Abstract
Background
Atopic dermatitis (AD) is related to a deficiency of delta-6-desaturase, an enzyme responsible for converting linoleic acid to gamma-linolenic acid (GLA). Evening primrose oil (EPO) as a source of GLA has been of interest in the management of AD.
Objective
The aim of this randomized, double-blinded, placebo-controlled clinical study is to evaluate the efficacy and safety of EPO in Korean patients with AD.
Methods
Fifty mild AD patients with an Eczema Area Severity Index (EASI) score of 10 or less were enrolled and randomly divided into two groups. The first group received an oval unmarked capsule containing 450 mg of EPO (40 mg of GLA) per capsule, while placebo capsules identical in appearance and containing 450 mg of soybean oil were given to the other group. Treatment continued for a period of four months. EASI scores, transepidermal water loss (TEWL), and skin hydration were evaluated in all the AD patients at the baseline, and in months 1, 2, 3, and 4 of the study.
Results
At the end of month 4, the patients of the EPO group showed a significant improvement in the EASI score (p=0.040), whereas the patients of the placebo group did not. There was a significant difference in the EASI score between the EPO and placebo groups (p=0.010). Although not statistically significant, the TEWL and skin hydration also slightly improved in the EPO patients group.
Atopic dermatitis (AD) is a chronic, recurrent, and inflammatory skin disease characterized by dry skin, itch, and erythema as well as increase in the transepidermal water loss (TEWL)12. AD is multifactorial and has complicated immunological abnormal responses, including damage to the epidermal barrier, genetic factors, and environmental causes. Seemingly, many parts of the pathophysiological mechanism interact with each other to cause and exacerbate AD3.
Some researchers have suggested that AD may be related to the abnormal metabolism of essential fatty acid, especially the abnormality in the production of gamma-linolenic acid (GLA)456. In some AD patient groups, the functional deficiency of delta-6 desaturase was discussed as a factor of AD478. Delta-6 desaturase converts linoleic acid (LA) to GLA, which is then metabolized into dihomogamma-linolenic acid (DGLA)8. The functional deficiency of delta-6 desaturase has been found to cause an increase in the LA level and a decrease in GLA, DGLA, arachidonic acid, and prostaglandin E1 (PGE1) in patients with AD456. The deficiency of PGE1 can lead to immune dysregualation and the dominance of inflammatory PGE2 and PGF2, thereby causing AD9.
Evening primrose oil (EPO) is a natural source of LA and GLA. The intake of GLA contained in EPO is presumed to cause an anti-inflammatory response as the blood concentrations of GLA and DGLA increase4. Studies conducted by supplementing GLA to humans and rodents showed a selective increase of anti-inflammatory PGE1, but not inflammatory PGE28. Many studies have also shown a beneficial effect of EPO in AD10, but some studies have shown different results11. Although EPO is one of the adjuvant therapeutic agents listed in the Treatment Guideline of Korean Atopic Dermatitis12 published by the Korean Atopic Dermatitis Association, the effect of EPO on Korean patients with AD has not been sufficiently investigated. In addition, no report has ever been published about a well-designed, randomized, double-blinded, placebo-controlled study. Therefore, a randomized, double-blinded, placebo-controlled study was conducted to evaluate the efficacy and safety of EPO on Korean patients with AD. EPO or a placebo was administered to mild AD patients for 4 months, and the changes in the values including Eczema Area Severity Index (EASI), TEWL, and skin hydration, were measured.
This study was conducted for four months as a randomized, double-blinded, placebo-controlled clinical study. Among the outpatients who visited the Department of Dermatology at the Hallym University Medical Center for two years from August 2014 to July 2016, male and female patients who were diagnosed with mild AD according to the Diagnostic Criteria of Hanifin and Rajka13 and showed an EASI14 score equal to or lower than 10 were enrolled in the present study. Those who had another skin disease in addition to AD, showed an infectious finding, and had a systemic disease or an uncontrolled chronic disease were excluded. The present study was approved by the Institutional Review Board (IRB no. 2014-09-129) at the Hallym University Medical Center, and written consents were received from the patients or their guardians. There was no important changes of methods after trial commencement.
The patients were allocated to two groups using a computerized randomization scheme that were not disclosed to the observers. (1) The first group received unmarked oval 735 mg capsules containing 450 mg of EPO (40 mg of GLA) per capsule (Dalim, Seoul, Korea). (2) The placebo control group received placebo capsules that were identical in appearance, but contained 450 mg of soybean oil per capsule. For the randomization of the study drug group and the placebo group, randomization codes were given to the study products so that the clinical investigators and the subjects were unaware of the products in the double-blind study. The dose was four capsules per day for the patients between the ages of 2 and 12, and eight capsules per day for the others. The maximum allowable dose was provided to all the patients to avoid the effect of various doses on the response. During the study period, the patients were prohibited from taking phototherapy, a topocal immunosuppressant, a systemic immunosuppressant, a topical steroid, a systemic corticosteroid, or any other drugs. A washout period of one week was given before the treatment with regard to a topical steroid, a topical immunosuppressant, and a systemic antihistamine, and four weeks with regard to a systemic immunosuppressant, a systemic corticosteroid, and phototherapy. The patients of both the experimental group and the control group were recommended to use a moisturizer. We had patients use Atobarrier® lotion (Amorepacific Corp., Seoul, Korea) as the moisturizer. This lotion contains ceramide, cholesterol, and free fatty acids. We educated the patients to apply the amount of two fingers tip unit to one palm-sized lesion twice a day.
The drug administration and adverse effect evaluations were performed for all the patients. The EASI score, TEWL, skin hydration, and visual analogue scale (VAS) for pruritus were also evaluated in months 0, 1, 2, 3, and 4. Blood sampling for measuring blood immunoglobulin E (IgE) was performed in months 0 and 4. The severity of AD was evaluated by two dermatologists by using the EASI score14, and the mean values were calculated. The TEWL (g/h/m2) was measured by using VapoMeter® (Delfin Inc., Kuopio, Finland) and the skin hydration (arbitrary unit) was measured by using MoistureMeterSC Compact® (Delfin Inc.). The measurement devices were put on the skin at the lesions on both forearms and cheeks and kept vertical to the skin surface based on the recommendations of the manufacturers. The measurement was also performed three times, within two minutes in each time, to record the mean values. All measurements were conducted in a room that was not climate controlled. The room temperature and humidity were relatively stable (20℃~24℃ and 40%~60% relative humidity). Subjects were prohibited from washing for at least an hour before measurement and took a break for over 30 minutes in the same room. For the subjective itchy feeling felt by the patients, the intensity of the itch feeling was evaluated in the VAS from 0 to 10 points. The primary outcome measure was the EASI score. Secondary outcome measure were TEWL, skin hydration, VAS score, and adverse effects.
All the data were expressed as “mean±standard deviation.” Student's t-test was performed to compare the demographical and clinical characteristics between the two groups. The changes in the EASI score, TEWL, skin hydration, VAS for pruritus, and IgE was tested by performing Student's t-test and by using repeated-measures ANOVA. A p-value less than 0.05 was determined to be significant after the statistical test. All the statistical analyses were performed by using IBM SPSS Statistics 24.0 (IBM Co., Armonk, NY, USA).
A total of 69 mild AD patients were enrolled and randomized into either the control group (14 males and 17 females) or the EPO group (20 males and 18 females). Six patients in the control group and 13 patients in the EPO group dropped out due to follow up loss. No patient dropped out because the disease worsened. Finally, a total of 50 mild AD patients from the ages of 2 to 24 (26 males and 24 females) completed the present clinical study. Twenty-five patients (13 males and 12 females) were randomly allocated to the EPO group, and 25 patients (11 males and 14 females) to the control group. The mean age of the patients was 9.2±7.4 years, and the mean EASI score at the beginning of the study was 4.60±1.22. Table 1 shows the demographical characteristics and the initial measurement values of the EPO group and the control group. No significant difference was found in the mean age, EASI score, TEWL, skin hydration, and IgE measurement value of the patients between the EPO group and the control group (Table 1).
After supplementing GLA, the clinical improvement was compared between the EPO group and the control group. The mean EASI score was significantly different between the experimental group and the control group in month 4 (p=0.010). At months 1, 2, 3, there was no statistical difference in EASI scores between the two groups (p=0.348, 0.252, 0.195). The changes in the EASI score were greater in the experimental group than in the control group. In month 4, the mean EASI score was lower than the initial value by 1.09 times in the control group, and by 1.67 times in the EPO group. The mean EASI score in the experimental group administered with EPO gradually decreased from 4.69±1.63, 3.73±1.44, 3.23±1.10, 3.13± 0.95, and 2.80±0.87 in months 0, 1, 2, 3, and 4, respectively. The difference in the EASI score between the beginning of the study and month 4 was significant in the experimental group (p=0.040) (Fig. 1). The EASI score in the control group was 4.50±0.86, 4.57±0.97, 4.15±1.08, 3.97±0.80, and 4.14±0.92 in months 0, 1, 2, 3, and 4, respectively. No significant difference was found in any of the time points in comparison with the value at the beginning of the study (Fig. 1). The difference in EASI Score was statistically significant (p=0.002) at month 4 between two groups under the age of 12 years when it was divided based on age. On the other hand, at age over 12 years, the difference in EASI score was not statistically significant at month 4 between the two groups (p=0.481). The difference between the baseline and month 4 was statistically significant (p=0.001) in the EPO group for ages 12 and under. However, the placebo group had no statistical significance, regardless of age.
The changes in TEWL were compared on month 4 between the experimental group and the control group to the TEWL value at the beginning of the study (Fig. 2). Although no significant difference was found between the experimental group and the control group, the TEWL values at the forearms (experimental group vs. control group, −3.05±8.26 vs. −1.60±7.10; p=0.714) and the cheeks (experimental group vs. control group, −1.63±4.81 vs. −0.44±2.17; p=0.714) decreased more in the experimental group than in the control group in month 4.
With reference to the skin hydration value at the beginning of the study, the changes in the skin hydration in month 4 were compared between the experimental group and the control group (Fig. 3). Similarly to TEWL, no significant changes were found in the skin hydration value between the experimental group and the control group. However, the improvement in the skin hydration at the forearms (experimental group vs. control group, 6.57±11.94 vs. 3.03±9.06; p=0.470) was more in the experimental group than in the control group in month 4. But, there was no significant difference at the cheeks (experimental group vs. control group, 2.76±6.13 vs. 2.30±6.57; p=0.920).
The subjective itch feeling felt by patients, measured in VAS, was 4.3±1.1, 4.1±1.4, 4.2±1.5, 4.1±1.4, and 3.8±1.1 in months 0, 1, 2, 3, and 4, respectively, in the experimental group. This indicates that the score decreased by about 0.5 points in four months (p=0.343), but the subjective itch feeling felt by patients in the control group was 4.5±1.5, 4.7±1.6, 4.4±1.3, 4.2±1.2, and 4.3±1.5 in months 0, 1, 2, 3, and 4, respectively, indicating that the score decreased by about 0.2 points in four months (p=0.859) (Fig. 4A). No significant difference was found between the experimental group and the control group in the subjective itch feeling measured in month 4 (experimental group vs. control group, 3.8±1.1 vs. 4.3±1.5; p=0.714).
The blood IgE concentration decreased from 298.85±58.21 (IU/ml) at the beginning of the study to 264.65±40.86 (IU/ml) in month 4 in the experimental group (p=0.920), and from 291.09±59.78 (IU/ml) at the beginning of the study to 279.02±54.76 (IU/ml) in month 4 in the control group (p=0.899) (Fig. 4B). No significant difference was found between the experimental group and the control group in the IgE concentration measured in month 4 (experimental group vs. control group, 291.09±59.78 vs. 279.02±54.76; p=0.944).
Evening promise, a plant from the Onagraceae family, is called this because it only blooms at night, and the evening promise seed oil contains a large amount of LA as well as GLA, which is an unsaturated essential fatty acid15. Evening promise was used as a popular folk remedy after being introduced to Europe in the 17th century9. Since the high content of GLA in the EPO became known in the 1930s, EPO has been used as a raw material for medicine and supplementary health food. GLA was firstly extracted from evening promise seeds, and is also contained in borage oil, black currant oil, and hampseed oil916.
AD may be related to a mild genetic abnormality in the essential fatty acid metabolism. Studies conducted in the 1930s to 1950s revealed that a lack of omega-6 essential fatty acids can cause an inflammatory skin state in both animals and humans. Studies conducted in the 2000s verified that a lack of LA is not present in the blood of AD patients. Instead, the LA concentration was high in the blood, breast milk, and adipose tissue of the patients with AD, but the concentration of the LA metabolites was substantially low. This finding suggests that the conversion of LA to GLA decreased4.
GLA, a C18-three double bonds (18:3) omega-6 unsaturated fatty acid, is synthesized from LA by the action of delta-6-desaturase, the transforming enzyme17. GLA is rapidly converted in the body to DGLA, which is the precursor of Prostaglandin H1 (PGH1) that produces anti-inflammatory substances, PGE1, and thromboxane A1 (TXA1)18. PEG1 has anti-inflammatory, anti-coagulative, and vasodilator functions, and TXA1 regulates the pro-inflammatory characteristics of thromboxane A2 (TAX2)9. DGLA may also be converted by the action of delta-5-desaturase to arachidonic acid (20:4, n-6) as a precursor of PGE2, TXA2, and leukotriene B4 (LTB4)19. In contrast to other eicosanoids, DGLA is unable to directly produce leukotriene, but may inhibit the production of pro-inflammatory leukotriene from arachidonic acid20. Previous study has shown that in AD patients, a defect was found in the production of delta-6-desaturase that catalyzes the conversion of LA to GLA, DGLA, and arachidonic acid21. When GLA is supplemented to AD patients through EPO, the GLA may bypass delata-6-desaturase, the rate-limiting enzyme, and directly enter the LA metabolic pathway, thereby gradually recovering the anti-inflammatory PEG1 that is lacking in the body.
On the basis of the hypothesis, the clinical improving effect of EPO on the treatment of mild AD was verified in the present study. The EASI score of the experimental group administered with EPO was gradually decreased from month 1, showing a significantly difference decrease in the EASI score in comparison with the control group. Although not significantly different, TEWL showed a greater tendency to improvement in the experimental group than in the control group. The skin hydration value also improved in a similar pattern on the forearm, but not on the cheek. No significant difference was found in the VAS for pruritus and IgE in the EPO group and the control group. None of the two groups showed an adverse effect related to the drug.
Since it was found that deficiency of GLA may contribute to the factors of AD, many studies regarding the effect of GLA supplementation on AD patients have been conducted, but the results have been inconsistent. Recently, the Cochrane Review performed a systematic review of borage oil and EPO and concluded that the intake of these mixtures is not an effective therapy for AD11. However, a detailed review of randomized studies verifying the effect of EPO makes it difficult to definitely judge the presence of an effect16. Bamford et al.22 conducted a double-blinded cross-over study with 154 patients with AD and found that EPO did not significantly improve erythema, scale, abrasion, lichenification, or their severity in comparison with the placebo. Another study conducted by Berth-Jones and Graham-Brown23 with 123 subjects showed that the disease symptoms did not significantly improve in the EPO groups in comparison with the placebo group. Both studies finally concluded that EPO containing GLA does not have a significant effect in comparison with a placebo.
On the contrary, Bordoni et al.24 investigated 24 patients with AD and found that EPO significantly improved the symptoms of AD in comparison with a placebo. Similarly, Schalin-Karrila25 conducted a study with 25 patients with AD and reported that the severity and degree of inflammation improved in both the EPO group and the placebo group, but there was significantly more improvement in the EPO group. EPO has also shown significant improvement in skin dryness, pruritus, and range of lesions. Humphreys et al.26 conducted a study with 58 patients with moderate to severe AD and showed that erythema and surface damage significantly improved more in the EPO than in the placebo group. Finally, a study conducted with 25 AD patients showed that all the measurement indicators, including range of lesions, severity, pruritus, and skin dryness, improved significantly more in the EPO group than in the placebo group9.
Two studies were conducted to verify the effect of GLA on Korean AD patients. Yoon et al.27 conducted a study with 14 adult AD patients and reported that the range of skin lesions and the degree of pruritus significantly decreased in all the patients administered with EPO. In another study conducted with 40 children with AD, where the patients were divided into a 160 mg EPO supplementation group and a 320 mg EPO supplementation group, the EASI score improved and the blood LA level significantly increased in both groups. This change was more distinctive in the high-dose group, suggesting a dose-dependent effect28. These previous studies conducted with Koreans showed a beneficial effect of EPO in AD. The present study is meaningful in the sense that the effect was verified through a well-designed, randomized, double-blinded, placebo-controlled study, in contrast to the previous studies.
In the present study, a measure of improvement in the EASI score, TEWL, and skin hydration was also found in the placebo group. However, this observation was neither consistent nor gradual, but inconsistent. The irregular improvement found in the control group may have been because of the effect of a local moisturizer, an inherent placebo response, and the natural catamnesis of AD.
Despite the Cochrane Review11, the beneficial effect of EPO on AD may not be completely denied. Many confounding factors, such as racial factors and combined use of a corticosteroid, have been revealed in recent studies, which may explain the inconsistent patient response to EPO that has been reported until now10. Therefore, the results could be made more appropriately consistent by deleting confounding factors such as age and race. In this study, the effect was better shown when the subjects were less than 12 years old. Recent studies have shown the unique complexity of the fatty acid metabolism and immunological responses in AD that are more complicated than previously reported. This may help to identify groups that are unresponsive to EPO and establish subgroups that may acquire continuous benefits from EPO. The almost complete absence of adverse effects and the expectancy of the unidentified and potential efficacies of EPO suggest that EPO deserves more studies. There were no studies adequate to compare the therapeutic effect of evening primrose oil on Korean AD patients. In particular, has been no well-designed randomized, placebo-controlled study in Korea. Therefore, it is meaningful that this study was the first attempt to do this in Korea. The significance of the present study is that the improvement of the clinical symptoms was verified in Korean patients with mild AD who were administered EPO through this randomized, double-blinded, placebo-controlled clinical study. However, there are some limitations in this study. AD usually shows seasonal improvement and aggravation. Patients in our work were being studied in different seasons. Moreover, information about the season was not collected. Finally, this study was conducted in a single country at single institution; therefore, the results cannot be generalized. Further studies, including standardization of the EPO administration method, may contribute to the treatment of AD.
The present study was conducted as a randomized, double-blinded, placebo-controlled clinical study with 50 patients with mild AD to investigate the therapeutic effect and safety of EPO. The results of the present study showed that there was a significantly improved EASI score in the group supplemented with EPO than in the placebo group. The TEWL and the skin hydration value also showed a tendency of improvement after the administration of EPO. No adverse effect was found in relation to EPO. These results may support the basis of using EPO as an adjuvant therapeutic agent for Korean patients with mild AD.
Figures and Tables
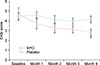 | Fig. 1Changes in Eczema Area Severity Index (EASI) score from baseline after intake of evening primrose oil (EPO) or placebo. The EPO group showed significant improvements in EASI score after 4 months (p=0.040). There was a significant difference between the EPO and placebo group after 4 months (*p=0.010). |
 | Fig. 2Changes in transepidermal water loss (TEWL) at the forearm (A) and cheek (B) from baseline after intake of evening primrose oil (EPO) or placebo. |
 | Fig. 3Changes in skin hydration of the forearm (A) and cheek (B) from baseline after intake of evening primrose oil (EPO) or placebo. a.u.: arbitrary unit. |
 | Fig. 4Changes in pruritus (A) and IgE (B) from baseline after intake of evening primrose oil (EPO) or placebo. VAS: visual analogue scale, IgE: immunoglobulin E. |
Table 1
Patient demographics

ACKNOWLEDGMENT
This study was supported by grants of the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT & Future Planning (NRF-2017 R1A2B4006252, 2018R1C1B6007998), Korea Healthcare technology R&D project, funded by Ministry of Health & Welfare, Republic of Korea (HI17C0597), and the Hallym University Research Fund (HURF-2017-35, HURF-2017-52, HURF-2017-83).
References
2. Cork MJ, Danby SG, Vasilopoulos Y, Hadgraft J, Lane ME, Moustafa M, et al. Epidermal barrier dysfunction in atopic dermatitis. J Invest Dermatol. 2009; 129:1892–1908.

3. McPherson T. Current Understanding in Pathogenesis of Atopic Dermatitis. Indian J Dermatol. 2016; 61:649–655.

4. Horrobin DF. Essential fatty acid metabolism and its modification in atopic eczema. Am J Clin Nutr. 2000; 71:1 Suppl. 367S–372S.

6. Manku MS, Horrobin DF, Morse N, Kyte V, Jenkins K, Wright S, et al. Reduced levels of prostaglandin precursors in the blood of atopic patients: defective delta-6-desaturase function as a biochemical basis for atopy. Prostaglandins Leukot Med. 1982; 9:615–628.

7. Kerscher MJ, Korting HC. Treatment of atopic eczema with evening primrose oil: rationale and clinical results. Clin Investig. 1992; 70:167–171.

8. Simon D, Eng PA, Borelli S, Kägi R, Zimmermann C, Zahner C, et al. Gamma-linolenic acid levels correlate with clinical efficacy of evening primrose oil in patients with atopic dermatitis. Adv Ther. 2014; 31:180–188.

9. Senapati S, Banerjee S, Gangopadhyay DN. Evening primrose oil is effective in atopic dermatitis: a randomized placebo-controlled trial. Indian J Dermatol Venereol Leprol. 2008; 74:447–452.

10. Morse NL, Clough PM. A meta-analysis of randomized, placebo-controlled clinical trials of Efamol evening primrose oil in atopic eczema. Where do we go from here in light of more recent discoveries? Curr Pharm Biotechnol. 2006; 7:503–524.

11. Bamford JT, Ray S, Musekiwa A, van Gool C, Humphreys R, Ernst E. Oral evening primrose oil and borage oil for eczema. Cochrane Database Syst Rev. 2013; (4):CD004416.

12. Lee JH, Kim KH, Kim MN, Kim JW, Ro YS, Park YL, et al. Report from ADRG: the treatment guideline of Korean atopic dermatitis. Korean J Dermatol. 2006; 44:907–913.
13. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venerol (Stockh). 1980; 92:44–47.
14. Hanifin JM, Thurston M, Omoto M, Cherill R, Tofte SJ, Graeber M. The eczema area and severity index (EASI): assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp Dermatol. 2001; 10:11–18.

16. Vieira BL, Lim NR, Lohman ME, Lio PA. Complementary and Alternative Medicine for Atopic Dermatitis: An Evidence-Based Review. Am J Clin Dermatol. 2016; 17:557–581.

17. Muggli R. Systemic evening primrose oil improves the biophysical skin parameters of healthy adults. Int J Cosmet Sci. 2005; 27:243–249.

18. Wertz PW, Swartzendruber DC, Abraham W, Madison KC, Downing DT. Essential fatty acids and epidermal integrity. Arch Dermatol. 1987; 123:1381–1384.

19. McCusker MM, Grant-Kels JM. Healing fats of the skin: the structural and immunologic roles of the omega-6 and omega-3 fatty acids. Clin Dermatol. 2010; 28:440–451.

20. Belch JJ, Hill A. Evening primrose oil and borage oil in rheumatologic conditions. Am J Clin Nutr. 2000; 71:1 Suppl. 352S–356S.

21. Manku MS, Horrobin DF, Morse NL, Wright S, Burton JL. Essential fatty acids in the plasma phospholipids of patients with atopic eczema. Br J Dermatol. 1984; 110:643–648.

22. Bamford JT, Gibson RW, Renier CM. Atopic eczema unresponsive to evening primrose oil (linoleic and gammalinolenic acids). J Am Acad Dermatol. 1985; 13:959–965.

23. Berth-Jones J, Graham-Brown RA. Placebo-controlled trial of essential fatty acid supplementation in atopic dermatitis. Lancet. 1993; 341:1557–1560.

24. Bordoni A, Biagi PL, Masi M, Ricci G, Fanelli C, Patrizi A, et al. Evening primrose oil (Efamol) in the treatment of children with atopic eczema. Drugs Exp Clin Res. 1988; 14:291–297.
25. Schalin-Karrila M, Mattila L, Jansen CT, Uotila P. Evening primrose oil in the treatment of atopic eczema: effect on clinical status, plasma phospholipid fatty acids and circulating blood prostaglandins. Br J Dermatol. 1987; 117:11–19.

26. Humphreys F, Symons JA, Brown HK, Duff GW, Hunter JAA. The effects of gamolenic acid on adult atopic eczema and premenstrual exacerbation of eczema. Eur J Dermatol. 1994; 4:598–603.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download