed. Outcome assessment was performed 4 weeks after the final laser therapy session. Photographs were taken in a standardized format using a digital camera. (Canon EOS-40D; Canon Corp., Tokyo, Japan) OSI score was evaluated by three dermatologists, including the therapist. The favorable response rate was defined as the percentage of patients whose OSI score decreased by more than 75% compared to their initial result. All statistical analyses were performed using SPSS software (version 20.0; IBM Co., Armonk, NY, USA). The outcome of the statistical analysis was deemed significant when the p-value was below 0.05.
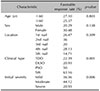
A total of 174 infected nails were included in this study. Table 1 shows the baseline demographic characteristics of all enrolled nails. Overall, the OSI score was significantly decreased after 4 to 6 laser treatments sessions (p<0.0001). Table 2 demonstrates different therapeutic results according to various clinical factors. No significant differences in favorable response rate were observed according to age, sex, and location of the onychomycosis, while clinical type and initial disease severity affected the therapeutic response significantly. The superficial white type showed statistically better clinical outcomes than the total dystrophic or distal and lateral subungual type (p=0.001, p=0.000, respectively). The moderately severe group was associated with more favorable treatment outcomes compared to the severe group (44.12% vs. 20.93%, p=0.006). In terms of safety, there were no sustained side effects other than a temporary heating sensation.
The therapeutic mechanism responsible for the efficacy of laser therapy for onychomycosis has not yet been elucidated, although several hypotheses have been proposed458. Considering that the current clinical data remain controversial, further studies will be needed to properly determine how best to identify those patients who will have a better response to laser treatment. This study is meaningful in that it is the first paper to deal with this topic in earnest.
The results of this study showed that superficial white type and moderately severe onychomycosis are associated with a better therapeutic response to 1064 nm Nd:YAG laser treatment. Patients with initially mild onychomycosis also had a better outcome compared to those with severe onychomycosis, but the difference was not statistically significant. We also found that age, sex, and location of onychomycosis had no effect on clinical outcome. This was consistent with the results of Kim et al.5 who showed that the response of total dystrophic type onychomycosis is poor and that the location of the infected nail does not influence therapeutic outcomes. On the other hand, our results are not consistent with those described by Gupta and Paquet4 who reported that patients younger than 60 years of age have better outcomes and that initial severity does not affect therapeutic outcomes.
The limitations of this study included the use of a relatively small number of subjects. In addition, some factors known to be the poor prognostic factor were not included, including whether the patient is immunosuppressed, has poor peripheral circulation, or suffers from poorly controlled diabetes mellitus. It is also known that nail infection by non-dermatophyte mold or yeast is generally considered to have a worse prognosis, an aspect that was not addressed in our study.
In conclusion, we found that patients with superficial white type and moderate initially severe onychomycosis have a relatively good therapeutic response to 1064 nm Nd:YAG laser treatment.
ACKNOWLEDGMENT
This study was approved by the Institutional Review Board of the Kyung Hee University Medical Center (IRB no. KHUHMDIRB 2017-03-047).
References
1. Scher RK, Rich P, Pariser D, Elewski B. The epidemiology, etiology, and pathophysiology of onychomycosis. Semin Cutan Med Surg. 2013; 32:2 Suppl 1. S2–S4.

2. Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M. British Association of Dermatologists' guidelines for the management of onychomycosis 2014. Br J Dermatol. 2014; 171:937–958.

3. Francuzik W, Fritz K, Salavastru C. Laser therapies for onychomycosis - critical evaluation of methods and effectiveness. J Eur Acad Dermatol Venereol. 2016; 30:936–942.

4. Gupta AK, Paquet M. A retrospective chart review of the clinical efficacy of Nd:YAG 1064-nm laser for toenail onychomycosis. J Dermatolog Treat. 2015; 26:376–378.

5. Kim TI, Shin MK, Jeong KH, Suh DH, Lee SJ, Oh IH, et al. A randomised comparative study of 1064 nm Neodymium-doped yttrium aluminium garnet (Nd:YAG) laser and topical antifungal treatment of onychomycosis. Mycoses. 2016; 59:803–810.

6. Karsai S, Jäger M, Oesterhelt A, Weiss C, Schneider SW, Jünger M, et al. Treating onychomycosis with the short-pulsed 1064-nm-Nd:YAG laser: results of a prospective randomized controlled trial. J Eur Acad Dermatol Venereol. 2017; 31:175–180.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download